Abstract
Objective
Encephaloceles (ENCs) may cause clinical complications, including drug-resistant epilepsy that can be cured with epilepsy surgery.
Methods
We describe clinical, diagnostic, and neuropathological findings of 12 patients with temporal ENC and epilepsy evaluated for surgery and compare them with a control group of 26 temporal lobe epilepsy (TLE) patients.
Results
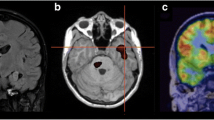
Six patients had unilateral and 6 bilateral temporal ENCs. Compared to TLEs, ENCs showed i) later epilepsy onset, ii) higher prevalence of psychiatric comorbidities, iii) no history of febrile convulsions, and iv) ictal semiology differences. Seven patients had MRI signs of gliosis, and 9 of intracranial hypertension. Interictal EEG analysis in ENCs demonstrated significant differences with controls: prominent activity in the beta/gamma frequency bands in frontal regions, interictal short sequences of low-voltage fast activity, and less frequent and more localized interictal epileptiform discharges. Ictal EEG patterns analyzed in 9 ENCs showed delayed and slower contralateral spread compared to TLEs. All ENCs that underwent surgery (7 lobectomies and 1 lesionectomy) are in Engel class I. Neuropathological examination revealed 4 patterns: herniated brain fragments, focal layer I distortion, white matter septa extending into the cortex, and altered gyral profile.
Conclusions and significance
The described peculiarities might help clinicians to suspect the presence of largely underdiagnosed ENCs.





Similar content being viewed by others
Data availability
Raw data are available in national repository.
Abbreviations
- BMI:
-
Body mass index
- ENC:
-
Encephalocele
- FCD:
-
Focal cortical dysplasia
- GFAP:
-
Glial-fibrillary acid protein
- HE:
-
Hematoxylin and eosin
- IED:
-
Interictal epileptic discharge
- IHC:
-
Immunohistochemistry
- IIH:
-
Idiopathic intracranial hypertension
- LFB:
-
Luxol fast blue
- LVFA:
-
Low voltage fast activity
- RP:
-
Relative power
- SNR:
-
Signal-to-noise ratio
- TLE:
-
Temporal lobe epilepsy
References
Vargas MI, Vulliemoz S, Rosset A et al (2008) Temporal anterior encephalocele. Neurology 71:1293. https://doi.org/10.1212/01.wnl.0000327602.65933.79
Wind JJ, Caputy AJ, Roberti F (2008) Spontaneous encephaloceles of the temporal lobe. Neurosurg Focus 25:1–6. https://doi.org/10.3171/FOC.2008.25.12.E11
Byrne RW, Smith AP, Roh D, Kanner A (2010) Occult middle fossa encephaloceles in patients with temporal lobe epilepsy. World Neurosurg 73:541–546. https://doi.org/10.1016/j.wneu.2010.01.018
Matthews YY, Dean F, Lim MJ et al (2017) Pseudotumor cerebri syndrome in childhood: Incidence, clinical profile and risk factors in a national prospective population-based cohort study. Arch Dis Child 102:715–721. https://doi.org/10.1136/archdischild-2016-312238
Urbach H, Jamneala G, Mader I et al (2017) Temporal lobe epilepsy due to meningoencephaloceles into the greater sphenoid wing: a consequence of idiopathic intracranial hypertension? Neuroradiology 60:51–60. https://doi.org/10.1007/s00234-017-1929-5
Benson JC, Lane J, Geske JR et al (2019) Prevalence of asymptomatic middle cranial fossa floor pits and encephaloceles on MR imaging. Am J Neuroradiol 40:2090–2093. https://doi.org/10.3174/ajnr.A6311
Pettersson DR, Hagen KS, Sathe NC et al (2020) MR imaging features of middle cranial fossa encephaloceles and their associations with epilepsy. Am J Neuroradiol 41:268–2074. https://doi.org/10.3174/ajnr.A6798
Rehder D (2020) Idiopathic Intracranial Hypertension: Review of Clinical Syndrome, Imaging Findings, and Treatment. Curr Probl Diagn Radiol 49:205–214. https://doi.org/10.1067/j.cpradiol.2019.02.012
Ramos-Fresnedo A, Domingo RA, McGeary RC et al (2021) Encephalocele-Associated Drug-Resistant Epilepsy of Adult Onset: Diagnosis, Management, and Outcomes. World Neurosurg 151:91–101. https://doi.org/10.1016/j.wneu.2021.04.121
Campbell ZM, Hyer JM, Lauzon S et al (2018) Detection and characteristics of temporal encephaloceles in patients with refractory epilepsy. Am J Neuroradiol 39:1468–1472. https://doi.org/10.3174/ajnr.A5704
Paule E, Freiman TM, Strzelczyk A et al (2019) Characteristics of bilateral versus unilateral temporal encephalocele-associated epilepsy. Seizure 71:13–19. https://doi.org/10.1016/j.seizure.2019.05.022
Tse GT, Frydman AS, O’Shea MF et al (2020) Anterior temporal encephaloceles: Elusive, important, and rewarding to treat. Epilepsia 61:2675–2684. https://doi.org/10.1111/epi.16729
Lapalme-Remis S, Witte RJ, Wong-Kisiel LC (2017) Anteroinferior Temporal Encephalocele: A Surgically Treatable Cause of Pharmacoresistant Epilepsy. Pediatr Neurol 77:89–90. https://doi.org/10.1016/j.pediatrneurol.2017.07.003
Gil Guerra AB, Rodríguez Velasco M, Sigüenza González R, Sánchez Ronco MA (2020) Temporal lobe encephalocele, a subtle structural lesion that can be associated with temporal lobe epilepsy. Neurologia 35:216–217. https://doi.org/10.1016/j.nrl.2018.01.004
Reeves RA, Gorniack R (2021) Neuroimaging in epilepsy. In: Epilepsy: A Century of Discovery. 85–132
Faulkner HJ, Sandeman DR, Love S et al (2010) Epilepsy surgery for refractory epilepsy due to encephalocele: A case report and review of the literature. Epileptic Disord 12:160–166. https://doi.org/10.1684/epd.2010.0308
Gasparini S, Ferlazzo E, Pustorino G et al (2018) Epileptogenic role of occult temporal encephalomeningocele. Neurology 90:1–4. https://doi.org/10.1212/WNL.0000000000005263
Morone PJ, Sweeney AD, Carlson ML et al (2015) Temporal Lobe Encephaloceles: A Potentially Curable Cause of Seizures. Otol Neurotol 36:1439–1442. https://doi.org/10.1097/MAO.0000000000000825
Toledano R, Jiménez-Huete A, Campo P et al (2016) Small temporal pole encephalocele: A hidden cause of “normal” MRI temporal lobe epilepsy. Epilepsia 57:841–851. https://doi.org/10.1111/epi.13371
Fong MWK, Sala-Padro J, Bartley M et al (2019) The varied semiology of seizures in the context of small anterior temporal encephaloceles. Epileptic Disord 21:347–352. https://doi.org/10.1684/epd.2019.1081
Toledano R, Campo P, Gil-Nagel A (2020) Temporal pole epilepsy: Do not forget to look for occult encephaloceles. Epilepsia 61:2859–2860. https://doi.org/10.1111/epi.16760
Saavalainen T, Jutila L, Mervaala E et al (2015) Temporal anteroinferior encephalocele. Neurology 85:1467–1474. https://doi.org/10.1212/WNL.0000000000002062
Panov F, Li Y, Chang EF et al (2016) Epilepsy with temporal encephalocele: Characteristics of electrocorticography and surgical outcome. Epilepsia 57:e33–e38. https://doi.org/10.1111/epi.13271
Hsu CC-T, Stenberg L, Krings T (2020) Imaging the Patient with Epilepsy. In: Hodler J (ed) Diseases of the Brain, Head and Neck, Spine. IDKD Springer Series, 111–130
de Souza JPSAS, Mullin J, Wathen C et al (2017) The usefulness of stereo-electroencephalography (SEEG) in the surgical management of focal epilepsy associated with “hidden” temporal pole encephalocele: a case report and literature review. Neurosurg Rev 41:347–354. https://doi.org/10.1007/s10143-017-0922-0
Gasparini S, Ferlazzo E, Villani F et al (2014) Refractory epilepsy and encephalocele: Lesionectomy or tailored surgery? Seizure 23:583–584
Tsalouchidou PE, Zoellner JP, Kirscht A et al (2023) Temporal encephaloceles and coexisting epileptogenic lesions. Epilepsia Open 8:113–124. https://doi.org/10.1002/epi4.12674
Tatum WO (2012) Mesial temporal lobe epilepsy. J Clin Neurophysiol 29:356–365. https://doi.org/10.1097/WNP.0b013e31826b3ab7
Asadi-Pooya AA, Nei M, Sharan A, Sperling MR (2015) Type of preoperative aura may predict postsurgical outcome in patients with temporal lobe epilepsy and mesial temporal sclerosis. Epilepsy Behav 50:98–100. https://doi.org/10.1016/j.yebeh.2015.06.041
Didato G, Chiesa V, Villani F et al (2015) Bitemporal epilepsy : A specific anatomo-electro-clinical phenotype in the temporal lobe epilepsy spectrum. Seizure 31:112–119. https://doi.org/10.1016/j.seizure.2015.07.013
Engel J (1996) Introduction to temporal lobe epilepsy. In: Epilepsy Research. 141–150
Englot DJ, Morgan VL, Chang C (2020) Impaired vigilance networks in temporal lobe epilepsy: Mechanisms and clinical implications. Epilepsia 61:189–202. https://doi.org/10.1111/epi.16423
Varotto G, Burini A, Didato G et al (2021) Impaired awareness in mesial temporal lobe epilepsy: Network analysis of foramen ovale and scalp EEG. Clin Neurophysiol 132:3084–3094. https://doi.org/10.1016/j.clinph.2021.09.011
Sanchez-Gistau V, Sugranyes G, Baillés E et al (2012) Is major depressive disorder specifically associated with mesial temporal sclerosis? Epilepsia 53:386–392. https://doi.org/10.1111/j.1528-1167.2011.03373.x
di Giacomo R, Didato G, Belcastro V et al (2021) Rage and aggressive behaviour in frontal lobe epilepsy: description of a case and review of the mechanisms of aggressive behaviour in epilepsy and dementia. Epileptic Disord 23:419–425. https://doi.org/10.1684/epd.2021.1277
Elias GJB, Germann J, Neudorfer C et al (2021) Impact of Mesial Temporal Lobe Resection on Brain Structure in Medically Refractory Epilepsy. World Neurosurg 152:e652–e665. https://doi.org/10.1016/j.wneu.2021.06.039
Author information
Authors and Affiliations
Contributions
All authors
1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work;
2) drafted the work or revised it critically for important intellectual content;
3) approved the version to be published; and.
4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors report no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Di Giacomo, R., Burini, A., Visani, E. et al. Distinctive electro-clinical, neuroimaging and histopathological features of temporal encephaloceles associated to epilepsy. Neurol Sci 44, 4451–4463 (2023). https://doi.org/10.1007/s10072-023-06939-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06939-x