Abstract
Purpose
Laparoscopic total extra-peritoneal hernia repair (TEP) is associated with less post-operative pain and earlier return to normal activity compared to open hernia repair (OHP). Despite this, post-operative pain remains a major issue. The aim of this double-blinded randomized controlled trial was to identify whether the instillation of local anaesthetic in the pre-peritoneal space improves pain scores following TEP.
Methods
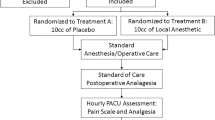
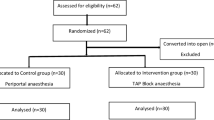
One hundred patients undergoing laparoscopic total pre-peritoneal hernia repair (TEP) between the years of 2009–2014 were included. Patients were randomly assigned to receive either 20 mL of normal saline or 0.25% bupivacaine with adrenaline. Visual analogue scores (VAS 0–10) were recorded post-operatively at the 4 h, 1 day, 2 weeks, and 6 week mark. Secondary endpoints included complications, time to discharge, and return to normal activity.
Results
51 patients were allocated to the local group. 49 patients were allocated to the placebo group. The baseline characteristics and demographics of patients in both groups were comparable. Patients in the local group had similar VAS scores compared to the placebo group at both 4 h (1.1 vs. 1.4, respectively; p = 0.19) and 24 h (2.1 vs. 2.3; p = 0.63). No statistically significant difference noted in other primary and secondary outcomes.
Conclusion
Although the concept of pre-peritoneal local anaesthetic instillation following laparoscopic TEP is attractive, this appropriately powered study has failed to show any advantage in pain scores at 4 and 24 h. The pain scores recorded, however, were remarkably low in both groups.


Similar content being viewed by others
References
McCormack K, Scott NW, Go PM, Ross S, Grant AM, Collaboration EUHT (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD001785. doi:10.1002/14651858.CD001785
Wake B, Perez J, Fraser C, Cook J, McIntosh E, Vale L, Grant A (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess (Winchester, England) 9(14):1–203 (iii–iv)
Bracale U, Melillo P, Pignata G, Di Salvo E, Rovani M, Merola G, Pecchia L (2012) Which is the best laparoscopic approach for inguinal hernia repair: TEP or TAPP? A systematic review of the literature with a network meta-analysis. Surg Endosc 26(12):3355–3366. doi:10.1007/s00464-012-2382-5
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD004703. doi:10.1002/14651858.CD004703.pub2
Krishna A, Misra MC, Bansal VK, Kumar S, Rajeshwari S, Chabra A (2012) Laparoscopic inguinal hernia repair: transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trial. Surg Endosc 26(3):639–649. doi:10.1007/s00464-011-1931-7
O’Riordain DS, Kelly P, Horgan PG, Keane FB, Tanner WA (1998) A randomized controlled trial of extraperitoneal bupivacaine analgesia in laparoscopic hernia repair. Am J Surg 176(3):254–257
O’Riordain DS, Kelly P, Horgan PG, Keane FB, Tanner WA (1999) Laparoscopic extraperitoneal inguinal hernia repair in the day-care setting. Surg Endosc 13(9):914–917
Ramshaw BJ, Tucker JG, Duncan TD, Heithold D, Garcha I, Mason EM, Wilson JP, Lucas GW (1996) Technical considerations of the different approaches to laparoscopic herniorrhaphy: an analysis of 500 cases. Am Surg 62(1):69–72
Felix EL, Michas CA, Gonzalez MH Jr (1995) Laparoscopic hernioplasty. TAPP vs TEP. Surg Endosc 9(9):984–989
Tong YS, Wu CC, Bai CH, Lee HC, Liang HH, Kuo LJ, Wei PL, Tam KW (2014) Effect of extraperitoneal bupivacaine analgesia in laparoscopic inguinal hernia repair: a meta-analysis of randomized controlled trials. Hernia 18(2):177–183. doi:10.1007/s10029-013-1100-0
Abbas MH, Hamade A, Choudhry MN, Hamza N, Nadeem R, Ammori BJ (2010) Infiltration of wounds and extraperitoneal space with local anesthetic in patients undergoing laparoscopic totally extraperitoneal repair of unilateral inguinal hernias: a randomized double-blind placebo-controlled trial. Scand J Surg 99(1):18–23
Suvikapakornkul R, Valaivarangkul P, Noiwan P, Phansukphon T (2009) A randomized controlled trial of preperitoneal bupivacaine instillation for reducing pain following laparoscopic inguinal herniorrhaphy. Surg Innov 16(2):117–123. doi:10.1177/1553350609334128
Lau H, Patil NG, Yuen WK, Lee F (2002) Urinary retention following endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc 16(11):1547–1550. doi:10.1007/s00464-001-8292-6
Lau H, Lee F (2003) Seroma following endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 17(11):1773–1777. doi:10.1007/s00464-002-8771-4
Bar-Dayan A, Natour M, Bar-Zakai B, Zmora O, Shabtai M, Ayalon A, Kuriansky J (2004) Preperitoneal bupivacaine attenuates pain following laparoscopic inguinal hernia repair. Surg Endosc 18(7):1079–1081. doi:10.1007/s00464-003-8214-x
Hon SF, Poon CM, Leong HT, Tang YC (2009) Pre-emptive infiltration of Bupivacaine in laparoscopic total extraperitoneal hernioplasty: a randomized controlled trial. Hernia 13(1):53–56. doi:10.1007/s10029-008-0422-9
Palmes D, Rottgermann S, Classen C, Haier J, Horstmann R (2007) Randomized clinical trial of the influence of intraperitoneal local anaesthesia on pain after laparoscopic surgery. Br J Surg 94(7):824–832. doi:10.1002/bjs.5810
Pasqualucci A, de Angelis V, Contardo R, Colo F, Terrosu G, Donini A, Pasetto A, Bresadola F (1996) Preemptive analgesia: intraperitoneal local anesthetic in laparoscopic cholecystectomy. A randomized, double-blind, placebo-controlled study. Anesthesiology 85(1):11–20
Fischer S, Troidl H, MacLean AA, Koehler L, Paul A (2000) Prospective double-blind randomised study of a new regimen of pre-emptive analgesia for inguinal hernia repair: evaluation of postoperative pain course. Eur J Surg 166(7):545–551. doi:10.1080/110241500750008619
Barczynski M, Konturek A, Herman RM (2006) Superiority of preemptive analgesia with intraperitoneal instillation of bupivacaine before rather than after the creation of pneumoperitoneum for laparoscopic cholecystectomy: a randomized, double-blind, placebo-controlled study. Surg Endosc 20(7):1088–1093. doi:10.1007/s00464-005-0458-1
Lau H, Patil NG, Lee F, Yuen WK (2002) A prospective trial of analgesia following endoscopic totally extraperitoneal (TEP) inguinal hernioplasty. Surg Endosc 16(1):159–162. doi:10.1007/s00464-001-8106-x
Saff GN, Marks RA, Kuroda M, Rozan JP, Hertz R (1998) Analgesic effect of bupivacaine on extraperitoneal laparoscopic hernia repair. Anesth Analg 87(2):377–381
Clark WC, Yang JC, Tsui SL, Ng KF, Bennett Clark S (2002) Unidimensional pain rating scales: a multidimensional affect and pain survey (MAPS) analysis of what they really measure. Pain 98(3):241–247
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SK declares no conflicts of interest, MR declares no conflicts of interest, LP declares no conflicts of interest, and MHM declares no conflicts of interest.
Funding
No financial disclosures to make.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
I hereby undersign and certificate that this article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent obtained from every patient prior to inclusion
Rights and permissions
About this article
Cite this article
Kulasegaran, S., Rohan, M., Pearless, L. et al. Pre-peritoneal local anaesthetic does not reduce post-operative pain in laparoscopic total extra-peritoneal inguinal hernia repair: double-blinded randomized controlled trial. Hernia 21, 879–885 (2017). https://doi.org/10.1007/s10029-017-1672-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1672-1