Abstract
Objective
To demonstrate improved healing of a midline laparotomy after application of mesenchymal stromal cells and platelet-rich plasma on a collagen matrix and introduce a potential cellular-based therapy for the prevention of incisional hernia formation.
Background
Up to 10 % of laparotomies are complicated by postoperative incisional hernias. Despite continuous improvements in surgical technique and technology, hernia rates have remained constant. Cell-based therapies focused on augmentation of the body’s natural healing properties could reduce hernia formation.
Methods
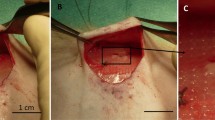
Midline laparotomies were performed on 42 Lewis rats. Three groups were studied: (1) primary repair only, (2) primary repair with CollaTape™ (CoTa) overlay and platelet-rich plasma (PRP), and (3) primary repair with CoTa overlay and PRP and bone marrow-derived mesenchymal stromal cells (BM-MSCs). Abdominal wall fascia was recovered at 4 and 8 weeks in each group. Biomechanical testing and histological evaluation was performed.
Results
At 4 weeks, there was a twofold increase in tensile strength between groups 1 and 2 and a fourfold increase between groups 1 and 3 (p < 0.001). Group 3 had a 320 % increase in total energy absorption at 4 weeks compared to group 1 and a 142 % increase at 8 weeks (p < 0.001). Vascularization and collagen abundance were significantly increased in group 3 at both time points.
Conclusion
The addition of BM-MSCs, PRP, and CoTa led to a marked improvement in abdominal wall strength and energy absorption. Histologic evaluation confirmed increased vascularity and collagen abundance consistent with the biomechanical findings. Application of this therapy may ultimately reduce incisional hernia formation.




Similar content being viewed by others
References
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Blomstedt B, Welin-Berger T (1972) Incisional hernias: a comparison between midline, oblique and transrectal incisions. Acta Chir Scand 138:275–278
Ellis H, Bucknall TE, Cox PJ (1985) Abdominal incisions and their closure. Curr Probl Surg 22:1–51
Schoetz DJ, Coller JA, Veidenheimer MC (1988) Closure of abdominal wounds with polydioxanone: a prospective study. Arch Surg 123:72–74
Bucknall TE, Cox PJ, Ellis H (1982) Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J Clin Res Ed 284:931–933
Burger JW, Luijendijk RW, Hop WC et al (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
van der Linden FT, van Vroonhoven TJ (1988) Long-term results after surgical correction of incisional hernia. Neth J Surg 40:127–129
Franz MG, Steed DL, Robson MC (2007) Optimizing healing of the acute wound by minimizing complications. Curr Probl Surg 44:691–763
Hodgson NC, Malthaner RA, Ostbye T (2000) The search for an ideal method of abdominal facial closure: a meta-analysis. Ann Surg 231:436–442
Hsiao W, Young K, Wang S et al (2000) Incisional hernia after laparotomy: prospective randomized comparison between early-absorbable and late-absorbable suture materials. World J Surg 24:747–752
Robson MC, Mustoe TA, Hunt TK (1998) The future of recombinant growth factors in wound healing. Am J Surg 176(2A):80S–82S
Robson MC, Phillips LG, Thomason A et al (1992) Platelet-derived growth factor BB for the treatment of chronic pressure ulcers. Lancet 339:23–25
Tsang MW, Wong WK, Hung CS et al (2003) Human epidermal growth factor enhances healing of diabetic foot ulcers. Diabetes Care 26:1856–1861
Kimura A, Ogata H, Yazawa M et al (2005) The effects of platelet-rich plasma on cutaneous incisional wound healing in rats. J Dermatol Sci 40:205–208
Kakudo N, Minakata T, Mitsui T et al (2008) Proliferation-promoting effect of platelet-rich plasma on human adipose-derived stem cells and human dermal fibroblasts. Plast Reconstr Surg 122:1352–1360
Oprea WE, Karp JM, Hosseini MM et al (2003) Effect of platelet releasate on bone cell migration and recruitment in vitro. J Craniofac Surg 14:292–300
Ahmed MR, Vairamuthu S, Shafiuzama M et al (2005) Microwave irradiated collagen tubes as a better matrix for peripheral nerve regeneration. Brain Res 1046:55–67
Lin H, Chen B, Sun W et al (2006) The effect of collagen-targeting platelet-derived growth factor on cellularization and vascularization of collagen scaffolds. Biomaterials 27:5708–5714
Boccafoschi F, Habermehl J, Vesentini S et al (2005) Biological performances of collagen-based scaffolds for vascular tissue engineering. Biomaterials 26:7410–7417
Jung U, Kim S, Kim C et al (2007) Effect of chitosan with absorbable collagen sponge carrier on bone regeneration in rat calvarial defect model. Curr Appl Phys 7S1:68–70
Friedenstein AJ (1976) Precursor cells of mechanocytes. Int Rev Cytol 47:327–359
Pittenger MF, Mackay AM, Beck SC et al (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Badiavas EV, Abedi M, Butmarc J et al (2003) Participation of bone marrow derived cells in cutaneous wound healing. J Cell Physiol 196:245–250
Badiavas EV, Falanga V (2003) Treatment of chronic wounds with bone marrow-derived cells. Arch Dermatol 139:510–516
Falanga V, Iwamoto S, Chartier M et al (2007) Autologous bone marrow-derived cultured mesenchymal stem cells delivered in a fibrin spray accelerate healing in murine and human cutaneous wounds. Tissue Eng 13:1299–1312
Marie H, Zhang Y, Heffner J et al (2010) Biomechanical and elastographic analysis of mesenchymal stromal cell treated tissue following surgery. J Biomech Eng 132:074503
Maekawa Y, Yagi K, Nonomura A et al (2003) A tetrazolium-based colorimetric assay for metabolic activity of stored blood platelets. Thromb Res 109:307–314
Dai W, Hale SL, Martin BJ et al (2005) Allogeneic mesenchymal stem cell transplantation in postinfarcted rat myocardium: short- and long-term effects. Circulation 112:214–223
Javazon EH, Colter DC, Schwarz EJ et al (2001) Rat marrow stromal cells are more sensitive to plating density and expand more rapidly from single-cell-derived colonies than human marrow stromal cells. Stem Cells 19:219–225
Dubay DA, Wang X, Adamson B et al (2006) Mesh incisional herniorrhaphy increase abdominal wall elastic properties: a mechanism for decreased hernia recurrences in comparison with suture repair. Surgery 140:14–24
Stanwix MG, Nam AJ, Hui-Chou HG et al (2011) Abdominal ventral hernia repair with current biological prostheses. Ann Plast Surg 66:403–409
Badylak S, Kokini K, Tullius B et al (2002) Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 103:190–202
Konstantinovic ML, Lagae P, Zheng F et al (2005) Comparison of host response to polypropylene and non-cross-linked porcine small intestine serosal-derived collagen implants in a rat model. BJOG 112:1554–1560
Steed DL (1998) Modifying the wound healing response with exogenous growth factors. Clin Plast Surg 25:397–405
De Leon J, Driver V, Fylling C (2011) The clinical relevance of treating chronic wounds with an enhanced near-physiologic concentration of platelet-rich plasma gel. Adv. Skin Wound Care 8:357–368
Pietramaggiori G, Scherer SS, Mathews JC et al (2008) Healing modulation induced by freeze-dried platelet-rich plasma and micronized allogenic dermis in a diabetic wound model. Wound Repair Regen 16:218–225
Smith SE, Roukis TS (2009) Bone and wound healing augmentation with platelet-rich plasma. Clin Podiatric Med Surg 26:559–588
Luitaud C, Laflamme C, Semlali A et al (2007) Development of an engineering autologous platal mucosa-like tissue for potential clinical applications. J Biomed Mater Res B Appl Biomater 83:554–561
Zhao S, Wehner R, Bornhauser M et al (2010) Immunomodulatory properties of mesenchymal stromal cells and their therapeutic consequences for immune-mediated disorders. Stem Cells Dev 19:607–614
Jeon YK, Jang YH, Yoo DR et al (2010) Mesenchymal stem cells’ interaction with skin: wound-healing effect on fibroblast cells and skin tissue. Wound Rep Reg 18:655–661
Fathke C, Wilson L, Hutter J et al (2004) Contribution of bone marrow-derived cells to skin: collagen deposition and wound repair. Stem Cells 22:812–822
Goedecke A, Wobus M, Krech M et al (2011) Differential effect of platelet-rich plasma and fetal calf serum on bone marrow-derived human mesenchymal stromal cells expanded in vitro. J Tissue Eng Regen Med 5:648–654
Wu Y, Chen L, Scott PG et al (2007) Mesenchymal stem cells enhance wound healing through differentiation and angiogenesis. Stem Cells 25:2648–2659
Lacci KM, Dardik A (2010) Platelet-rich plasma: support for its use in wound Healing. Yale J Biol Med 83:1–9
McFarlin K, Gao X, Yong BL et al (2006) Bone marrow-derived mesenchymal stromal cells accelerate wound healing in the rat. Wound Repair Regen 14:471–484
Schrepfer S, Deuse T, Reichenspurner H et al (2007) Stem cell transplantation: the lung barrier. Transplant Proc 39:573–576
Kidd S, Spaeth E, Dembinski JL et al (2009) Direct evidence of mesenchymal stem cell tropism for tumor and wounding microenvironments using in vivo bioluminescent imaging. Stem Cells 27:2614–2623
Acknowledgments
Funding was provided by the American Hernia Society/Lifestyle Resident Research Award 2010.
Conflict of interest
There are no other disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heffner, J.J., Holmes, J.W., Ferrari, J.P. et al. Bone marrow-derived mesenchymal stromal cells and platelet-rich plasma on a collagen matrix to improve fascial healing. Hernia 16, 677–687 (2012). https://doi.org/10.1007/s10029-012-0941-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0941-2