Abstract
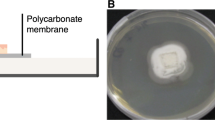
Children in community bodies like kindergartens are predisposed to suffer from impetigo. To consider important measures for infection prevention, direct and indirect transmission routes of pathogens must be revealed. Therefore, we studied the role of skin and fabrics in the spread of the impetigo pathogen Staphylococcus aureus and the strain Streptococcus equi (surrogate to Streptococcus pyogenes) in order to assess infection transfer in realistic scenarios. The transmission of test strains was studied with standardized fabric-skin models using a technical artificial skin and fabrics of different fiber types commonly occurring in German kindergartens. In synthetic pus, both test strains persisted on artificial skin and fabrics for at least 4 h. Friction enhanced transfer, depending on the fiber type or fabric construction. In a skin-to-skin setup, the total transfer was higher than via fabrics and no decrease in the transmission rates from donor to recipients could be observed after successive direct skin contacts. Children in kindergartens may be at risk of transmission for impetigo pathogens, especially via direct skin contact, but also by the joint use of fabrics, like towels or handicraft materials. Fabric-skin models used in this study enable further insight into the transmission factors for skin infections on the basis of a practical approach.




Similar content being viewed by others
References
Wannamaker LW (1970) Differences between streptococcal infections of the throat and of the skin. I. N Engl J Med 282(1):23–31. doi:10.1056/NEJM197001012820106
Empinotti JC, Uyeda H, Ruaro RT, Galhardo AP, Bonatto DC (2012) Pyodermitis. An Bras Dermatol 87(2):277–284
Kristensen JK (1991) Scabies and Pyoderma in Lilongwe, Malawi. Prevalence and seasonal fluctuation. Int J Dermatol 30(10):699–702
Loffeld A, Davies P, Lewis A, Moss C (2005) Seasonal occurrence of impetigo: a retrospective 8-year review (1996–2003). Clin Exp Dermatol 30(5):512–514. doi:10.1111/j.1365-2230.2005.01847.x
Kakar N, Kumar V, Mehta G, Sharma RC, Koranne RV (1999) Clinico-bacteriological study of pyodermas in children. J Dermatol 26(5):288–293
Feldmeier H, Singh Chhatwal G, Guerra H (2005) Pyoderma, group A streptococci and parasitic skin diseases—a dangerous relationship. Trop Med Int Health 10(8):713–716. doi:10.1111/j.1365-3156.2005.01457.x
Crocker HR (1881) On the contagium of impetigo contagiosa. Lancet 117(3012):821
Parker MT, Tomlinson AJ, Williams RE (1955) Impetigo contagiosa; the association of certain types of Staphylococcus aureus and of Streptococcus pyogenes with superficial skin infections. J Hyg (Lond) 53(4):458–473
Brown J, Shriner DL, Schwartz RA, Janniger CK (2003) Impetigo: an update. Int J Dermatol 42(4):251–255
Barrow GI (1955) Clinical and bacteriological aspects of impetigo contagiosa. J Hyg (Lond) 53(4):495–508
Darmstadt GL, Lane AT (1994) Impetigo: an overview. Pediatr Dermatol 11(4):293–303
Cruickshank JG, Lightfoot NF, Sugars KH, Colman G, Simmons MD, Tolliday J, Oakley EH (1982) A large outbreak of streptococcal pyoderma in a military training establishment. J Hyg (Lond) 89(1):9–21
Ludlam H, Cookson B (1986) Scrum kidney: epidemic pyoderma caused by a nephritogenic Streptococcus pyogenes in a rugby team. Lancet 2(8502):331–333
Levy JA (2004) Common bacterial dermatoses: protecting competitive athletes. Phys Sportsmed 32(6):33–39. doi:10.3810/psm.2004.06.380
Sheehan HL, Girdwood Fergusson A (1943) Impetigo aetiology and treatment. Lancet 241(6244):547–550
Chiller K, Selkin BA, Murakawa GJ (2001) Skin microflora and bacterial infections of the skin. J Investig Dermatol Symp Proc 6:170–174. doi:10.1046/j.0022-202x.2001.00043.x
Sattar SA, Springthorpe S, Mani S, Gallant M, Nair RC, Scott E, Kain J (2001) Transfer of bacteria from fabrics to hands and other fabrics: development and application of a quantitative method using Staphylococcus aureus as a model. J Appl Microbiol 90(6):962–970
Bloomfield S, Exner M, Fara GM, Scott EA (2008) Prevention of the spread of infection—the need for a family-centred approach to hygiene promotion. Euro Surveill 13(22):1–4
Waller AS, Paillot R, Timoney JF (2011) Streptococcus equi: a pathogen restricted to one host. J Med Microbiol 60(Pt 9):1231–1240. doi:10.1099/jmm.0.028233-0
Burkhardt F (1992) Mikrobiologische Diagnostik, vol 1. Auflage, Stuttgart
von Gorup-Besànez EF (1862) Lehrbuch der physiologischen Chemie. Druck und Verlag von Friedrich Vieweg und Sohn, Braunschweig
König C, Simmen HP, Blaser J (1998) Bacterial concentrations in pus and infected peritoneal fluid—implications for bactericidal activity of antibiotics. J Antimicrob Chemother 42(2):227–232
ISO 105-E04:2013 Textiles—Tests for colour fastness—Part E04: Colour fastness to perspiration; German version EN ISO 105-E04:2013
DIN 53923:1978-01 Testing of textiles; determination of water absorption of textile fabrics
Hammer TR, Berner-Dannenmann N, Hoefer D (2013) Quantitative and sensory evaluation of malodour retention of fibre types by use of artificial skin, sweat and radiolabelled isovaleric acid. Flavour Fragr J 28(4):238–244. doi:10.1002/ffj.3134
Gwaltney JM Jr, Moskalski PB, Hendley JO (1978) Hand-to-hand transmission of rhinovirus colds. Ann Intern Med 88(4):463–467
Ghareeb PA, Bourlai T, Dutton W, McClellan WT (2013) Reducing pathogen transmission in a hospital setting. Handshake versus fist bump: a pilot study. J Hosp Infect 85(4):321–323. doi:10.1016/j.jhin.2013.08.010
Lingaas E, Fagernes M (2009) Development of a method to measure bacterial transfer from hands. J Hosp Infect 72(1):43–49. doi:10.1016/j.jhin.2009.01.022
Mbithi JN, Springthorpe VS, Boulet JR, Sattar SA (1992) Survival of hepatitis A virus on human hands and its transfer on contact with animate and inanimate surfaces. J Clin Microbiol 30(4):757–763
Jabbar U, Leischner J, Kasper D, Gerber R, Sambol SP, Parada JP, Johnson S, Gerding DN (2010) Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol 31(6):565–570. doi:10.1086/652772
Mela S, Whitworth DE (2014) The fist bump: a more hygienic alternative to the handshake. Am J Infect Control 42(8):916–917. doi:10.1016/j.ajic.2014.04.011
Meadow JF, Bateman AC, Herkert KM, O’Connor TK, Green JL (2013) Significant changes in the skin microbiome mediated by the sport of roller derby. Peer J 1:e53. doi:10.7717/peerj.53
Lax S, Smith DP, Hampton-Marcell J, Owens SM, Handley KM, Scott NM, Gibbons SM, Larsen P, Shogan BD, Weiss S, Metcalf JL, Ursell LK, Vázquez-Baeza Y, Van Treuren W, Hasan NA, Gibson MK, Colwell R, Dantas G, Knight R, Gilbert JA (2014) Longitudinal analysis of microbial interaction between humans and the indoor environment. Science 345(6200):1048–1052. doi:10.1126/science.1254529
Martínez-Bastidas T, Castro-del Campo N, Mena KD, Castro-del Campo N, León-Félix J, Gerba CP, Chaidez C (2014) Detection of pathogenic micro-organisms on children’s hands and toys during play. J Appl Microbiol 116(6):1668–1675. doi:10.1111/jam.12473
Mygind O, Rønne T, Søe AL, Henrik Wachmann C, Ricks P (2003) Comparative intervention study among Danish daycare children: the effect on illness of time spent outdoors. Scand J Public Health 31(6):439–443. doi:10.1080/14034940310005349
Scott E, Bloomfield SF (1990) The survival and transfer of microbial contamination via cloths, hands and utensils. J Appl Bacteriol 68(3):271–278
Fritz SA, Epplin EK, Garbutt J, Storch GA (2009) Skin infection in children colonized with community-associated methicillin-resistant Staphylococcus aureus. J Infect 59(6):394–401. doi:10.1016/j.jinf.2009.09.001
Gerhardts A, Hammer TR, Balluff C, Mucha H, Hoefer D (2012) A model of the transmission of micro-organisms in a public setting and its correlation to pathogen infection risks. J Appl Microbiol 112(3):614–621. doi:10.1111/j.1365-2672.2012.05234.x
Barker J, Jones MV (2005) The potential spread of infection caused by aerosol contamination of surfaces after flushing a domestic toilet. J Appl Microbiol 99(2):339–347. doi:10.1111/j.1365-2672.2005.02610.x
Hambraeus A (1973) Transfer of Staphylococcus aureus via nurses’ uniforms. J Hyg (Lond) 71(4):799–814
Marples RR, Towers AG (1979) A laboratory model for the investigation of contact transfer of micro-organisms. J Hyg (Lond) 82(2):237–248
Mackintosh CA, Hoffman PN (1984) An extended model for transfer of micro-organisms via the hands: differences between organisms and the effect of alcohol disinfection. J Hyg (Lond) 92(3):345–355
Takashima M, Shirai F, Sageshima M, Ikeda N, Okamoto Y, Dohi Y (2004) Distinctive bacteria-binding property of cloth materials. Am J Infect Control 32(1):27–30. doi:10.1016/j.ajic.2003.05.003
Teufel L, Pipal A, Schuster KC, Staudinger T, Redl B (2010) Material-dependent growth of human skin bacteria on textiles investigated using challenge tests and DNA genotyping. J Appl Microbiol 108(2):450–461. doi:10.1111/j.1365-2672.2009.04434.x
Cotner S, Navrotski E, Sewera L, Snyder V, Richter E (2010) Diversity of culturable bacteria on natural vs artificial fabrics. Internet J Microbiol 8(2)
Hsieh YL, Merry J (1986) The adherence of Staphylococcus aureus, Staphylococcus epidermidis and Escherichia coli on cotton, polyester and their blends. J Appl Bacteriol 60(6):535–544
Hsieh Y-L, Timm DA, Merry J (1987) Bacterial adherence on fabrics by a radioisotope labeling method. Text Res J 57(1):20–28
Bajpai V, Dey A, Ghosh S, Bajpai S, Jha MK (2011) Quantification of bacterial adherence on different textile fabrics. Int Biodeterior Biodegrad 65(8):1169–1174
St Sauver J, Khurana M, Kao A, Foxman B (1998) Hygienic practices and acute respiratory illness in family and group day care homes. Public Health Rep 113(6):544–551
Conflict of interest
The authors declare that they have no conflict of interest.
Compliance of ethics
This article does not contain any studies with human participants performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gerhardts, A., Henze, S.V., Bockmühl, D. et al. Fabric-skin models to assess infection transfer for impetigo contagiosa in a kindergarten scenario. Eur J Clin Microbiol Infect Dis 34, 1153–1160 (2015). https://doi.org/10.1007/s10096-015-2336-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2336-7