Abstract
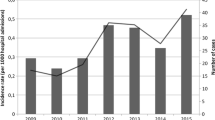
This is the first Portuguese multicenter observational and descriptive study that provides insights on the species distribution and susceptibility profiles of yeast isolates from fungemia episodes. Ten district hospitals across Portugal contributed by collecting yeast isolates from blood cultures and answering questionnaires concerning patients’ data during a 12-month period. Molecular identification of cryptic species of Candida parapsilosis and C. glabrata complex was performed. The susceptibility profile of each isolate, considering eight of the most often used antifungals, was determined. Both Clinical and Laboratory Standards Institute (CLSI) and European Committee on Antimicrobial Susceptibility Testing (EUCAST) protocols were applied. The incidence of 240 episodes of fungemia was 0.88/1,000 admissions. Fifteen different species were found, with C. albicans (40 %) being the most prevalent, followed by C. parapsilosis (23 %) and C. glabrata (13 %). Most isolates were recovered from patients admitted to surgical wards or intensive care units, with 57 % being males and 32 % aged between 41 and 60 years. For both the CLSI and EUCAST protocols, the overall susceptibility rates ranged from 74 to 97 % for echinocandins and from 84 to 98 % for azoles. Important resistance rate discrepancies between protocols were observed in C. albicans and C. glabrata for echinocandins and in C. parapsilosis and C. tropicalis for azoles. Death associated with fungemia occurred in 25 % of the cases, with more than half of C. glabrata infections being fatal. The great number of Candida non-albicans is noteworthy despite a relatively low antifungal resistance rate. Studies like this are essential in order to improve empirical treatment guidelines.
Similar content being viewed by others
References
Arendrup MC (2010) Epidemiology of invasive candidiasis. Curr Opin Crit Care 16:445–452
Pfaller MA, Diekema DJ, Gibbs DL, Newell VA, Ellis D, Tullio V, Rodloff A, Fu W, Ling TA; Global Antifungal Surveillance Group (2010) Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: a 10.5-year analysis of susceptibilities of Candida species to fluconazole and voriconazole as determined by CLSI standardized disk diffusion. J Clin Microbiol 48:1366–1377
Fortún J, Martín-Dávila P, Gómez-García de la Pedrosa E, Pintado V, Cobo J, Fresco G, Meije Y, Ros L, Alvarez ME, Luengo J, Agundez M, Belso A, Sánchez-Sousa A, Loza E, Moreno S (2012) Emerging trends in candidemia: a higher incidence but a similar outcome. J Infect 65:64–70
Yapar N (2014) Epidemiology and risk factors for invasive candidiasis. Ther Clin Risk Manag 10:95–105
Playford EG, Nimmo GR, Tilse M, Sorrell TC (2010) Increasing incidence of candidaemia: long-term epidemiological trends, Queensland, Australia, 1999–2008. J Hosp Infect 76:46–51
Clinical and Laboratory Standards Institute (CLSI) (2008) Reference method for broth dilution antifungal susceptibility testing of yeasts; Approved standard—Third edition. CLSI document M27-A3. CLSI, Wayne, PA
Clinical and Laboratory Standards Institute (CLSI) (2012) Reference method for broth dilution antifungal susceptibility testing of yeasts; Fourth informational supplement. CLSI document M27-S4. CLSI, Wayne, PA
Rodríguez-Tudela JL, Arendrup MC, Cuenca-Estrella M, Donnelly JP, Lass-Flörl C (2010) EUCAST breakpoints for antifungals. Drug News Perspect 23:93–97
Pfaller MA, Andes D, Diekema DJ, Espinel-Ingroff A, Sheehan D; CLSI Subcommittee for Antifungal Susceptibility Testing (2010) Wild-type MIC distributions, epidemiological cutoff values and species-specific clinical breakpoints for fluconazole and Candida: time for harmonization of CLSI and EUCAST broth microdilution methods. Drug Resist Updat 13:180–195
Romeo O, Scordino F, Pernice I, Lo Passo C, Criseo G (2009) A multiplex PCR protocol for rapid identification of Candida glabrata and its phylogenetically related species Candida nivariensis and Candida bracarensis. J Microbiol Methods 79(1):117–120
Tavanti A, Davidson AD, Gow NA, Maiden MC, Odds FC (2005) Candida orthopsilosis and Candida metapsilosis spp. nov. to replace Candida parapsilosis groups II and III. J Clin Microbiol 43:284–292
Espinel-Ingroff A, Arendrup MC, Pfaller MA, Bonfietti LX, Bustamante B, Canton E, Chryssanthou E, Cuenca-Estrella M, Dannaoui E, Fothergill A, Fuller J, Gaustad P, Gonzalez GM, Guarro J, Lass-Flörl C, Lockhart SR, Meis JF, Moore CB, Ostrosky-Zeichner L, Pelaez T, Pukinskas SR, St-Germain G, Szeszs MW, Turnidge J (2013) Interlaboratory variability of caspofungin MICs for Candida spp. using CLSI and EUCAST methods: should the clinical laboratory be testing this agent? Antimicrob Agents Chemother 57:5836–5842
Pfaller MA, Espinel-Ingroff A, Canton E, Castanheira M, Cuenca-Estrella M, Diekema DJ, Fothergill A, Fuller J, Ghannoum M, Jones RN, Lockhart SR, Martin-Mazuelos E, Melhem MS, Ostrosky-Zeichner L, Pappas P, Pelaez T, Peman J, Rex J, Szeszs MW (2012) Wild-type MIC distributions and epidemiological cutoff values for amphotericin B, flucytosine, and itraconazole and Candida spp. as determined by CLSI broth microdilution. J Clin Microbiol 50:2040–2046
Tortorano AM, Prigitano A, Lazzarini C, Passera M, Deiana ML, Cavinato S, De Luca C, Grancini A, Lo Cascio G, Ossi C, Sala E, Montagna MT (2013) A 1-year prospective survey of candidemia in Italy and changing epidemiology over one decade. Infection 41:655–662
Pemán J, Cantón E, Quindós G, Eraso E, Alcoba J, Guinea J, Merino P, Ruiz-Pérez-de-Pipaon MT, Pérez-del-Molino L, Linares-Sicilia MJ, Marco F, García J, Roselló EM, Gómez-G-de-la-Pedrosa E, Borrell N, Porras A, Yagüe G; FUNGEMYCA Study Group (2012) Epidemiology, species distribution and in vitro antifungal susceptibility of fungaemia in a Spanish multicentre prospective survey. J Antimicrob Chemother 67:1181–1187
Colombo AL, Nucci M, Park BJ, Nouér SA, Arthington-Skaggs B, da Matta DA, Warnock D, Morgan J; Brazilian Network Candidemia Study (2006) Epidemiology of candidemia in Brazil: a nationwide sentinel surveillance of candidemia in eleven medical centers. J Clin Microbiol 44:2816–2823
Costa-de-Oliveira S, Pina-Vaz C, Mendonça D, Gonçalves Rodrigues A (2008) A first Portuguese epidemiological survey of fungaemia in a university hospital. Eur J Clin Microbiol Infect Dis 27:365–374
Asmundsdottir LR, Erlendsdottir H, Gottfredsson M (2013) Nationwide study of candidemia, antifungal use, and antifungal drug resistance in Iceland, 2000 to 2011. J Clin Microbiol 51(3):841–848
Das I, Nightingale P, Patel M, Jumaa P (2011) Epidemiology, clinical characteristics, and outcome of candidemia: experience in a tertiary referral center in the UK. Int J Infect Dis 15:e759–e763
Wu Z, Liu Y, Feng X, Liu Y, Wang S, Zhu X, Chen Q, Pan S (2014) Candidemia: incidence rates, type of species, and risk factors at a tertiary care academic hospital in China. Int J Infect Dis 22:4–8
Quindós G (2014) Epidemiology of candidaemia and invasive candidiasis. A changing face. Rev Iberoam Micol 31:42–48
Chalmers C, Gaur S, Chew J, Wright T, Kumar A, Mathur S, Wan WY, Gould IM, Leanord A, Bal AM (2011) Epidemiology and management of candidaemia—a retrospective, multicentre study in five hospitals in the UK. Mycoses 54:e795–e800
Arendrup MC, Dzajic E, Jensen RH, Johansen HK, Kjaeldgaard P, Knudsen JD, Kristensen L, Leitz C, Lemming LE, Nielsen L, Olesen B, Rosenvinge FS, Røder BL, Schønheyder HC (2013) Epidemiological changes with potential implication for antifungal prescription recommendations for fungaemia: data from a nationwide fungaemia surveillance programme. Clin Microbiol Infect 19:E343–E353
Ericsson J, Chryssanthou E, Klingspor L, Johansson AG, Ljungman P, Svensson E, Sjölin J (2013) Candidaemia in Sweden: a nationwide prospective observational survey. Clin Microbiol Infect 19:E218–E221
Bonfietti LX, Szeszs MW, Chang MR, Martins MA, Pukinskas SR, Nunes MO, Pereira GH, Paniago AM, Purisco SU, Melhem MS (2012) Ten-year study of species distribution and antifungal susceptibilities of Candida bloodstream isolates at a Brazilian tertiary hospital. Mycopathologia 174:389–396
Tosun I, Akyuz Z, Guler NC, Gulmez D, Bayramoglu G, Kaklikkaya N, Arikan-Akdagli S, Aydin F (2013) Distribution, virulence attributes and antifungal susceptibility patterns of Candida parapsilosis complex strains isolated from clinical samples. Med Mycol 51:483–492
Esposto MC, Prigitano A, Romeo O, Criseo G, Trovato L, Tullio V, Fadda ME, Tortorano AM; FIMUA Working Group (2013) Looking for Candida nivariensis and C. bracarensis among a large Italian collection of C. glabrata isolates: results of the FIMUA working group. Mycoses 56:394–396
Pfaller MA, Espinel-Ingroff A, Boyken L, Hollis RJ, Kroeger J, Messer SA, Tendolkar S, Diekema DJ (2011) Comparison of the broth microdilution (BMD) method of the European Committee on Antimicrobial Susceptibility Testing with the 24-hour CLSI BMD method for testing susceptibility of Candida species to fluconazole, posaconazole, and voriconazole by use of epidemiological cutoff values. J Clin Microbiol 49:845–850
Pfaller MA, Castanheira M, Messer SA, Rhomberg PR, Jones RN (2014) Comparison of EUCAST and CLSI broth microdilution methods for the susceptibility testing of 10 systemically active antifungal agents when tested against Candida spp. Diagn Microbiol Infect Dis 79:198–204
Acknowledgments
We would like to thank all the participants whom have contributed with isolates and clinical data: J. Melo Cristino (Centro Hospitalar de Lisboa Norte); V. Lopes, J. Teixeira, and H. Ramos (Centro Hospitalar do Porto); C. Toscano and T. Marques (Centro Hospitalar de Lisboa Ocidental); Z. Videira, A. Almeida, E. Tiza, and M. Silveira (Instituto Português de Oncologia de Lisboa); G. Gonçalves and A. Estrada (Hospital de São Marcos, Braga); A. C. Lameiras and M. A. Guimarães (Instituto Português de Oncologia do Porto); H. Oliveira and M. H. Pereira (Centro Hospitalar de Coimbra); E. Ramalheira and S. Ferreira (Hospital Infante Dom Pedro, Aveiro). We would also like to acknowledge the collaboration of “Grupo de Estudos de Micologia Médica” (GEMM).
This work was supported by Fundação Ciência e Tecnologia (FCT, project PTDC/DTP-EPI/1660/2012 “Surveillance of the emergent Candida parapsilosis antifungal resistance”.
I. Faria-Ramos is supported by an FCT PhD grant (SFRH/BD/91155/2012).
Funding
This work was financially supported by Pfizer Inc. grant WS759839.
Conflict of interest
No conflicts to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faria-Ramos, I., Neves-Maia, J., Ricardo, E. et al. Species distribution and in vitro antifungal susceptibility profiles of yeast isolates from invasive infections during a Portuguese multicenter survey. Eur J Clin Microbiol Infect Dis 33, 2241–2247 (2014). https://doi.org/10.1007/s10096-014-2194-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2194-8