Abstract
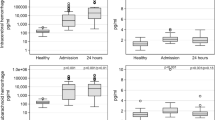
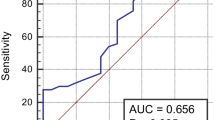
The objective of this study was to explore the efficacy of glial fibrillary acidic protein (GFAP) in differentiating intracerebral hemorrhage (ICH) from ischemic stroke (IS). Suspicious patients of acute stroke were screened and finally diagnosed by computed tomography and magnetic resonance imaging. Blood samples were collected within 2–6 h after onset of symptoms, and serum GFAP level was determined by ELISA assay. The functional outcome for the patients was determined by modified Rankin Scale (mRS) 90 days after onset of symptoms. 43 ICH patients and 65 IS patients were enrolled. GFAP concentration in ICH group was significantly higher than in IS group (p < 0.001). Significant correlation was found when comparing GFAP with National Institutes of Health Stroke Scale (NIHSS) (r = 0.418, p = 0.005) and hemorrhage volume (r = 0.840, p < 0.001) in ICH group, while such correlation was not observed in IS group. ROC analysis indicated that GFAP level at the cut-point of 0.7 ng/ml yielded an AUC of 0.901 (95 % CI 0.828–0.950) with high sensitivity (86.0 %) and specificity (76.9 %) to differentiate ICH from IS. Patients with higher serum GFAP concentration in ICH group experienced poorer functional disability (r = 0.755, p < 0.001), while this phenomenon was not observed in IS group (r = −0.114, p = 0.368). ROC curve analysis found that GFAP level at the cut-point of 1.04 ng/ml yielded an AUC of 0.936 (95 % CI 0.817–0.988) in identifying patients with poor functional outcome, at the sensitivity and specificity of 95.7 and 80.0 %, respectively. GFAP test is a promising technique for diagnosis of ICH from IS and prediction of short-term functional outcomes.



Similar content being viewed by others
References
Sudlow CL, Warlow CP (1997) Comparable studies of the incidence of stroke and its pathological types: results from an international collaboration. International stroke incidence collaboration. Stroke 28(3):491–499
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF (2001) Spontaneous intracerebral hemorrhage. N Engl J Med 344(19):1450–1460
Suzuki K, Kutsuzawa T, Takita K, Ito M, Sakamoto T, Hirayama A et al (1987) Clinico-epidemiologic study of stroke in Akita, Japan. Stroke 18(2):402–406
Kreitzer N, Adeoye O (2013) An update on surgical and medical management strategies for intracerebral hemorrhage. Semin Neurol 33(5):462–467
Juvela S, Hillbom M, Palomaki H (1995) Risk factors for spontaneous intracerebral hemorrhage. Stroke 26(9):1558–1564
Nilsson OG, Lindgren A, Brandt L, Saveland H (2002) Prediction of death in patients with primary intracerebral hemorrhage: a prospective study of a defined population. J Neurosurg 97(3):531–536
Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A et al (2007) Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke 38(5):1655–1711
Schriger DL, Kalafut M, Starkman S, Krueger M, Saver JL (1998) Cranial computed tomography interpretation in acute stroke: physician accuracy in determining eligibility for thrombolytic therapy. JAMA 279(16):1293–1297
Grotta JC, Chiu D, Lu M, Patel S, Levine SR, Tilley BC et al (1999) Agreement and variability in the interpretation of early CT changes in stroke patients qualifying for intravenous rtPA therapy. Stroke 30(8):1528–1533
Zhang J, Zhang CH, Lin XL, Zhang Q, Wang J, Shi SL (2013) Serum glial fibrillary acidic protein as a biomarker for differentiating intracerebral hemorrhage and ischemic stroke in patients with symptoms of acute stroke: a systematic review and meta-analysis. Neurol Sci 34(11):1887–1892
Schiff L, Hadker N, Weiser S, Rausch C (2012) A literature review of the feasibility of glial fibrillary acidic protein as a biomarker for stroke and traumatic brain injury. Mol Diagn Ther 16(2):79–92
Maas MB, Furie KL (2009) Molecular biomarkers in stroke diagnosis and prognosis. Biomark Med 3(4):363–383
Eng LF, Ghirnikar RS, Lee YL (2000) Glial fibrillary acidic protein: GFAP-thirty-one years (1969–2000). Neurochem Res 25(9–10):1439–1451
Missler U, Wiesmann M, Wittmann G, Magerkurth O, Hagenstrom H (1999) Measurement of glial fibrillary acidic protein in human blood: analytical method and preliminary clinical results. Clin Chem 45(1):138–141
Dvorak F, Haberer I, Sitzer M, Foerch C (2009) Characterisation of the diagnostic window of serum glial fibrillary acidic protein for the differentiation of intracerebral haemorrhage and ischaemic stroke. Cerebrovasc Dis 27(1):37–41
Foerch C, Curdt I, Yan B, Dvorak F, Hermans M, Berkefeld J et al (2006) Serum glial fibrillary acidic protein as a biomarker for intracerebral haemorrhage in patients with acute stroke. J Neurol Neurosurg Psychiatry 77(2):181–184
Unden J, Strandberg K, Malm J, Campbell E, Rosengren L, Stenflo J et al (2009) Explorative investigation of biomarkers of brain damage and coagulation system activation in clinical stroke differentiation. J Neurol 256(1):72–77
Foerch C, Niessner M, Back T, Bauerle M, De Marchis GM, Ferbert A et al (2012) Diagnostic accuracy of plasma glial fibrillary acidic protein for differentiating intracerebral hemorrhage and cerebral ischemia in patients with symptoms of acute stroke. Clin Chem 58(1):237–245
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G (1993) Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke 24(7):987–993
Brunkhorst R, Pfeilschifter W, Foerch C (2010) Astroglial proteins as diagnostic markers of acute intracerebral hemorrhage-pathophysiological background and clinical findings. Trans Stroke Res 1(4):246–251
Persson L, Hardemark HG, Bolander HG, Hillered L, Olsson Y (1989) Neurologic and neuropathologic outcome after middle cerebral artery occlusion in rats. Stroke 20(5):641–645
Herrmann M, Vos P, Wunderlich MT, de Bruijn CH, Lamers KJ (2000) Release of glial tissue-specific proteins after acute stroke: a comparative analysis of serum concentrations of protein S-100B and glial fibrillary acidic protein. Stroke 31(11):2670–2677
Niebroj-Dobosz I, Rafalowska J, Lukasiuk M, Pfeffer A, Mossakowski MJ (1994) Immunochemical analysis of some proteins in cerebrospinal fluid and serum of patients with ischemic strokes. Folia Neuropathol 32(3):129–137
Huttner HB, Kohrmann M, Tognoni E, Juttler E, Richter G, Dorfler A et al (2008) Clinical severity predicts time to hospital admission in patients with spontaneous intracerebral hemorrhage. Cerebrovasc Dis 25(6):533–538
Foerch C, du Mesnil R, de Rochemont O, Singer T, Neumann-Haefelin M, Buchkremer FE Zanella et al (2003) S100B as a surrogate marker for successful clot lysis in hyperacute middle cerebral artery occlusion. J Neurol Neurosurg Psychiatry 74(3):322–325
Wunderlich MT, Wallesch CW, Goertler M (2006) Release of glial fibrillary acidic protein is related to the neurovascular status in acute ischemic stroke. Eur J Neurol 13(10):1118–1123
Jung CS, Foerch C, Schanzer A, Heck A, Plate KH, Seifert V et al (2007) Serum GFAP is a diagnostic marker for glioblastoma multiforme. Brain 130(Pt 12):3336–3341
Pelinka LE, Kroepfl A, Schmidhammer R, Krenn M, Buchinger W, Redl H et al (2004) Glial fibrillary acidic protein in serum after traumatic brain injury and multiple trauma. J Trauma 57(5):1006–1012
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xiong, L., Yang, Y., Zhang, M. et al. The use of serum glial fibrillary acidic protein test as a promising tool for intracerebral hemorrhage diagnosis in Chinese patients and prediction of the short-term functional outcomes. Neurol Sci 36, 2081–2087 (2015). https://doi.org/10.1007/s10072-015-2317-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-015-2317-8