Abstract
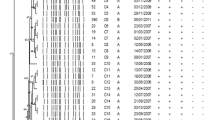
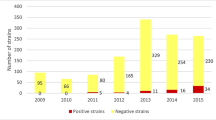
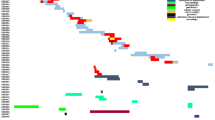
The purpose of this investigation was to determine the prevalence of plasmid-mediated AmpC (pAmpC) and carbapenemases in Enterobacteriaceae collected from 35 hospitals in Spain and to establish their epidemiological relationships. We conducted a prospective multi-centre study on pAmpC- or carbapenemase-producing Enterobacteriaceae isolates from clinical samples collected from February to July 2009. The strains suspected to carry pAmpC were resistant or showed intermediate susceptibility to co-amoxiclav and second- or third-generation cephalosporins. Strains suspected to carry a carbapenemase were selected because they showed a minimum inhibitory concentration (MIC) to imipenem >1 mg/L. Polymerase chain reaction (PCR) and a sequencing strategy were used to characterise the enzymes. The clonal relationships between isolates was analysed by pulsed field gel electrophoresis (PFGE). Among 100,132 Enterobacteriaceae isolates collected, 1,654 were compatible with the production of pAmpC or carbapenemases. We found a prevalence of 0.64 % of pAmpC (n = 635) and 0.04 % of carbapenemases (n = 43). The most prevalent pAmpC enzymes were CMY-type (78.3 %), DHA-type (19.5 %), ACC-type (1.6 %) and FOX-type (0.6 %). The CMY-type was the most frequent in Escherichia coli and Proteus mirabilis species, whereas the DHA-type was mainly found in Klebsiella spp. The enzymes involved in carbapenem resistance were VIM-1, IMP-22 and the new IMP-28. Nine new bla genes were described: bla CMY-54, bla CMY-55, bla CMY-56, bla CMY-57, bla CMY-96, bla DHA-6, bla DHA-7, bla FOX-8 and bla IMP-28. The prevalence of pAmpC or carbapenemases found is not negligible. The CMY-types were the predominant pAmpC, whereas the VIM or IMP enzymes were the predominant carbapenemases. Furthermore, we observed a great genetic diversity among pAmpC-producing strains and a close clonal relationship between carbapenemase-producing strains.
Similar content being viewed by others
References
Pérez-Pérez FJ, Hanson ND (2002) Detection of plasmid-mediated AmpC β-lactamase genes in clinical isolates by using multiplex PCR. J Clin Microbiol 40:2153–2162
Mata C, Miró E, Rivera A et al (2010) Prevalence of acquired AmpC β-lactamases in Enterobacteriaceae lacking inducible chromosomal ampC genes at a Spanish hospital from 1999 to 2007. Clin Microbiol Infect 16:472–476
Navarro F, Pérez-Trallero E, Marimón JM et al (2001) CMY-2-producing Salmonella enterica, Klebsiella pneumoniae, Klebsiella oxytoca, Proteus mirabilis and Escherichia coli strains isolated in Spain (October 1999–December 2000). J Antimicrob Chemother 48:383–389
Yamasaki K, Komatsu M, Abe N et al (2010) Laboratory surveillance for prospective plasmid-mediated AmpC β-lactamases in the Kinki region of Japan. J Clin Microbiol 48:3267–3273
Song W, Kim JS, Kim HS et al (2006) Increasing trend in the prevalence of plasmid-mediated AmpC β-lactamases in Enterobacteriaceae lacking chromosomal ampC gene at a Korean university hospital from 2002 to 2004. Diagn Microbiol Infect Dis 55:219–224
Empel J, Baraniak A, Literacka E et al (2008) Molecular survey of β-lactamases conferring resistance to newer β-lactams in Enterobacteriaceae isolates from Polish hospitals. Antimicrob Agents Chemother 52:2449–2454
Miró E, Segura C, Navarro F et al (2010) Spread of plasmids containing the bla VIM-1 and bla CTX-M genes and the qnr determinant in Enterobacter cloacae, Klebsiella pneumoniae and Klebsiella oxytoca isolates. J Antimicrob Chemother 65:661–665
Oteo J, Hernández-Almaraz JL, Gil-Antón J et al (2010) Outbreak of VIM-1-carbapenemase-producing Enterobacter cloacae in a pediatric intensive care unit. Pediatr Infect Dis J 29:1144–1146
Conejo MC, Domínguez MC, López-Cerero L et al (2010) Isolation of multidrug-resistant Klebsiella oxytoca carrying bla IMP-8, associated with OXY hyperproduction, in the intensive care unit of a community hospital in Spain. J Antimicrob Chemother 65:1071–1073
Giakoupi P, Maltezou H, Polemis M et al; Greek System for the Surveillance of Antimicrobial Resistance (2009) KPC-2-producing Klebsiella pneumoniae infections in Greek hospitals are mainly due to a hyperepidemic clone. Euro Surveill 14. pii: 19218
Cuzon G, Ouanich J, Gondret R et al (2011) Outbreak of OXA-48-positive carbapenem-resistant Klebsiella pneumoniae isolates in France. Antimicrob Agents Chemother 55:2420–2423
Struelens MJ, Monnet DL, Magiorakos AP et al; European NDM-1 Survey Participants (2010) New Delhi metallo-β-lactamase 1-producing Enterobacteriaceae: emergence and response in Europe. Euro Surveill 15. pii: 19716
Miriagou V, Cornaglia G, Edelstein M et al (2010) Acquired carbapenemases in Gram-negative bacterial pathogens: detection and surveillance issues. Clin Microbiol Infect 16:112–22
Navarro F, Calvo J, Cantón R et al (2011) Detection of resistance phenotypes in gram-negative bacteria. Enferm Infecc Microbiol Clin 29:524–534
Walther-Rasmussen J, Høiby N (2007) Class A carbapenemases. J Antimicrob Chemother 60:470–482
Clinical and Laboratory Standards Institute (CLSI) (2005) Performance standards for antimicrobial susceptibility testing; fourteenth informational supplement, M100-S14. CLSI, Wayne, PA, USA
Pasteran F, Mendez T, Guerriero L et al (2009) Sensitive screening tests for suspected class A carbapenemase production in species of Enterobacteriaceae. J Clin Microbiol 47:1631–1639
Dubois V, Poirel L, Marie C et al (2002) Molecular characterization of a novel class 1 integron containing bla GES-1 and a fused product of aac(3)-Ib/aac(6″)-Ib” gene cassettes in Pseudomonas aeruginosa. Antimicrob Agents Chemother 46:638–645
Yigit H, Queenan AM, Anderson GJ et al (2001) Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother 45:1151–1161
Poirel L, Magalhaes M, Lopes M et al (2004) Molecular analysis of metallo-β-lactamase gene bla SPM-1-surrounding sequences from disseminated Pseudomonas aeruginosa isolates in Recife, Brazil. Antimicrob Agents Chemother 48:1406–1409
Poirel L, Lambert T, Türkoglü S et al (2001) Characterization of Class 1 integrons from Pseudomonas aeruginosa that contain the bla VIM-2 carbapenem-hydrolyzing β-lactamase gene and of two novel aminoglycoside resistance gene cassettes. Antimicrob Agents Chemother 45:546–552
Rodríguez-Baño J, Miró E, Villar M et al (2012) Colonisation and infection due to Enterobacteriaceae producing plasmid-mediated AmpC β-lactamases. J Infect 64:176–183
Oteo J, Navarro C, Cercenado E et al (2006) Spread of Escherichia coli strains with high-level cefotaxime and ceftazidime resistance between the community, long-term care facilities, and hospital institutions. J Clin Microbiol 44:2359–2366
Sabbuba NA, Mahenthiralingam E, Stickler DJ (2003) Molecular epidemiology of Proteus mirabilis infections of the catheterized urinary tract. J Clin Microbiol 41:4961–4965
Tenover FC, Arbeit RD, Goering RV et al (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33:2233–2239
Ding H, Yang Y, Lu Q et al (2008) The prevalence of plasmid-mediated AmpC β-lactamases among clinical isolates of Escherichia coli and Klebsiella pneumoniae from five children’s hospitals in China. Eur J Clin Microbiol Infect Dis 27:915–921
Queenan AM, Bush K (2007) Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev 20:440–458
Tórtola MT, Lavilla S, Miró E et al (2005) First detection of a carbapenem-hydrolyzing metalloenzyme in two Enterobacteriaceae isolates in Spain. Antimicrob Agents Chemother 49:3492–3494
Tato M, Coque TM, Ruíz-Garbajosa P et al (2007) Complex clonal and plasmid epidemiology in the first outbreak of Enterobacteriaceae infection involving VIM-1 metallo-β-lactamase in Spain: toward endemicity? Clin Infect Dis 45:1171–1178
Pérez-Llarena FJ, Fernández A, Zamorano L et al (2012) Characterization of a novel IMP-28 metallo-β-lactamase from a Spanish Klebsiella oxytoca clinical isolate. Antimicrob Agents Chemother 56:4540–4543
Gaibani P, Ambretti S, Berlingeri A et al (2011) Rapid increase of carbapenemase-producing Klebsiella pneumoniae strains in a large italian hospital: surveillance period 1 March–30 September 2010. Euro Surveill 16. pii: 19800
Solé M, Pitart C, Roca I et al (2011) First description of an Escherichia coli strain producing NDM-1 carbapenemase in Spain. Antimicrob Agents Chemother 55:4402–4404
Pitart C, Solé M, Roca I et al (2011) First outbreak of a plasmid-mediated carbapenem-hydrolyzing OXA-48 β-lactamase in Klebsiella pneumoniae in Spain. Antimicrob Agents Chemother 55:4398–4401
Oteo J, Cercenado E, Cuevas O et al (2010) AmpC β-lactamases in Escherichia coli: emergence of CMY-2-producing virulent phylogroup D isolates belonging mainly to STs 57, 115, 354, 393, and 420, and phylogroup B2 isolates belonging to the international clone O25b-ST131. Diagn Microbiol Infect Dis 67:270–276
Naseer U, Haldorsen B, Simonsen GS et al (2010) Sporadic occurrence of CMY-2-producing multidrug-resistant Escherichia coli of ST-complexes 38 and 448, and ST131 in Norway. Clin Microbiol Infect 16:171–178
Empel J, Hrabák J, Kozińska A et al (2010) DHA-1-producing Klebsiella pneumoniae in a teaching hospital in the Czech Republic. Microb Drug Resist 16:291–295
Ohana S, Leflon V, Ronco E et al (2005) Spread of a Klebsiella pneumoniae strain producing a plasmid-mediated ACC-1 AmpC β-lactamase in a teaching hospital admitting disabled patients. Antimicrob Agents Chemother 49:2095–2097
Psichogiou M, Tassios PT, Avlamis A et al (2008) Ongoing epidemic of bla VIM-1-positive Klebsiella pneumoniae in Athens, Greece: a prospective survey. J Antimicrob Chemother 61:59–63
Cagnacci S, Gualco L, Roveta S et al (2008) Bloodstream infections caused by multidrug-resistant Klebsiella pneumoniae producing the carbapenem-hydrolysing VIM-1 metallo-β-lactamase: first Italian outbreak. J Antimicrob Chemother 61:296–300
Acknowledgements
To the members of the GEMARA and GEIH groups: Emilia Cercenado (Hospital Gregorio Marañon, Madrid), Beatriz Orden (CE Argüelles, CEP Madrid, Hospital Universitario Puerta del Hierro, Madrid), Andrea Mª Gonzalez and Alberto Delgado-Iribarren (Hospital Fundación de Alcorcón, Madrid), Rafael Cantón and M. Isabel Morosini (Hospital Ramon y Cajal, Madrid), Carmen Aspiroz and Blanca Fortuño (Hospital Royo Villanova, Zaragoza), Fe Tubau and Josefina Ayats (Hospital de Bellvitge, Barcelona), F. Javier Castillo and Cristina Seral (Hospital Clínico Universitario Lozano Blesa, Zaragoza), Margarita Salvador and Concepción Segura (Laboratori de Referencia, Barcelona), Cayo Sádaba and Marta Lamata (Fundación Hospital de Calahorra, La Rioja), Ana Granados and Dionisia Fontanals (Hospital Parc Taulí, Barcelona), Frederic Ballester and Oscar Villuenda (Hospital de Sant Joan de Reus, Reus), Frederic Gómez and Rafael Sánchez (Hospital Universitari Joan XXIII, Tarragona), Cristina Pitart and Francesc Marco (Hospital Clínic de Barcelona, Barcelona), Gloria Royo and Montserrat Ruíz (Hospital General Universitari d’Elx, Elx), Mª Luz Núñez and Antonio Altuna Cuesta (Hospital Reina Sofia de Murcia, Murcia), José Luis López and Miguel Salavert (Hospital Universitari La Fe, Valencia), Pilar Marín (Hospital Puerta del Mar, Cadiz), Pilar Teno (Hospital San Pedro de Alcántara, Cáceres), Patricia Iraurgui and Cecilia Martín (Hospital Virgen del Rocío, Sevilla), Gloria Esteban and Begoña Fernández (Complejo hospitalario de Ourense, Ourense), M. Isabel Fernández-Natal (Complejo Asistencial de León, León), Carlos Fuster (Hospital de El Bierzo, León), Fernando García-Garrote and Amparo Coira Nieto (Complejo Hospitalario Xeral-Calde de Lugo, Lugo), Ana Fleites and Marta Lantero (Hospital Universitario Central de Asturias, Oviedo), Andrés Canut (Hospital Santiago Apostol Osakidetza, Servicio Vasco de Salud, Basurto), Estibaliz Ugalde and Carmen Torres (Hospital San Pedro, Logroño), Mª Luz Cordón and Ainara Rodríguez (Hospital de Alto Deba, Mondragón), Mirian Alkorta and Ana María Iturzaeta (Hospital de Zumárraga, Zumárraga), Joxe Mari Manterola (Hospital de Mendaro, Mendaro).
We thank C. Newey for revising the English language in this paper.
Funding
This study was partially supported by the Ministry of Health and Consumer Affairs, Instituto de Salud Carlos III—FEDER, the Spanish Network for Research in Infectious Diseases (REIPI RD06/0008), by a grant from the Fondo de Investigación Sanitaria (PS09/00125) and by AstraZeneca Farmacéutica Spain and Wyeth (now Pfizer) pharmaceutical industries.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miró, E., Agüero, J., Larrosa, M.N. et al. Prevalence and molecular epidemiology of acquired AmpC β-lactamases and carbapenemases in Enterobacteriaceae isolates from 35 hospitals in Spain. Eur J Clin Microbiol Infect Dis 32, 253–259 (2013). https://doi.org/10.1007/s10096-012-1737-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1737-0