Abstract
Purpose
Oral submucous fibrosis is a disease of an Indian subcontinent with obscure aetiology and poorly treated with varying signs and symptoms. OSMF occurs at any age but is most commonly seen in teenagers and adults in the age ranging between 16 and 35 years. A number of surgical treatments have been used for the treatment of oral submucous fibrosis with unpredictable results.
Patients and method
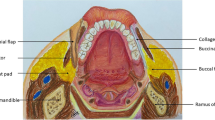
In this study, 220 patients were randomly divided into two groups with mouth opening less than 16 mm and evaluated with immediate and delayed aggressive physiotherapy with buccal fat pad interposition after fibrotomy. Group A (n = 110) patients underwent aggressive mouth opening exercise from the next postoperative day while in group B (n = 110), patients underwent physiotherapy 7th day postoperatively. Pain and discomfort, mucosalization, infection, flap dehiscence and necrosis were noted. Patients were followed for 1 year on a regular interval basis.
Results
At the end of 1-year follow up, the post-operative mean mouth opening in group A was 38.63 mm and 34.19 mm in group B. In group A, the immediate physiotherapy results in mild to moderate pain and discomfort to the patients as compared to no apparent pain in the group B. The mean mucosalization time in group A and group B was 4.2 and 5.1 weeks, respectively. Postoperatively, all patients achieve satisfactory mouth opening.
Conclusion
Immediate aggressive physiotherapy yields a comparatively superior result than delayed physiotherapy with respect to mouth opening in 1 year of follow-up.










Similar content being viewed by others
References
Sirsat SM, Khanolkar VR (1962) Submucous fibrosis of the palate and pillars of the fauces. J Med Science 16:189–197
Gupta D, Sharma SC (1988) Oral submucous fibrosis – a new treatment regimen. J Oral MaxillofacSurg 46:830–833
Joshi SG (1953) Submucous fibrosis of the palate and pillars. Indian Journal of otolaryngeal 4:1–4
Paymaster JC (1956) Cancer of the buccal mucosa: clinical study of 650 cases in Indian patients. Cancer 9:431–435
Borle RM, Borle SR (1991) Management of oral submucous fibrosis. J Oral MaxillofacSurg 49:788–791
Lambade P, Dawane P, Thorat P (2014) Oral submucous fibrosis— a treatment protocol based on clinical study of 100 patients in Central India. J Oral MaxillofacSurg. doi:10.1007/s10006-014-0478-x
Khanna JN, Andrade NN (1995) Oral submucous fibrosis: a new concept in surgical management. Report of 100 cases. Int J Oral MaxillofacSurg 24:433–439
Bande CR et al (2012) Extended nasolabial flap compared with the platysmamyocutaneous muscle flap for reconstruction of intraoral defects after release of oral submucous fibrosis: a comparative study. Br J Oral MaxillofacSurg. doi:10.1016/j.bjoms.2012.02.015
Wei FC, Chang YM, Kildal M, Tsang WS, Chen HC (2001) Bilateral small radial forearm flaps for the reconstruction of buccal mucosa after surgical release of submucosal fibrosis: a new reliable approach. PlastReconstrSurg 107:1679–1683
Scammon RE (1919) On the development and finer structure of the corpus adiposumbuccae. Anat Rec 15:267–287
Egyedi P (1977) Utilisation of the buccal fat pad for closure of oro-antral and/or oro-nasal communications. J CraniomaxillofacSurg 5:241–244
Dubien B, Jackson IT, Halim A, Ferreira M (1989) Anatomy of the buccal fat pad and its clinical significance. Plast Reconstr Surg 257–63
Lambade P, Meshram V, Thorat P, Dawane P, Thorat A, Rajkhokar D (2016) Efficacy of nasolabial flap in reconstruction of fibrotomy defect in surgical management of oral submucous fibrosis: a prospective study. Oral MaxillofacSurg. doi:10.1007/s10006015-0519-0
Lambade P, Dawane P, Thorat A (2016) Efficacy of buccal fat pad in the surgical management of oral submucous fibrosis: a prospective study. Oral MaxillofacSurg. doi:10.1007/s10006-016-0546-5
Tideman H, Bosanquet A, Scott J (1986) Use of the buccal fat pad as a pedicled graft. J Oral MaxillofacSurg 44:435–440
Fujimura N, Nagura H, Enomoto S (1990) Grafting of the buccal fat pad into palatal defects. J CraniomaxillofacSurg 18:219–222
Amin MA, Bailey BM, Swinson B, Witherow H (2005) Use of the buccal fat pad in the reconstruction and prosthetic rehabilitation of oncological maxillary defects. Br J Oral MaxillofacSurg 43:148–154
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study obtained approval from an institutional ethical committee.
Conflict of interest
The authors declare that they have no competing interests.
Funding source
None.
Rights and permissions
About this article
Cite this article
Bande, C., Dawane, P., Gupta, M.K. et al. Immediate versus delayed aggressive physical therapy following buccal fat pad interposition in oral submucous fibrosis—a prospective study in Central India. Oral Maxillofac Surg 20, 397–403 (2016). https://doi.org/10.1007/s10006-016-0580-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-016-0580-3