Abstract
Purpose
Establishing the existence of inguinal neuritis, and defining patterns of nerve involvement in primary inguinal hernia repair.
Methods
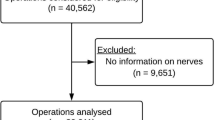
A retrospective chart review of 100 consecutive primary inguinal hernia repairs by Lichtenstein technique with frequent ilioinguinal nerve removal was performed. Nerves suspected of containing neuritis had been sent for histological examination. Objective clinical parameters and nerve pathology reports were reviewed. An independent biostatistician reviewed the data.
Results
There were 34 cases of inguinal neuritis in these primary inguinal hernia repairs. The nerve most affected in primary repairs was the ilioinguinal nerve, accounting for 88% of the neuritis cases. Inguinal neuritis occurred mainly at the external oblique neuroperforatum—where the nerve pierces the external oblique fascia, accounting for 83% in primary repair. The only clinical parameter with statistical significance was hernia laterality (P = 0.04), 46% of the patients who had a hernia on the left also had inguinal neuritis.
Conclusion
The overall incidence of inguinal neuritis was 34% in primary inguinal hernia repairs. The ilioinguinal nerve was most commonly affected in these primary inguinal hernia repairs, and inguinal neuritis was most likely to occur at the external oblique neuroperforatum.







Similar content being viewed by others
References
Madura JA, Madura JA 2nd, Copper CM, Worth RM (2004) Inguinal neurectomy for inguinal nerve entrapment: an experience with 100 patients. Am J Surg 189(3):283–287. doi:10.1016/j.amjsurg.2004.11.015
Aasvang E, Kehlet H (2004) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95(1):69–76. doi:10.1093/bja/aei019
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367(9522):1618–1625. doi:10.1016/S0140-6736(06)68700-X
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg (2):212–219. doi:10.1097/01.sla.0000218081.53940.01
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2002) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19(1):48–54
Ferzli GS, Edwards E, Al-Khoury G, Hardin R (2007) Postherniorrhaphy groin pain and how to avoid it. Surg Clin North Am 88(1):203–216. doi:10.1016/j.suc.2007.10.006 (x–xi)
Dittrick GW, Ridl K, Kuhn JA, McCarty TM (2004) Routine ilioinguinal nerve excision in inguinal hernia repairs. Am J Surg 188(6):736–740. doi:10.1016/j.amjsurg.2004.08.039
Mui WL, Ng CS, Fung TM, Cheung FK, Wong CM, Ma TH, Bn MY, Ng EK (2006) Prophylactic ilioinguinal neurectomy in open inguinal hernia repair: a double-blind randomized controlled trial. Ann Surg 244(1):27–33. doi:10.1097/01.sla.0000217691.81562.7e
Malekpour F, Mirhashemi SH, Hajinasrolah E, Salehi N, Khoshkar A, Kolahi AA (2007) Ilioinguinal nerve excision in open mesh repair of inguinal hernia—results of a randomized clinical trial: simple solution for a difficult problem. Am J Surg 195(6):735–740. doi:10.1016/j.amjsurg.2007.09.03 Epub 2008 Apr 28
Vuilleumier H, Hübner M, Demartines N (2009) Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg. (4):841–845. doi:10.1007/s00268-008-9869-1
Scheithauer B, Woodruff J, Erlandson R (1997) Reactive lesions. In: Rosai J (ed) Atlas of tumor pathology, 3rd edn. Washington DC, pp 37–41
Jefferson D, Neary D, Eames R (1981) Renaut body distribution at site of human peripheral nerve entrapment. J Neurol Sci 49:19–29. doi:10.1016/0022-510X(81)90184-2
Bartlett DC, Porter C, Kingsnorth AN (2007) A pragmatic approach to cutaneous nerve division during open inguinal hernia repair. Hernia. 11(3):243–246. (Epub 2007 Mar 20). doi:10.1007/s10029-007-0209-4
Alfieri S, Rotondi F, Di Giorgio A, Fumagalli U, Salzano A, Di Miceli D, Ridolfini MP, Sgagari A, Doglietto G, Groin Pain Trial Group (2006) Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg 243(4):553–558
Kim D, Midha R, Murovic J, Spinner R (2008) Operative care and techniques. In: Pioli S (ed) Kline and Hudson’s nerve injuries: operative results for major nerve injuries, entrapments, and tumors, 2nd edn. Saunders, Philadelphia
Tindall G, Cooper P, Barrow D (1996) The practice of neurosurgery, vol 3. Williams and Wilkins, Baltimore, pp 3155–3156
Winn R, Youmans J (2004) Youman’s neurological surgery, 5th edn, vol 4. Saunders, Philadelphia
Acknowledgments
Philip Good, biostatistician, has been very helpful in understanding the significance of our data. Pathologists were Larry O’Bryant and Eric Arntson.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wright, R.C., Sanders, E. Inguinal neuritis is common in primary inguinal hernia. Hernia 15, 393–398 (2011). https://doi.org/10.1007/s10029-011-0807-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-011-0807-z