Abstract
There are four medical conditions characterized by high levels of ferritin, the macrophage activation syndrome (MAS), adult onset Still’ s disease (AOSD), catastrophic antiphospholipid syndrome (CAPS), and septic shock, that share similar clinical and laboratory features, suggesting a common pathogenic mechanism. This common syndrome entity is termed “the hyperferritinemic syndrome.” Here, we describe two different cases of hyperferritinemic syndrome triggered by Chikungunya fever virus infection: a 21-year-old female with SLE and a 32-year-old male patient who developed AOSD after the coinfection of dengue and Chikungunya viruses.
Similar content being viewed by others
Introduction
Ferritin, a major iron storage protein, is essential to iron homeostasis and is involved in a wide range of physiologic and pathologic processes. In clinical medicine, ferritin is predominantly used as a serum marker of total body iron stores and also such as an acute-phase reactant.
It is increasingly recognized that ferritin also plays a role in a multitude of other conditions, including inflammatory, neurodegenerative, and malignant diseases, even with a possible role in their pathogenesis [1].
Four well-recognized clinical conditions may be associated with high ferritin levels: the macrophage activation syndrome (MAS), adult-onset Still’s disease (AOSD), catastrophic antiphospholipid syndrome (CAPS), and septic shock. These disorders are characterized by life-threatening hyperinflammation with high levels of ferritin and cytokine storm, clinically presented as multiorgan failure. They share similar clinical signs, symptoms, and laboratory parameters. In addition, they also respond to similar therapies [2, 3]. Here, we report two cases of hyperferritinemic syndrome triggered by Chikungunya fever virus infection.
Patients and methods
Case report
Case 1
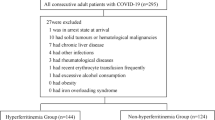
A 32-year-old male patient, with a previous history of typhoid fever 19 years ago was admitted at the ICU of our center by an 8-day clinical picture characterized by chills, disabling polyarthralgias associated to vomiting, sore throat, and non-dysenteric diarrheic stools. Two days prior to admission, he also presented generalized skin rash, edema, and choluric urine with decreased urinary output. At admission, the patient’s general status was poor with evidence of systemic inflammatory response (hypotension: blood pressure (BP) 95/56, tachycardia: heart rate (HR) 118 beats per minute, high respiratory rate (RR) 30 per minute, and fever (39 °C)). Dehydration was also documented and progressive edemas to anasarca developed within hours. On physical examination, a congestive oropharynx with petechiae on the palate, decreased breath sounds in both lung bases, widespread abdominal pain on palpation without signs of peritoneal irritation, mottled skin, and polyarthritis with marked limitation of the articular range of movements were also found. Laboratory investigation revealed abnormal white blood cell (WBC) count with leukemoid reaction and left deviation 35.150/uL (reference values 4800–11.000) (79 % neutrophils, lymphocytes 1 %, and bandemia) with normal hemoglobin (Hb) 13.6 g/dL (reference value between 14 and 17.5 g/dL) and platelet count in 246,000/uL (reference value 130,000–400,000). An elevated C-reactive protein (CRP) in 47 mg/dL (reference value 0–0.5) was also documented. Renal function tests were compatible with acute renal injury AKIN III with dialysis requirement: urea nitrogen 82.5 mg/dL (normal 8–23), creatinine 8.18 mg/dL (0.67–1.17), urinary protein/creatinine ratio 1.200 mg/dL, and blood arterial gases with metabolic acidosis. Alanine aminotransferase (AST) was also elevated in 91 U/L (0–40) while aspartate aminotransferase (ALT) 27 U/L (0–41), bilirubin, and gamma-glutamyl transpeptidase (GGT) were normal. Total creatine phosphokinase (CPK) 2130 UI/L (normal value up to 220) and lactic dehydrogenase (LDH) in 1765 U/L (135–225) were markedly elevated. Ceftriaxone and doxycycline were started due to the clinical suspicion of Weil’s syndrome/salmonellosis. Infectious tests including Leptospira IgM; HIV; VDRL; hepatitis A IgM; surface antigen VHB; VHC; blood, urine, and stool cultures; and thick-film and febrile antigen tests were all negative. On the contrary, dengue IgM and IgG serology were both positive. Due to an outbreak of Chikungunya infection in our region, a quantitative polymerase chain reaction for this virus was taken. The result was positive with 1,825,000 copies/mL (range of detection <500 copies). Thus, a diagnosis of coinfection of dengue and Chikungunya fever virus was made. The patient had torpid evolution, with fever persistence, leading to broadening of the antibiotic coverage (meropenem/vancomycin). The limb skin lesions progressed to bullous involvement. Over 1 week, fever and leukocytosis remained high despite antibiotic management. All cultures, including blood, urine, and stool cultures, were all negative. Drug fever reaction was discarded and the retest of quantitative polymerase chain reaction for Chikungunya virus (1 week separated from the initial test to rule out persistent viremia as the cause of fever) was undetectable, confirming the clearance of the virus. Due to poor improvement in clinical condition with persistence of renal disease, non-nephrotic proteinuria, leukemoid reaction, and high LDH level, a systemic disease was considered. Several hematological and rheumatic tests were done including a protein electrophoresis with no monoclonal peaks, a normal bone marrow aspiration-biopsy, and JAK2 mutation detection reported as negative. Rheumatoid factor, antinuclear antibodies (ANA), antibodies to the double-strain DNA (anti-DNAds) ANCAS, cryoglobulins, lupus anticoagulant, and anticardiolipins were all negative. On the other hand, the anti-RNP and anti-Sm were slightly high. These augmentations were considered as a false-positive reaction (attributed to an epiphenomenon). C3 and C4 fractions were diminished. Renal biopsy showed pigmentary nephropathy secondary to rhabdomyolysis. A PET-CT showed a reactive process due to the presence of hypermetabolic axillary and cervical lymph nodes, with periarticular and muscle inflammatory changes without evidence of malignancy (Fig. 1). Endoscopy and colonoscopy were both negative for malignancy. At week 3 since admission, the patient remained in a poor clinical condition presenting daily fever, sore throat, polyarthralgia, marked leukocytosis, and raised levels of C-reactive protein, transaminases, and serum ferritin in 5918 ng/mL, raising the suspicion of AOSD. According to Yamaguchi et al., this patient fulfilled the criteria for classification of AOSD, including four major criteria: high spiking fever, arthralgia, typical rash, and leukocytosis and four minor ones: sore throat, lymphadenopathy, liver dysfunction, and the absence of RF and antinuclear antibody. Methylprednisolone pulses for 3 days were started with rapid improvement of fever, skin lesions, and articular symptoms. Acute phase reactants improved as well. The patient was switched to oral prednisone and discharged from the hospital with subsequent steroid tapering and without recurrence.
Case 2
A 21-year-old female patient, with a previous history of 5 years of SLE in association to positive lupus anticoagulant and IgM and IgG anti-cardiolipins without obstetric or thrombotic events suggestive of APS, was admitted in our center with an acute disease. Her usual medication was based on azathioprine 150 mg/day, chloroquine 150 mg/day, and prednisone 25 mg/day. She was admitted for a 4-day clinical picture characterized by fever, polyarthritis of the hands and feet, oliguria with anasarca, diarrhea, and a widespread skin rash.
The patient was in regular state and she was admitted to the ICU with systemic inflammatory response (tachycardia with HR 143, RR 22, and fever −41 °C). Her BP was normal. The physical examination showed bilateral synovitis on the wrist, carpal, and proximal interphalangeal and ankle articulations. Anasarca, widespread livedo reticularis, and a bullous lesion in the intermammary region were also evidenced. The admission Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 6 indicating lupus activity. Laboratory test showed Hb 18.2 g/dL (normal 14–17.5), WBC with leukemoid reaction of 46,790 cells/uL (89.7 % neutrophils and 6.2 % lymphocytes), and platelets 137,000/uL. Acute-phase reactants were elevated with CRP in 34 mg/dL and procalcitonin in 26 ng/mL (reference value <0.5). In addition, renal and hepatic alterations were found with serum creatinine in 1.64 mg/dL, AST 93 IU/L, and normal ALT 37. LDH in 2314 U/L and lactic acid 8.08 mmol/L (range 0.5–2.22) were markedly elevated. Coagulation test were normal. Complement levels were decreased with C3, 61 mg/dL (90–180 mg/dL) and C4, 4 mg/dL (10–40). Extractable nuclear antigens (ENAS) and anti-DNAds (by IFI and EIA) were negative. Broad-range empiric antibiotics were started (meropenem, vancomycin, and fluconazole) with a previous take of blood cultures. An abdominopelvic CT and a Doppler of renal arteries and venous lower limbs were done with positive findings of nephropathy and splenic infarctions (Fig. 2).
In the next 24 h, her clinical condition worsened with metabolic acidosis, renal dysfunction (anuria without uremia with ultrafiltration requirement), and profound hypotension requiring vasopressors. Cardiac dysfunction was documented with 20–25 % of ejection fraction in the left ventricle and a positive quantitative troponin I 1.740 ng/mL (normal up to <0.030). Considering these findings, inotropic therapy (levosimendan) was initiated, without improvement. The patient deteriorated and developed an acute respiratory distress syndrome with requirement of mechanical ventilation. In addition, skin lesions progressed to purpuric lesions suggestive of livedoid vasculitis and necrotic lesions on the digits of hands and feet were evidenced. The laboratory test showed worsening of the systemic condition with a 3.4 g drop of Hb level (14.8 g/dL), positive direct Coomb’s test (++), raising of WBC to 68,390 (neutrophils 81 %, lymphocytes 6 %), and severe thrombocytopenia (platelets 40,000). The peripheral blood smear showed anisocytosis, microcytes, macrocytes, and slight poiquilocytosis, and toxic granulations with Döhle bodies. In addition, a raise on transaminases (AST 233 U/L, ALT 50 U/L) without jaundice was also evidenced. LDH (2156) and ferritin (50,025) were also elevated, and findings suggestive of disseminated intravascular coagulation (DIC) with TP 145 (INR 9.51) and aPTT 138, fibrinogen 123 (228–415) were evidenced.
All these findings configured the diagnosis of multiorgan dysfunction, secondary to suspected catastrophic APS (CAPS). Blood and urine culture were negative, in addition to serologic test for hepatitis B and C, dengue, leptospira, and Clostridium difficile. Due to an outbreak of Chikungunya infection, a quantitative polymerase chain reaction for this virus was taken. The result was positive with >5,000,000 copies/mL (range of detection <500 copies).
Considering that not specific antiviral treatments are available, the use of steroids and IV immunoglobulin (IVIG) was defined in order to treat the suspected CAPS. Forty-eight hours after admission and despite all support measures and two doses of IVIG, the clinical condition continues deteriorating, with cardiac arrest with unsuccessful reanimation maneuvers.
Discussion
Ferritin is a major intracellular iron storage protein, exists in two forms: an iron-free form named aporreferritin (composed of a nanocage of 24 assembled subunits of two kinds: H-subunit and L-subunit) and the iron-containing form termed holoferritin. Depending on the tissue type and physiologic status of the cell, the ratio of H- to L-subunits in ferritin can vary widely [1–3].
Their best-known function is storage of iron (captures the intracellular labile iron pool), and it is also an acute phase reactant, involved in an inflammatory response which includes oxidative stress-induced process [4].
The expression of ferritin is regulated at the transcriptional and posttranscriptional levels by various elements including iron, cytokines, chemokine production, lipopolysaccharide, hormones, growth factors, second messengers, hypoxia/hyperoxia, and oxidative stress [2].
Accumulating data have implicated a role for ferritin as a signaling molecule and direct mediator of the immune system with complex interaction with cytokines in the control of pro-inflammatory and anti-inflammatory mediators [3]. So ferritin can be either an immunosuppressive or a pro-inflammatory molecule. This ambivalence depends on the activation of different pathways through different receptors possibly employing different effectors (i.e., ferritin L versus H) and possibly in different contexts [2, 3].
Four clinical conditions may be associated with high ferritin levels: MAS, AOSD, CAPS, and septic shock. These disorders are characterized by life-threatening hyperinflammation with high levels of ferritin and cytokine storm, clinically presented as multiorgan failure. They share similar clinical signs, symptoms, and laboratory parameters. In addition, they also may respond to similar therapies [2, 3, 5].
The high levels of ferritin to be pathogenic require a second hit, like a pro-inflammatory environment, a specific infection, or maybe a particular genetic background [2, 3, 5]. Here, we describe two cases of a systemic disease characterized by high ferritin levels triggered by the same agent: a Chikungunya infection, supporting even more the previous findings.
Virus infection is a primary factor that has been implicated in the initiation of autoimmune diseases. Infection triggers a robust and usually well-coordinated immune response that is critical for viral clearance. However, in some instances, immune regulatory mechanisms may falter, culminating in the breakdown of self-tolerance, resulting in immune-mediated attack directed against both viral and self-antigens. Traditionally, cross-reactive T cell recognition, known as molecular mimicry, as well as bystander T cell activation, culminating in epitope spreading, has been the predominant mechanisms elucidated through which infection may culminate in a T cell-mediated autoimmune response [6]. Some viral infections are reported as etiologic and precipitating factors of AOSD [7] and CASP [8].
The Chikungunya virus is a single-stranded RNA mosquito-borne alphavirus of the family Togaviridae [9]. The illness was described to have two identifiable phases: the first (within 10 days of onset) characterized by typically rapid-onset febrile disease, intense asthenia, arthralgia, headache, conjunctivitis, and maculopapular rash mainly in the trunk (sometimes it can be bullous). The second and more chronic phase consists in morning stiffness and persistent arthritis/arthralgias, which may last for months to years. Atypical and even fatal presentations are higher in immunocompromised individuals. Up until now, the arboviral infections have been considered as well-recognized but rare and arcane causes of virally mediated rheumatic complications, arthritis mimicking rheumatoid arthritis mostly, but little is known about this infection triggering or complicating other rheumatologic conditions [10].
It is difficult to discern if the very high ferritin levels in these clinical conditions are not just the product of the inflammation like an innocent bystander or may have a pathogenic role. Possibly, in an inflammatory environment, as observed in these diseases, the huge levels of ferritin may be involved in some sort of a loop mechanism where ferritin’ s inflammatory proprieties are exacerbated, leading to an extreme expression of additional inflammatory mediators that are characteristic in the cytokine storm [4].
References
Knovich MA, Storey JA, Coffman LG, Torti SV, Torti FM (2009) Ferritin for the clinician. Blood Rev 23(3):95–104
Rosário C, Zandman-Goddard G, Meyron-Holtz EG, D’Cruz DP, Shoenfeld Y (2013) The hyperferritinemic syndrome: macrophage activation syndrome, Still’s disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med 11:185–195
Rosário C, Shoenfeld Y, Hon F (2014) The hyperferritinemic syndrome. IMAJ 16:10–11
Mehta B, Efthimiou P (2012) Ferritin in adult-onset Still’s disease: just a useful innocent bystander? Int J Inflam 2012:254858
Agmon-Levin N, Rosário C, Katz B-SP, Zandman-Goddard G, Meroni P, Cervera R et al (2013) Ferritin in the antiphospholipid syndrome and its catastrophic variant (cAPS). Lupus 22(13):1327–1335
Getts DR, Chastain EM, Terry RL, Miller SD (2013) Virus infection, antiviral immunity, and autoimmunity. Immunol Rev 255(1):197–209
Wouters JM, van der Veen J, van de Putte LB, de Rooij DJ (1988) Adult onset Still’s disease and viral infections. Ann Rheum Dis 47(9):764–767
Ortega-Hernandez O-D, Agmon-Levin N, Blank M, Asherson RA, Shoenfeld Y (2009) The physiopathology of the catastrophic antiphospholipid (Asherson’s) syndrome: compelling evidence. J Autoimmun 32(1):1–6
Campion EW, Weaver SC, Lecuit M (2015) Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med 372(13):1231–1239
Calabrese LH (2008) Emerging viral infections and arthritis: the role of the rheumatologist. Nat Clin Pract Rheumatol 4(1):2–3
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Betancur, JF., Navarro, EP., Echeverry, A. et al. Hyperferritinemic syndrome: Still’s disease and catastrophic antiphospholipid syndrome triggered by fulminant Chikungunya infection: a case report of two patients. Clin Rheumatol 34, 1989–1992 (2015). https://doi.org/10.1007/s10067-015-3040-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-015-3040-9