Abstract
Objective
The aim of this meta-analysis was to evaluate the evidence on the effectiveness of music therapy in the recovery of language function in post-stroke aphasia, compared with conventional therapy or no therapy.
Methods
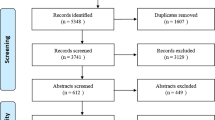
We searched studies that explored the effect of music therapy on language function in post-stroke aphasia and published in PubMed, Embase, the Cochrane Library, Web of Science, CINAHL, ProQuest Digital Dissertations, and ClinicalTrials.gov from inception to March 2021. Six reviewers independently screened out eligible studies, extracted data, and evaluated the methodological quality. Results were pooled using mean difference (MD) with 95% confidence interval (CI). Heterogeneity was assessed by the chi-square test and I2 statistic.
Results
Six studies were included in this meta-analysis involving 115 patients. The methodological quality of these studies ranged from poor to excellent. There was significant mean difference in functional communication for post-stroke aphasia by 1.45 (95% CI: 0.24, 2.65; P = 0.02, from poor to excellent evidence), in repetition by 6.49 (95% CI: 0.97, 12.00; P = 0.02, from acceptable to excellent evidence), and in naming by 11.44 (95% CI: 1.63, 21.26; P = 0.02, from acceptable to excellent evidence). But there was no significant difference in comprehension for post-stroke aphasia by 7.21 (95% CI: − 10.88, 25.29; P = 0.43, from acceptable to excellent evidence).
Conclusions
Music therapy can improve functional communication, repetition, and naming in patients with post-stroke aphasia, but did not significantly improve comprehension.
Trial registration
CRD42021251526





Similar content being viewed by others
References
Berthier ML (2005) Poststroke aphasia: epidemiology, pathophysiology and treatment. Drugs Aging 22(2):163–182. https://doi.org/10.2165/00002512-200522020-00006
Fridriksson J, Rorden C, Elm J, Sen S, George MS, Bonilha L (2018) Transcranial direct current stimulation vs sham stimulation to treat aphasia after stroke: a randomized clinical trial. JAMA Neurol 75(12):1470–1476. https://doi.org/10.1001/jamaneurol.2018.2287
Godecke E, Armstrong E, Rai T, Ciccone N, Rose ML, Middleton S, Whitworth A, Holland A, Ellery F, Hankey GJ, Cadilhac DA, Bernhardt J, VERSE Collaborative Group (2021) A randomized control trial of intensive aphasia therapy after acute stroke: the Very Early Rehabilitation for SpEech (VERSE) study. Int J Stroke 16(5)556-572https://doi.org/10.1177/1747493020961926
Fama ME, Turkeltaub PE (2014) Treatment of poststroke aphasia: current practice and new directions. Semin Neurol 34(5):504–513. https://doi.org/10.1055/s-0034-1396004
Lendrem W, Lincoln NB (1985) Spontaneous recovery of language in patients with aphasia between 4 and 34 weeks after stroke. J Neurol Neurosurg Psychiatry 48(8):743–748. https://doi.org/10.1136/jnnp.48.8.743
Brady MC, Kelly H, Godwin J, Enderby P, Campbell P (2016) Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev 2016(6):CD000425. https://doi.org/10.1002/14651858.CD000425.pub4
Lazar RM, Minzer B, Antoniello D, Festa JR, Krakauer JW, Marshall RS (2010) Improvement in aphasia scores after stroke is well predicted by initial severity. Stroke 41(7):1485–1488. https://doi.org/10.1161/STROKEAHA.109.577338
Code C (2003) The quantity of life for people with chronic aphasia. Neuropsychol Rehabil 13(3):379-390https://doi.org/10.1080/09602010244000255
Jones F, Riazi A (2011) Self-efficacy and self-management after stroke: a systematic review. Disabil Rehabil 33(10):797–810. https://doi.org/10.3109/09638288.2010.511415
Engelter ST, Gostynski M, Papa S, Frei M, Born C, Ajdacic-Gross V, Gutzwiller F, Lyrer PA (2006) Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke 37(6):1379–1384. https://doi.org/10.1161/01.STR.0000221815.64093.8c
Magee WL, Clark I, Tamplin J, Bradt J (2017) Music interventions for acquired brain injury. Cochrane Database Syst Rev 1(1):D6787. https://doi.org/10.1002/14651858.CD006787.pub3
Aalbers S, Fusar-Poli L, Freeman RE, Spreen M, Ket JC, Vink AC, Maratos A, Crawford M, Chen XJ, Gold C (2017) Music therapy for depression. Cochrane Database Syst Rev 11(11):D4517. https://doi.org/10.1002/14651858.CD004517.pub3
Särkämö T, Tervaniemi M, Laitinen S, Forsblom A, Soinila S, Mikkonen M, Autti T, Silvennoinen HM, Erkkilä J, Laine M, Peretz I, Hietanen M (2008) Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain 131(Pt 3):866–76. https://doi.org/10.1093/brain/awn013
Kim SJ, Koh I (2005) The effects of music on pain perception of stroke patients during upper extremity joint exercises. J Music Ther 42(1):81–92. https://doi.org/10.1093/jmt/42.1.81
Tarrant M, Carter M, Dean SG, Taylor R, Warren FC, Spencer A, Adamson J, Landa P, Code C, Backhouse A, Lamont RA, Calitri R (2021) Singing for people with aphasia (SPA): results of a pilot feasibility randomised controlled trial of a group singing intervention investigating acceptability and feasibility. BMJ Open 11(1):e040544. https://doi.org/10.1136/bmjopen-2020-040544
Sihvonen AJ, Leo V, Ripollés P, Lehtovaara T, Ylönen A, Rajanaro P, Laitinen S, Forsblom A, Saunavaara J, Autti T, Laine M, Rodríguez-Fornells A, Tervaniemi M, Soinila S, Särkämö T (2020) Vocal music enhances memory and language recovery after stroke: pooled results from two RCTs. Ann Clin Transl Neurol 7(11):2272–2287. https://doi.org/10.1002/acn3.51217
Leonardi S, Cacciola A, De Luca R, Aragona B, Andronaco V, Milardi D, Bramanti P, Calabrò RS (2018) The role of music therapy in rehabilitation: improving aphasia and beyond. Int J Neurosci 128(1):90–99. https://doi.org/10.1080/00207454.2017.1353981
Shi ER, Zhang Q (2020) A domain-general perspective on the role of the basal ganglia in language and music: benefits of music therapy for the treatment of aphasia. Brain Lang 206:104811. https://doi.org/10.1016/j.bandl.2020.104811
Särkämö T, Sihvonen AJ (2018) Golden oldies and silver brains: deficits, preservation, learning, and rehabilitation effects of music in ageing-related neurological disorders. Cortex 109:104–123. https://doi.org/10.1016/j.cortex.2018.08.034
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1)1https://doi.org/10.1186/2046-4053-4-1
Bhogal SK, Teasell RW, Foley NC, Speechley MR (2005) The PEDro scale provides a more comprehensive measure of methodological quality than the Jadad scale in stroke rehabilitation literature. J Clin Epidemiol 58(7):668–673. https://doi.org/10.1016/j.jclinepi.2005.01.002
Foley NC, Teasell RW, Bhogal SK, Speechley MR (2003) Stroke rehabilitation evidence-based review: methodology. Top Stroke Rehabil 10(1):1–7
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928https://doi.org/10.1136/bmj.d5928
Yang FG, Wang NY, Lin C, Chiang T, Lin C, Lai Y (2019) Change of neuronal pathways in Chinese speakers with non-fluent aphasia after therapy. LINGUA 218(SI):3–13. https://doi.org/10.1016/j.lingua.2018.01.005
Haro-Martínez AM, Lubrini G, Madero-Jarabo R, Díez-Tejedor E, Fuentes B (2019) Melodic intonation therapy in post-stroke nonfluent aphasia: a randomized pilot trial. Clin Rehabil 33(1):44–53. https://doi.org/10.1177/0269215518791004
Van Der Meulen I, Van De Sandt-Koenderman MW, Heijenbrok MH, Visch-Brink E, Ribbers GM (2016) Melodic intonation therapy in chronic aphasia: evidence from a pilot randomized controlled trial. Front Hum Neurosci 10:533. https://doi.org/10.3389/fnhum.2016.00533
van der Meulen I, van de Sandt-Koenderman WM, Heijenbrok-Kal MH, Visch-Brink EG, Ribbers GM (2014) the efficacy and timing of melodic intonation therapy in subacute aphasia. Neurorehabil Neural Repair 28(6):536–544. https://doi.org/10.1177/1545968313517753
Lim KB, Kim YK, Lee HJ, Yoo J, Hwang JY, Kim JA, Kim SK (2013) The therapeutic effect of neurologic music therapy and speech language therapy in post-stroke aphasic patients. Ann Rehabil Med 37(4):556–562. https://doi.org/10.5535/arm.2013.37.4.556
Conklyn D, Novak E, Boissy A, Bethoux F, Chemali K (2012) The effects of modified melodic intonation therapy on nonfluent aphasia: a pilot study. J Speech Lang Hear Res 55(5):1463–1471. https://doi.org/10.1044/1092-4388(2012/11-0105)
Yang Y, Fang YY, Gao J, Geng GL (2019) Effects of five-element music on language recovery in patients with poststroke aphasia: a systematic review and meta-analysis. J Altern Complement Med 25(10):993–1004. https://doi.org/10.1089/acm.2018.0479
Author information
Authors and Affiliations
Contributions
Qingqing Liu and Yu Yin initiated the study; Weibo Li and Zhenbiao Zhao contributed to the study design; Qingqing Liu, Yu Yin, Zhenbiao Zhao, and Yuhui Yang carried out the search and selection study; Yue Zhao and Yafei Tan performed data extraction; Yue Zhao and Yuhui Yang evaluated the quality of the study; Qingqing Liu and Jing Yu assessed the risk of bias; Qingqing Liu, Weibo Li, Yu Yin, and Zhenbiao Zhao contributed to statistical analysis. All authors contributed to interpreting the results. Qingqing Liu and Yu Yin wrote the first draft of the manuscript. Other authors contributed to the revision of the draft. All authors agreed with the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 328 kb)
Rights and permissions
About this article
Cite this article
Liu, Q., Li, W., Yin, Y. et al. The effect of music therapy on language recovery in patients with aphasia after stroke: a systematic review and meta-analysis. Neurol Sci 43, 863–872 (2022). https://doi.org/10.1007/s10072-021-05743-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05743-9