Abstract
Background and purpose
The relationship between lipid levels and the prognosis of acute intracerebral hemorrhage (ICH) remains controversial. Thus, we aimed to investigate whether lower low-density lipoprotein cholesterol (LDL-C) levels increased the risk of adverse outcomes, as well as the current situation of statin treatment in acute ICH patients with premorbid lipid-lowering therapy.
Methods
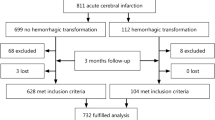
From August 1, 2015, to July 31, 2019, a total of 73,098 ICH patients were included in our study from the Chinese Stroke Center Alliance program. Patients were grouped by LDL-C levels of < 1.4 mmol/L, 1.4–1.8 mmol/L, 1.8–2.6 mmol/L, and > 2.6 mmol/L. Logistic regression was used to assess the association between LDL-C levels and the composite risk of hematoma expansion (HE) or in-hospital death. Moreover, statin treatment in ICH patients with cardio-cerebrovascular diseases was analyzed.
Results
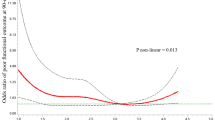
In total, 6368 (8.7%) patients were identified as a composite of HE or in-hospital death with a mean LDL-C level of 2.9 ± 1.7 mmol/L. In the univariate analysis, patients who achieved lower LDL-C concentrations under 1.4 mmol/L had a 36% higher risk of adverse outcomes compared with the ≥ 2.6 mmol/L group (OR 1.36, 95%CI 1.23–1.51). Similar results were obtained in multivariate analyses, especially for patients with GCS scores of 9–15. For acute ICH patients with concomitant atherosclerotic disease, statin treatment was discontinued in the majority of Chinese population.
Conclusions
Lower LDL-C levels (< 1.4 mmol/L) are associated with an increased risk of HE and ensuing mortality in acute ICH patients. Maintaining an optimal LDL-C range may have therapeutic potential against HE which merits further investigation.


Similar content being viewed by others
Data availability
Data are available to researchers on request for purpose of reproducing the results or replicating the procedure by directly contacting the corresponding author.
Code availability
N/A
Change history
09 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10072-022-06064-1
References
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L et al (2017) Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation 135(8):759–771. https://doi.org/10.1161/circulationaha.116.025250
An SJ, Kim TJ, Yoon BW (2017) Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke 19(1):3–10. https://doi.org/10.5853/jos.2016.00864
Dowlatshahi D, Demchuk AM, Flaherty ML, Ali M, Lyden PL, Smith EE (2011) Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology 76(14):1238–1244. https://doi.org/10.1212/WNL.0b013e3182143317
Cannon CP (2020) Low-density lipoprotein cholesterol: lower is totally better. J Am Coll Cardiol 75(17):2119–2121. https://doi.org/10.1016/j.jacc.2020.03.033
Chang JJ, Katsanos AH, Khorchid Y, Dillard K, Kerro A, Burgess LG et al (2018) Higher low-density lipoprotein cholesterol levels are associated with decreased mortality in patients with intracerebral hemorrhage. Atherosclerosis 269:14–20. https://doi.org/10.1016/j.atherosclerosis.2017.12.008
Cai B, Peng L, Wang ZB, Zhang M, Peng B (2020) Association between serum lipid and hematoma expansion after spontaneous intracerebral hemorrhage in Chinese patients. J Stroke Cerebrovasc Dis 29(6):104793. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104793
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L et al (2020) 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 41(1):111–188. https://doi.org/10.1093/eurheartj/ehz455
Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE et al (2006) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 355(6):549–559. https://doi.org/10.1056/NEJMoa061894
Goldstein LB, Amarenco P, Szarek M, Callahan A 3rd, Hennerici M, Sillesen H et al (2008) Hemorrhagic stroke in the stroke prevention by aggressive reduction in cholesterol levels study. Neurology 70(24 Pt 2):2364–2370. https://doi.org/10.1212/01.wnl.0000296277.63350.77
Kuramatsu JB, Gerner ST, Schellinger PD, Glahn J, Endres M, Sobesky J et al (2015) Anticoagulant reversal, blood pressure levels, and anticoagulant resumption in patients with anticoagulation-related intracerebral hemorrhage. JAMA 313(8):824–836. https://doi.org/10.1001/jama.2015.0846
Hackam DG, Woodward M, Newby LK, Bhatt DL, Shao M, Smith EE et al (2011) Statins and intracerebral hemorrhage: collaborative systematic review and meta-analysis. Circulation 124(20):2233–2242. https://doi.org/10.1161/circulationaha.111.055269
Dowlatshahi D, Demchuk AM, Fang J, Kapral MK, Sharma M, Smith EE (2012) Association of statins and statin discontinuation with poor outcome and survival after intracerebral hemorrhage. Stroke 43(6):1518–1523. https://doi.org/10.1161/strokeaha.111.645978
Flint AC, Conell C, Rao VA, Klingman JG, Sidney S, Johnston SC et al (2014) Effect of statin use during hospitalization for intracerebral hemorrhage on mortality and discharge disposition. JAMA Neurol 71(11):1364–1371. https://doi.org/10.1001/jamaneurol.2014.2124
Tapia-Perez JH, Zilke R, Schneider T (2016) Match-study of statin therapy in spontaneous intracerebral hemorrhage: is the discontinuation reasonable? J Neurosurg Sci 60(3):301–312
Siddiqui FM, Langefeld CD, Moomaw CJ, Comeau ME, Sekar P, Rosand J et al (2017) Use of statins and outcomes in intracerebral hemorrhage patients. Stroke 48(8):2098–2104. https://doi.org/10.1161/strokeaha.117.017358
Wang Y, Li Z, Wang Y, Zhao X, Liu L, Yang X et al (2018) Chinese Stroke Center Alliance: a national effort to improve healthcare quality for acute stroke and transient ischaemic attack: rationale, design and preliminary findings. Stroke Vasc Neurol 3(4):256–262. https://doi.org/10.1136/svn-2018-000154
Kothari R, Brott T, Broderick J, Barsan W, Sauerbeck L, Zuccarello M et al (1996) The ABCs of measuring intracerebral hemorrhage volumes. Stroke 27(8):1304–1305. https://doi.org/10.1161/01.str.27.8.1304
Rodriguez-Luna D, Rubiera M, Ribo M, Coscojuela P, Pagola J, Piñeiro S et al (2011) Serum low-density lipoprotein cholesterol level predicts hematoma growth and clinical outcome after acute intracerebral hemorrhage. Stroke 42(9):2447–2452. https://doi.org/10.1161/strokeaha.110.609461
Elkhatib THM, Shehta N, Bessar AA (2019) Hematoma expansion predictors: laboratory and radiological risk factors in patients with acute intracerebral hemorrhage: a prospective observational study. J Stroke Cerebrovasc Dis 28(8):2177–2186. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.04.038
Ramírez-Moreno JM, Casado-Naranjo I, Portilla JC, Calle ML, Tena D, Falcón A et al (2009) Serum cholesterol LDL and 90-day mortality in patients with intracerebral hemorrhage. Stroke 40(5):1917–1920. https://doi.org/10.1161/strokeaha.108.536698
Ovesen C, Christensen AF, Krieger DW, Rosenbaum S, Havsteen I, Christensen H (2014) Time course of early postadmission hematoma expansion in spontaneous intracerebral hemorrhage. Stroke 45(4):994–999. https://doi.org/10.1161/strokeaha.113.003608
Esfahani DR, Radnis CA, Hussein AE, Amin-Hanjani S, Charbel FT, Alaraj A (2017) Thresholds for volume and expansion in intraparenchymal hemorrhage: predictors of neurologic deterioration and mortality. World Neurosurg 106:131–138. https://doi.org/10.1016/j.wneu.2017.06.131
Schmitt S, Castelvetri LC, Simons M (2015) Metabolism and functions of lipids in myelin. Biochim Biophys Acta 1851(8):999–1005. https://doi.org/10.1016/j.bbalip.2014.12.016
Ference BA, Graham I, Tokgozoglu L, Catapano AL (2018) Impact of lipids on cardiovascular health: JACC Health Promotion Series. J Am Coll Cardiol 72(10):1141–1156. https://doi.org/10.1016/j.jacc.2018.06.046
Bang OY, Saver JL, Liebeskind DS, Starkman S, Villablanca P, Salamon N et al (2007) Cholesterol level and symptomatic hemorrhagic transformation after ischemic stroke thrombolysis. Neurology 68(10):737–742. https://doi.org/10.1212/01.wnl.0000252799.64165.d5
Ooneda G, Yoshida Y, Suzuki K, Shinkai H, Hori S, Kobori K et al (1978) Smooth muscle cells in the development of plasmatic arterionecrosis, arteriosclerosis, and arterial contraction. Blood Vessels 15(1–3):148–156. https://doi.org/10.1159/000158160
Chui DH, Marotta F, Rao ML, Liu DS, Zhang SC, Ideo C (1991) Cholesterol-rich LDL perfused at physiological LDL-cholesterol concentration induces platelet aggregation and PAF-acetylhydrolase activation. Biomed Pharmacother. 45(1):37–42. https://doi.org/10.1016/0753-3322(91)90152-j
Yamori Y, Nara Y, Horie R, Ooshima A (1980) Abnormal membrane characteristics of erythrocytes in rat models and men with predisposition to stroke. Clin Exp Hypertens 2(6):1009–1021. https://doi.org/10.3109/10641968009037158
Goritz C, Mauch DH, Pfrieger FW (2005) Multiple mechanisms mediate cholesterol-induced synaptogenesis in a CNS neuron. Mol Cell Neurosci 29(2):190–201. https://doi.org/10.1016/j.mcn.2005.02.006
Raffeld MR, Biffi A, Battey TW, Ayres AM, Viswanathan A, Greenberg SM et al (2015) APOE ε4 and lipid levels affect risk of recurrent nonlobar intracerebral hemorrhage. Neurology 85(4):349–356. https://doi.org/10.1212/wnl.0000000000001790
Sawyer RP, Sekar P, Osborne J, Kittner SJ, Moomaw CJ, Flaherty ML et al (2018) Racial/ethnic variation of APOE alleles for lobar intracerebral hemorrhage. Neurology 91(5):e410–e420. https://doi.org/10.1212/wnl.0000000000005908
Biffi A, Anderson CD, Battey TW, Ayres AM, Greenberg SM, Viswanathan A et al (2015) Association between blood pressure control and risk of recurrent intracerebral hemorrhage. JAMA 314(9):904–912. https://doi.org/10.1001/jama.2015.10082
Endres M, Nolte CH, Scheitz JF (2018) Statin treatment in patients with intracerebral hemorrhage. Stroke 49(1):240–246. https://doi.org/10.1161/strokeaha.117.019322
Acknowledgements
We gratefully appreciate all the participating centers in the CSCA program for their hard work in data collection.
Funding
The Chinese Stroke Center Alliance program was supported by grants from the National Science and Technology Major Project (2017ZX09304018), Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2019-I2M-5–029), and Beijing Natural Science Foundation (Z200016).
Author information
Authors and Affiliations
Consortia
Contributions
Y. Wang performed the experiments, interpreted the results of statistical analysis, and drafted the manuscript. H. Gu and K. Yang conducted the statistical analysis and interpreted the data. J. Wu, R. Jiang, and Z. Li revising the manuscript for intellectual content. Y. Wang and X. Zhao had full access to all of the data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Ethical approval
The study was conducted in accordance with guidelines from the Helsinki Declaration. All participating hospitals received research approval to collect data without requiring individual patient informed consent under the common rule or a waiver of authorization and exemption from their Institutional Review Board.
Consent to participate
N/A
Consent for publication
N/A
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Affiliation 1 should be revised to: China National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Y., Wu, J., Gu, H. et al. Lower low-density lipoprotein cholesterol levels are associated with an increased risk of hematoma expansion and ensuing mortality in acute ICH patients. Neurol Sci 43, 3121–3129 (2022). https://doi.org/10.1007/s10072-021-05742-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05742-w