Abstract
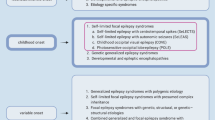
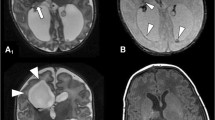
We report an unusual case of Parry–Romberg syndrome in which medically refractory focal epilepsy with ongoing epilepsia partialis continua (EPC) arose from the hemisphere contralateral to the side of facial atrophy. Unilateral cerebral involvement was confirmed by multi-modal brain imaging, as well as by electroencephalography (EEG) and magnetoencephalography (MEG). While in many cases of Parry–Romberg syndrome, the side of cerebral involvement is ipsilateral to that of the cutaneous lesion, these “discordant” exceptions imply that other yet undefined mechanisms may be responsible for the distribution of the cutaneous and cerebral pathologies.



Similar content being viewed by others
References
Stone J (2003) Parry–Romberg syndrome: a global survey of 205 patients using the Internet. Neurology 61:674–676
Garcia-de-la Torre I, Castello-Sendra J, Esgleyes-Ribot T, Martinez-Bonilla G, Guerrerosantos J, Fritzler MJ (1995) Autoantibodies in Parry–Romberg syndrome: a serologic study of 14 patients. J Rheumatol 22:73–77
Wolf SD, Verity MA (1974) Neurological complications of progressive facial hemiatrophy. J Neurol Neurosurg Psychiatry 37:997–1004
Carreno M, Donaire A, Barcelo MI et al (2007) Parry Romberg syndrome and linear scleroderma in coup de sabre mimicking Rasmussen encephalitis. Neurology 68:1308–1310
Shah JR, Juhasz C, Kupsky WJ et al (2003) Rasmussen encephalitis associated with Parry–Romberg syndrome. Neurology 61:395–397
Yamada K, Kizu O, Mori S et al (2003) Brain fiber tracking with clinically feasible diffusion-tensor MR imaging: initial experience. Radiology 227:295–301
Salayev KA, Nakasato N, Ishitobi M, Shamoto H, Kanno A, Iinuma K (2006) Spike orientation may predict epileptogenic side across cerebral sulci containing the estimated equivalent dipole. Clin Neurophysiol 117:1836–1843
Tinuper P, Plazzi G, Provini F et al (1992) Facial asymmetry in partial epilepsies. Epilepsia 33:1097–1100
Dupont S, Catala M, Hasboun D, Semah F, Baulac M (1997) Progressive facial hemiatrophy and epilepsy: a common underlying dysgenetic mechanism. Neurology 48:1013–1018
Moseley BD, Burrus TM, Mason TG, Shin C (2010) Neurological picture. Contralateral cutaneous and MRI findings in a patient with Parry–Romberg syndrome. J Neurol Neurosurg Psychiatry 81:1400–1401
Kister I, Inglese M, Laxer RM, Herbert J (2008) Neurologic manifestations of localized scleroderma: a case report and literature review. Neurology 71:1538–1545
Acknowledgments
Informed consent was obtained from the patient for the publication of his photograph and historical details in this paper.
Conflict of interest
Dr. Kakisaka, Dr. So, Dr. Jones, Dr. Wang, Dr. Mosher, Dr. Burgess report no disclosures. Dr. Alexopoulos have received research support from UCB and Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kakisaka, Y., So, N.K., Jones, S.E. et al. Intractable focal epilepsy contralateral to the side of facial atrophy in Parry–Romberg syndrome. Neurol Sci 33, 165–168 (2012). https://doi.org/10.1007/s10072-011-0643-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-011-0643-z