Abstract
This study aimed to examine the impact of maternal depressive symptoms trajectories on 15-year-old adolescents’ self-esteem and emotion regulation and test the mediating role of child maltreatment in this association. The 2004 Pelotas Birth Cohort is an ongoing cohort study originally comprised of 4231 live births in a southern Brazilian city. We examined a subsample of 1949 adolescents at age 15 years. Maternal depressive symptoms were assessed using the Edinburgh Postnatal Depression Scale. Trajectories of maternal depression from 3 months until the 11-year follow-up were calculated using a group-based modeling approach. Child maltreatment at age 11 years was measured using the parent-report version of the Parent–Child Conflict Tactics Scale. Adolescent outcomes at age 15 years were assessed by the self-report version of the Rosenberg Self-esteem Scale and the Emotion Regulation Index for Children and Adolescents. Path model analysis was conducted using a structural equation modeling framework in Mplus software. All maternal depression trajectories were negatively associated with offspring self-esteem and emotion regulation compared to the reference group (low depression trajectory). There was a significant indirect effect of maternal depression trajectories on emotion regulation mediated via child maltreatment. No evidence of moderation by sex was found for any pathway. The effects of maternal depression on adolescents’ emotion regulation are partly mediated by child maltreatment at age 11.
Similar content being viewed by others
Introduction
Adolescence is characterized by important changes in multiple domains of functioning, including physical, psychological and social transformations [1]. The onset of puberty is a biologically complex process that affects adolescent's growth, behavior, and emotional development [1]. Similar to early childhood, adolescence represents a sensitive period for later mental health and emotional well-being, with many risky and protective behaviors starting in this phase of life [1, 2]. However, in contrast to child health, research on adolescent health is less consolidated and many of the specific needs of this age group are still not properly addressed in both clinical practice and scientific study [1].
Previous investigations demonstrated that emotion regulation and self-esteem are important psychological resources related to well-being and successful adaptation during adolescence [3,4,5]. Emotion regulation has been proposed as a core component of socioemotional adjustment and comprises intrinsic processes that allow individuals to monitor, evaluate, and modify their emotional responses [4]. Self-esteem is conceived as an individual's subjective evaluation of the self and involves feelings of self-acceptance and worthiness as a person [5]. Individuals presenting an adaptive level of emotion regulation and positive feelings of self-worth are more likely to experience well-being, life satisfaction, and academic success [4, 5]. Conversely, emotion dysregulation and low self-esteem were associated with several negative outcomes, including poorer physical health, difficulties in social relationships, and an increased vulnerability to mental health problems [6, 7]. The developmental challenges occurring during adolescence make this an opportune period to investigate the predictors of emotion regulation and self-esteem development [8, 9].
The exposure to maternal depression is an important factor related to adolescents’ impaired psychosocial functioning [10, 11]. Maternal depression is a common psychiatric disorder, affecting approximately 20% of women globally, and represents a huge burden for women’s and children’s health and well-being [11]. The mother–child relationship often constitutes the most salient social experience in early childhood, influencing and shaping the trajectories of socioemotional development for decades [12]. Interactions within the family contain implicit and explicit information serving as the foundation for the child's lifelong interpersonal relations and self-evaluation [13, 14]. The quality of the family environment may be greatly affected by caregivers’ mental health problems [13, 14]. Indeed, compared to non-depressed controls, depressed mothers tend to demonstrate more irritable or sad affections, express more negative feelings toward their children, have more difficulty in engaging in consistent and positive disciplinary strategies, and experience more distress during interactions with their children [12].
Although the deleterious effects of maternal depression on adolescent socioemotional competencies are strongly supported by previous studies, the pathways linking these are still poorly examined [10, 13]. Investigating the mechanisms between these variables is important to focus on potential intervention targets aiming to reduce the harmful consequences of maternal depression on vulnerable adolescents [13]. One possible mechanism is suggested by evidence that depressed mothers are more likely to adopt negative disciplinary strategies when managing conflicts with their children and are at greater risk of perpetrating physical aggression and psychological abuse [9, 15]. Additionally, numerous studies show that experiencing any kind of maltreatment by parents severely impacts children’s mental health with long-term consequences [16]. Despite the evidence, few studies tested the indirect effect of child maltreatment on the association between maternal depression and offspring maladjustment via mediation analysis [13]. Moreover, most prior studies measured child maltreatment occurring in early childhood, and maltreatment at older ages was insufficiently investigated [17].
Another factor that needs further examination is whether the impacts of maternal depression on self-esteem and emotion regulation differ between boys and girls. Adolescence is an important period when sex differences in several domains of human development emerge and these differences can be accounted for by both biological processes and environmental influences [18]. Longitudinal studies suggest that girls demonstrate a greater ability to manage their emotions than boys, but this difference seems to decrease across development and disappear by late adolescence [4]. Regarding self-esteem, there is a small but robust difference, with boys reporting higher self-esteem than girls—a disparity that increases during childhood, peaks in adolescence, and decreases in adulthood [5]. In the presence of maternal depression, male offspring have been found to be more affected on cognitive outcomes and externalizing problems, whereas girls are more vulnerable to internalizing problems [10]. Potential differences (or similarities) in psychosocial development between boys and girls need to be investigated to advance understanding of mental health problems occurring during adolescence [18].
Although the extensive evidence of the negative impact of maternal depression on adolescent psychosocial outcomes, the majority of the studies used data from high-income countries, especially those examining the mechanisms underlying this association [13]. Longitudinal studies with high retention rates, multiple assessments, a large sample size, and an equal number of male and female individuals to detect sex differences are relatively limited in low- and middle-income countries [18]. Knowledge on adolescents’ health determinants in developing countries, where 90% of young people live, is crucial as risk factors, such as socioeconomic deprivations and exposure to violence, are more severe and frequent in these settings [13].
Therefore, using a Brazilian population-based birth cohort study, we aimed: (1) to examine the impacts of maternal depressive symptoms trajectories from 3 months to 11 years on the adolescent’s emotion regulation and self-esteem at age 15 years (total effects); (2) to explore the mediating role of child maltreatment at age 11 years in relation to this association; and (3) to test whether adolescent sex moderates either the total, direct or indirect pathways of the proposed association.
Methods
Participants
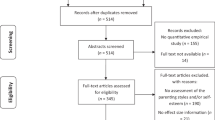
The 2004 Pelotas birth cohort is a population-based longitudinal study, occurring in the city of Pelotas, Brazil. The cohort recruited 4231 live newborns (99.2% of the births in 2004; 51.9% boys). Mothers were interviewed within 24 h postpartum using a standardized questionnaire. Mothers and their children were assessed again at home at mean (standard deviation) ages of 3.0 (0.1), 11.9 (0.2), 23.9 (0.4) and 49.5 (1.7) months and at a research clinic at 6.8 (0.3), and 11.0 (0.3) years (follow-up rates: 86.6% to 99.2%). The seventh follow-up, at a mean age of 15.7 (0.2), occurred between November 2019 and March 2020, when the social distancing measures due to COVID-19 pandemic took place in Brazil and data collection had to be interrupted. The total interviewed participants in the seventh follow-up included 46.1% of the original cohort (N = 1949). Further details about the cohort and data collection were published elsewhere [19, 20].
Measures
Maternal depressive symptoms trajectories
The Edinburgh Postnatal Depression Scale (EPDS) is a self-report scale assessing the intensity of depressive symptoms over the previous seven days, with higher scores indicating more severe depressive symptoms [21].
The EPDS scores from the 3-month to the 11-year-old follow-up were used to construct the trajectories of maternal depressive symptoms through a semi-parametric group-based modeling approach, a specialized form of finite mixture modeling [22, 23]. The steps and methods used to identify the trajectories of maternal depressive symptoms were detailed in previous studies [24, 25].
A five-group model emerged as the best fitting and most parsimonious model: (1) “low” and (2) “moderate-low” trajectories, which represented 74.5% of the sample and included women with EPDS < 10 across all time points. Group 3 “increasing” (11.1%), represented the women who had low levels of depressive symptoms in the children first years of life followed by a consistent increase in EPDS scores during the study period. The fourth group, “decreasing” (9.3%), was composed of women that showed high EPDS scores in the first 2 years postpartum and a decreasing tendency in those scores afterward. The fifth group, the “chronic-high” trajectory, comprised 5.2% of the sample and included mothers with high EPDS scores across the 11 years of children’s life.
Adolescents’ self-esteem and emotion regulation at age 15 years
Self-esteem was measured by the self-report Rosenberg Self-esteem Scale [26]. The measure includes 10 items scored on a 4-point Likert scale that evaluates individual's global self-esteem, including six items referring to a positive self-evaluation and four items related to a self-deprecating view (Table S1). The self-deprecating items were reverse-scored and a total score range from 10 to 40 was obtained by summing all items, with higher scores indicating higher levels of self-esteem.
Emotion regulation was assessed by the self-report version of the Emotional Regulation Index for Children and Adolescents (ERICA) [27]. ERICA is a 16-item scale rated on a 5-point Likert response format (scores range: 16–80). Ten items were reverse-scored, such that higher scores reflect more adaptive emotion regulation (Table S2). The measure is divided into three subscales: (i) Emotional control (7 items), which evaluates a social inappropriate emotional response; (ii) Emotional self-awareness (5 items), related to the recognition of self-emotions, and (iii) Situational responsiveness (4 items), regarding social empathy.
Child maltreatment at age 11 years
Child maltreatment was measured using the parent-report version of the Parent–Child Conflict Tactics Scale (CTSPC) [28]. We used a 14-item CTSPC version consisting of two subscales: (i) psychological aggression (5 items) and (ii) physical aggression (9 items), encompassing items related to physical punishment (6 items) and physical maltreatment (3 items). Each item was rated on a 5-point Likert scale. The CTSPC score was derived by summing all the responses (score range: 0–28) and higher scores indicate more frequent episodes of maltreatment. The CTSPC was completed mostly by biological or adoptive mothers (94.57%), followed by grandmothers (2.24%), biological fathers (2.04%), and other legal caregivers (1.45%).
Covariates
The covariates were collected in the perinatal interview and include: monthly family income in the month prior to delivery, maternal education (number of completed years of formal education), maternal self-reported skin color (white or non-white), marital status (mothers were asked if they were living with a partner; yes/no), and child sex.
Statistical analysis
Comparison of participants’ characteristics included and not included in the present study was analyzed using Pearson’s chi-square test. The not included sample was divided into (a) participants lost to follow-up before the sixth wave at age 11 years (N = 589) and (b) participants who were present at the sixth wave at age 11 years, but absent at the seventh wave at age 15 years due to follow-up interruption (N = 1693). We aimed to evaluate if the socioeconomic differences between the included and not included participants were mainly the result of the follow-up interruption occurred at the seventh wave. The mean score and standard deviation of the outcomes according to maternal and adolescents’ characteristics were analyzed using ANOVA. Descriptive statistics were conducted using Stata version 14.2.
As maternal depressive symptoms trajectories are a multi-categorical exposure, we used an indicator coding system to represent the different groups [29, 30]. Dummy variables were created for each category of the exposure, in which cases are set to 1 in that category, and 0 otherwise. The group that was not explicitly coded is treated as the reference category in the analysis (low trajectory of maternal depressive symptoms), and the parameters related to group differences are quantifications relative to this reference group [30].
In our conceptual model (Fig. 1A), the effect of each trajectory of maternal depressive symptoms in relation to the reference group on adolescents’ outcomes is the total effect (path c). The total effect comprises the direct effect (path c´) of each maternal depression trajectory on adolescents’ outcome and the indirect effect through child maltreatment (path a*b). Firstly, multivariable linear regression models were conducted to examine if the maternal depressive symptoms trajectories would predict the adolescents’ self-esteem and emotion regulation scores in two separated models for each outcome (total effects). The moderation by adolescents’ sex in the total effect pathway was verified by the inclusion of interaction terms in the linear regression models and probed by a Wald test for the comparison between the models with and without the interaction term. Next, we used structural equation modeling (SEM) to examine the mediating role of child maltreatment in the relationship between maternal depression trajectories and adolescent self-esteem and emotion regulation via a path model. The moderating role of adolescents’ sex in the indirect pathway (moderated mediation) was tested if the mediating effect was significant, calculated by a 95% bias-corrected confidence interval based on 5000 bootstrap samples that did not include the zero [29]. The adolescents’ sex was tested as the moderator of the direct pathway (path c´), first stage (the pathway from exposure to the mediator; path a), second stage (the pathway from mediator to the outcome; path b), and first + second stages of indirect pathways (path a*b; Fig. S1). Evidence for moderated mediation was tested by the computation of the Index of Moderated Mediation (IMM) and its 95% bias-corrected confidence interval based on 5000 bootstrap samples that did not contain zero [29]. All models were controlled for the covariates. The linear regression and path analyses were conducted using Mplus version 8.0, with maximum likelihood estimator and bootstrapped standard errors. Unstandardized (difference in outcomes’ means) and standardized (outcomes’ differences in standard deviations units) coefficients were reported. The effect sizes of the indirect pathways are represented by the structural equation modeling standardized coefficients and their 95% bias-corrected bootstrap confidence intervals (partially standardized effect) [29, 31], and can be interpreted as the outcomes’ expected change in standard deviations that the groups (“low” trajectory in contrast to the comparison trajectory) differ in average as a result of the indirect mechanism [29, 31]. All statistical tests were two-tailed, and significance was determined at the 0.05 level.
A Conceptual model of the mediating effect of child maltreatment on the association between maternal depressive symptoms trajectories on adolescents’ emotion regulation and self-esteem. B Statistical model for the relative mediating effects of child maltreatment on the association between maternal depressive symptoms trajectories adolescents’ emotion regulation (reference group: low trajectory); *p < 0.001; **p < 0.05; SE = Bias-corrected bootstrap standard Errors; B = unstandardized coefficients
Results
Attrition analysis
Compared to the participants lost to follow-up before the sixth wave, adolescents included in the analysis presented more advantaged socioeconomic indicators. The comparison between responders at the sixth wave who were not interviewed at the seventh follow-up, and the included participants shows that these groups did not differ according to the covariates (Table S3). It indicates that there were no major differences in socioeconomic variables between the samples who participated in the 15-year follow-up from those cohort members who were more likely to respond if the pandemics had not occurred. In addition, there were no differences in maternal depression and child maltreatment scores between those included and not included in the present study, showing that selection bias may not be a concern when interpreting the findings (Table S3).
Description of the sample characteristics
Lower adolescents’ self-esteem and emotion regulation scores were associated with lower family income and lower levels of maternal schooling. Adolescents from mothers in the high chronic depression trajectory had the lowest self-esteem and emotion regulation levels than any other group. Lower emotion regulation scores were also found in adolescents of single mothers, and who reported a non-white skin color. Self-esteem and emotion regulation scores were both lower for girls than boys (Table S4).
The means, standard deviations and correlations for all included study variables are presented in the Table S5. In addition, associations of the exposure with the mediator, and of the mediator with the outcomes, adjusted for confounders, are presented in Table S6. Emotion regulation score was negatively correlated to child maltreatment (CTSPC score; r = − 0.07, p < 0.001). In contrast, self-esteem score was unrelated to the CTSPC scores (r = − 0.02, p = 0.284). Adolescents’ sex was significantly associated with child maltreatment (r = 0.11, p < 0.001).
Results for adolescents’ self-esteem
Mean self-esteem score was 0.988 points lower among adolescents whose mothers belong to the high chronic depressive symptoms trajectory when compared to those from mothers in the low depressive symptoms trajectory group (unstandardized coefficient of the total effects; Table 1). We hypothesized that child maltreatment would mediate the effects of maternal depressive symptoms trajectories on the adolescents’ self-esteem. However, no evidence of indirect effects was found, based on the 95% bias-corrected bootstrap confidence intervals that included zero for all categories of maternal depression relative to the reference category.
We tested the moderating effect of adolescents’ sex by the inclusion of an interaction term in the linear regression model. The Wald test for comparison of the models with and without the interaction term was not significant (p = 0.207). It indicates that the impacts of maternal depression trajectories on adolescents’ self-esteem do not vary according to adolescents’ sex.
Results for adolescents’ emotion regulation
Mean emotion regulation score was 2.278 points lower among adolescents whose mothers belong to the high chronic depressive symptoms trajectory when compared to those from mothers in the low depressive symptoms trajectory group (unstandardized coefficients of total effects; Table 2).
Figure 1B and Table 2 present the results of the mediation analysis of child maltreatment on the association of maternal depressive symptoms trajectories and adolescents’ emotion regulation. Relative to the low trajectory group, all other trajectories of maternal depressive symptoms predicted higher levels of child maltreatment (Paths a1 to a4, Fig. 1B). Child maltreatment had a negative association with adolescent emotion regulation (Path b: B = − 0.118, SE = 0.059, p < 0.05) (Fig. 1B). All other trajectories of maternal depression had a negative direct effect on offspring emotion regulation, compared to the reference group (Table 2). All the indirect effects of maternal depression trajectories on adolescent emotion regulation through child maltreatment were negative and significant, indicated by the 95% bias-corrected bootstrap CI that did not include zero, supporting the hypothesis of a mediated-effect through child maltreatment. Adolescent from mothers belonging to the moderate low, increasing, decreasing and chronic-high trajectories scored, respectively, 0.016 (95% CI − 0.035; − 0.001), 0.026 (95% CI − 0.058; − 0.003), 0.019 (95% CI − 0.045; − 0.003), and 0.046 (95% CI − 0.101; − 0.006) standard deviations lower on emotion regulation scale than the reference group (adolescents from mothers in the “low” trajectory) as the result of the indirect mechanism via child maltreatment.
Figures S2–S4 and Table S7 show the statistical models for the moderated mediation analysis. No evidence of moderation by adolescents’ sex in the direct pathway was found (Fig. S2). Additionally, there was no evidence for a moderation of the indirect pathway, inferred by the 95% bias-corrected bootstrap CI for all IMM that included zero (Figs. S3 and S4; Table S7). The findings indicated that the total, direct and indirect effects of maternal depression trajectories on adolescents’ emotion regulation are linearly independent of adolescents’ sex.
Discussion
Using data from a Brazilian birth cohort, the current study examined the impact of maternal depressive symptoms trajectories on 15-year-old adolescents’ self-esteem and emotion regulation and child maltreatment at age 11 years as a potential mechanism underlying this association. The results showed that adolescents whose mothers had severe and chronic depressive symptoms reported lower levels of self-esteem and emotion regulation when compared to adolescents whose mothers had persistently low symptomatology. The negative effects of maternal depression on adolescent emotion regulation were partially mediated by child maltreatment at age 11 years. We found no evidence that the associations between maternal depressive symptoms and adolescent outcomes differ according to the adolescents’ sex.
Previous studies also identified harsh disciplinary strategies as an important mechanism by which maternal depression disrupts children’s normative development of emotional regulation [8, 32, 33]. The development of emotion regulation during childhood and adolescence is strongly influenced by the caregiver’s attention to the child’s emotional states and support in regulating emotional responses in accordance with situational demands [32]. When experiencing a negative emotion, children actively use the regulatory strategies learned through the interaction with their parents to manage distress [32]. Maternal depression is a well-known factor that negatively impacts the child-parent relationship and depressed mothers are likely to provide maladaptive models of emotional expressions to their offspring [8, 32]. Additionally, depressed mothers are more prone to use inconsistent parenting and disciplinary practices when dealing with child misbehavior, varying from permissive or unresponsive responses to a harsh strategy [15, 33]. Maternal depression was reported as a major risk factor for the occurrence of physical aggression, psychological and emotional abuse, and neglect [34, 35]. Children who have been maltreated are at increased risk of further maltreatment and maternal depression was identified as an important predictor of all types of maltreatment recurrence [36]. The intergenerational transmission of internalizing symptoms was partially explained by the depressed mothers’ greater use of harsh parenting strategies, especially psychological aggression [37, 38]. Furthermore, child maltreatment was found to mediate the association between maternal depression and a disruptive mother–child attachment relationship [39]. Contradictory parenting behaviors may lead to child’s lack of emotional security, which is associated with insecure attachment and disrupted emotional regulation development [8, 32]. Moreover, during early adolescence, parents and their offspring can experience less closeness and more conflictual relationship as teenagers strive for autonomy and less parental control [2]. Increasing conflicts and disagreement within the family may exacerbate maternal distress and lead a depressed mother to adopt harsh parenting strategies, including physical and psychological aggression [2, 15, 33].
The present study is also consistent with the literature reporting a negative association between maternal depression and adolescent self-esteem [14]. Prior research shows that depressed mothers are more likely to present hostile attitudes, be withdrawn and unresponsive, express negative feelings and criticism toward their children [12]. Child sense of self-worth is shaped by early social interactions, especially with parents; therefore, it is expected that children from depressed mother would present lower levels of self-esteem. This may be explained by scarce or predominantly negative maternal feedback related to the self-appraisal that is needed for the child identity formation [14]. Indeed, evidence from longitudinal studies suggests that the quality of both the home environment and the child–parent relationship during early childhood has long-lasting effects on individuals’ self-esteem, with a small but persisting effect until young adulthood [14]. Contrary to our initial theoretical-driven hypothesis, we found no evidence for a mediating role of child maltreatment for self-esteem. In fact, CTSPC scores were unrelated to adolescent self-esteem scores. A prior study showed that children’s self-conception may be related to several other aspects of maternal–child relationship quality regardless of maltreatment experiences [40]. In other words, the pathways linking maternal depression and adolescent self-esteem may include an absent sense of emotional security and psychological closeness in the mother–child relationship independent of the deleterious impacts of maltreatment [40]. As adolescence is a transitional period with significant changes in social environment, it is also possible that peers’ judgment about personal characteristics may have a heightened effect on self-esteem rather than the parental factors, thus buffering or exacerbating the negative effects of maternal depression [1, 2]. Future studies should consider assessing the quality of peer relationship and social support to develop a broader perspective of the relevant factors that affect adolescent self-esteem.
Contrary to our hypothesis, the associations between maternal depression and offspring emotion regulation and self-esteem are not moderated by adolescent sex. Previous evidence indicated that, in face of maternal depression, girls are at a higher risk of developing internalizing symptoms while boys are more susceptible to externalizing symptoms [10]. Accordingly, we expected that female adolescents whose mothers had been depressed would be more affected in terms of self-esteem and less affected in terms of emotion regulation, compared to male adolescents. Despite the absence of a moderating effect by sex, our results support the extensive evidence showing that girls present lower levels of self-esteem than boys [5]. Remarkably, we also found that girls also reported lower levels of emotion regulation, contrary to previous research indicating that boys show more emotion dysregulation, especially during adolescence [3]. Sex differences in emotional expressions and behaviors are determined by biological and sociocultural influences that occur during the individual’s life [18, 40]. The great social changes occurring during adolescence accentuate these environmental influences and shape the different patterns of behavior between boys and girls [18, 41]. Moreover, adolescence is a critical period when sex differences related to some mental health problems emerge, particularly in clinical depression, which present a female versus male prevalence ratio disparity of 2:1 [18]. Positive psychological assets, which include high self-esteem and adaptive levels of emotion regulation, are linked to resilience processes that contribute to thriving in the presence of adversities such as maternal depression [42]. Our results show that girls are particularly vulnerable to affective disorders when exposed to maternal depression due to lower levels of protective factors that could buffer the deleterious effects of stressors [7]. The malleable nature of such psychological assets (self-esteem and emotion regulation), rather than being fixed traits, represents an opportune target of intervention for the promotion of mental well-being of at-risk adolescents [43].
The current findings extend the prior research on maternal depression and offspring psychosocial development by examining a mechanism underlying this association in a Brazilian population-based birth cohort study. The prospective design and sample size of our study ensure temporal order between exposure, mediator and outcome measurements, increasing the confidence on the inference of specific causal pathways while testing for sex differences. Maternal depression was also evaluated through developmental trajectories, which describe the different patterns and progression of symptoms over time, identifying the adolescents’ most vulnerable groups according to the longitudinal exposure to maternal depressive symptoms. Additionally, child maltreatment was assessed at early adolescence, in contrast to most of previous evidence that measured it during childhood [17]. Finally, as both emotion regulation and self-esteem are subjective constructs based on self-evaluation, the outcomes’ assessment based on adolescent reports were essential.
There are some limitations to note about the present study. Unfortunately, the seventh wave had to be interrupted due to the COVID-19 pandemic, resulting in a loss to follow-up of nearly 50% from the original cohort. Although the attrition observed in the present study can be seen as the result of a random event, we cannot rule out that our analyses were, to some extent, subject to bias. However, it has been reported that loss to follow-up due to social disadvantages are related to modest differences in prevalence estimate [44]. In addition, Osler and colleagues [45] found that loss to follow-up did not bias the association between early life factors and adult mental health. Nonetheless, as we carefully adjusted all analyses for the main confounding variables, we believe that attrition mainly impacts the precision of estimates rather than the direction of association (i.e., the negative effects of maternal depression on adolescent outcomes). Indeed, the attrition analysis showed that the loss to follow-up due to socioeconomic disadvantages was more likely to occur before the sixth wave. Moreover, child maltreatment was based only on parent report, which could be affected by social desirability bias. Child reports could be not only more accurate on the prevalence of maltreatment, but also be more informative regarding how children perceive and experience the abuses committed by their parents [46]. Furthermore, our results should be considered in light of the assumptions of the mediation analysis (i.e., no unmeasured confounding between exposure–outcome, exposure–mediator and mediator–outcome associations). Despite the strengths of our study, it is important to note the limitations of observational studies in assessing causality as several parents and children share many potential genetical and environmental confounding influences that may further explain our associations [47, 48]. In addition, some relevant variables associated with the exposure, the mediator and the outcomes were not available for the current study, which constitutes a further limitation. Examples of such variables include maternal history of childhood maltreatment, child maltreatment at earlier ages, antenatal depression, and infant–mother attachment [38, 49, 50]. Finally, emotion regulation and self-esteem are complex constructs determined by genetic, social, cultural and individual factors and their interaction during the lifespan [4, 5]. It should be pointed out that our results presented relatively small effect sizes, suggesting that adolescents’ self-esteem and emotion regulation are likely to be further explained by several factors not addressed by our study. Nevertheless, our findings have important implications on intervention strategies targeting children and adolescents of depressed mothers.
The findings from the current study show that maternal depressive symptoms during childhood negatively impacts on self-esteem and emotion regulation at age 15 years, especially for children whose mothers experienced severe and chronic depressive symptoms. The current study adds to the literature by showing that the child maltreatment at age 11 years is a pathway through which maternal depression is linked to adolescent emotion regulation problems. Interventions targeting the prevention of child maltreatment and the promotion of positive disciplinary tactics may represent a possible route to reduce the impacts of maternal depression on adolescent adjustment.
References
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC (2018) The age of adolescence. Lancet Child Adolesc Health 2:223–228
Blakemore SJ (2019) Adolescence and mental health. Lancet 393:2030–2031
Compas BE, Jaser SS, Bettis AH, Watson KH et al (2017) Coping, emotion regulation, and psychopathology in childhood and adolescence: a meta-analysis and narrative review. Psychol Bull 143:939–991
Buss KA, Pérez-Edgar K, Vallorani A, Anaya B (2019) Emotion reactivity and regulation: a developmental model of links between temperament and personality. In: McAdamas DP, Shiner RL, Tackett JL (eds) Handbook of personality development. The Guilford Press, New York, pp 106–117
Orth U, Robins RW (2019) Development of Self-Esteem across the Lifespan. In: McAdamas DP, Shiner RL, Tackett JL (eds) Handbook of personality development. The Guilford Press, New York, pp 328–344
Masselink M, Van Roekel E, Oldehinkel AJ (2017) Self-esteem in early adolescence as predictor of depressive symptoms in late adolescence and early adulthood: the mediating role of motivational and social factors. J Youth Adolesc 47:932–946
Fiorelli C, Grimaldi CT, Barni D, Buonomo I, Gentile S (2019) Predicting adolescent depression: the interrelated roles of self-esteem and interpersonal stressors. Front Psychol. https://doi.org/10.3389/fpsyg.2019.00565
Bariola E, Gullone E, Hughes EK (2011) Child and adolescent emotion regulation: the role of parental emotion regulation and expression. Clin Child Fam Psychol Rev 14:198–212
World Health Organization (WHO) (2020) Guidelines on mental health promotive and preventive interventions for adolescents: helping adolescents thrive. World Health Organization, Geneva
Sanger C, Iles JE, Andew CS, Ramchandani PG (2015) Association between postnatal maternal depression and psychological outcomes in adolescent offspring: a systematic review. Arch Womens Ment Health 18:147–162
Gelaye B, Rondon MB, Araya R, Williams MA (2016) Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 3:973–982
Goodman SH (2007) Depression in mothers. Ann Rev Clin Psychol 3:107–135
Herba CM, Glover V, Ramchandani PG, Rondon MB (2016) Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiatry 3:983–992
Orth U (2018) The family environment in early childhood has a long-term effect on self-esteem: a longitudinal study from birth to age 27 years. J Pers Soc Psychol 114:637–655
Choi KW, Houts R, Arseneault L, Pariante C et al (2018) Maternal depression in the intergenerational transmission of childhood maltreatment and its sequelae: testing postpartum effects in a longitudinal birth cohort. Dev Psychopathol 31:143–156
Bellis MA, Hughes K, Ford K, Ramos Rodriguez G et al (2019) Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public health 4:e517–e528. https://doi.org/10.1016/S2468-2667(19)30145-8
Thornberry TP, Matsuda M, Greenman SJ, Augustyn MB et al (2014) Adolescent risk factors for child maltreatment. Child Abuse Negl 38:706–722
Zahn-Waxler C, Crick NR, Shirtcliff EA, Woods KE (2015) The origins and development of psychopathology in females and males. In: Cicchetti D, Cohen DJ (eds) Developmental psychopathology: theory and method. John Wiley & Sons, Inc, Hoboekn, pp 76–138
Santos IS, Barros AJ, Matijasevich A, Domingues MR et al (2011) Cohort profile: the 2004 Pelotas (Brazil) birth cohort study. Int J Epidemiol 40:1461–1468
Santos IS, Barros AJ, Matijasevich A, Zanini R et al (2014) Cohort profile update: 2004 Pelotas (Brazil) Birth Cohort Study. body composition, mental health and genetic assessment at the 6 years follow-up. Int J Epidemiol 43:1437–1437
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry 150:782–786
Nagin D, Tremblay RE (1999) Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Dev 70:1181–1196
Nagin DS (2005) Group-based modeling of development. Harvard University Press, Boston
Azeredo CM, Santos IS, Barros AJD, Barros FC et al (2017) Maternal depression and bullying victimization among adolescents: Results from the 2004 Pelotas cohort study. Depress Anxiety 34:897–907
Matijasevich A, Murray J, Cooper PJ, Anselmi L et al (2015) Trajectories of maternal depression and offspring psychopathology at 6 years: 2004 Pelotas cohort study. J Affect Disord 174:424–431
Rosenberg M (1989) Society and the adolescent self-image. Wesleyan University Press, Middletown.
MacDermott ST, Gullone E, Allen JS, King NJ et al (2010) The Emotion regulation index for children and adolescents (ERICA): a psychometric investigation. J Psychopathol Behavioral Assess 32:301–314
Straus MA, Hamby SL, Finkelhor D, Moore DW et al (1998) Identification of child maltreatment with the parent-child conflict tactics scales: development and psychometric data for a national sample of American parents. Child Abuse Negl 22:1177–1177
Hayes AF, Little TD (2018) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. The Guilford Press, New York
Hayes AF, Preacher KJ (2014) Statistical mediation analysis with a multicategorical independent variable. Br J Math Stat 67:451–470
Preacher KJ, Kelley K (2011) Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods 16:93–115
Blandon AY, Calkins SD, Keane SP, O’Brien M (2008) Individual differences in trajectories of emotion regulation processes: the effects of maternal depressive symptomatology and children’s physiological regulation. Dev Psychol 44:1110–1123
Wolford SN, Cooper AN, McWey LM (2019) Maternal depression, maltreatment history, and child outcomes: the role of harsh parenting. Am J Orthopsychiatry 89:181–191
Conron KJ, Beardslee W, Koenen KC, Buka SL et al (2009) A longitudinal study of maternal depression and child maltreatment in a national sample of families investigated by child protective services. Arch Pediatr Adolesc Med 163:922–930
Stith SM, Liu T, Davies LC, Boykin EL et al (2009) Risk factors in child maltreatment: a meta-analytic review of the literature. Aggress Violent Behav 14:13–29
White OG, Hindley N, Jones DP (2014) Risk factors for child maltreatment recurrence: an updated systematic review. Med Sci Law 55:259–277
Kuckertz JM, Mitchell C, Wiggins JL (2017) Parenting mediates the impact of maternal depression on child internalizing symptoms. Depress Anxiety 35:89–97
Plant DT, Pariante CM, Sharp D, Pawlby S (2015) Maternal depression during pregnancy and offspring depression in adulthood: role of child maltreatment. Br J Psych 207:213–220
Martoccio TL, Brophy-Herb HE, Maupin AN, Robinson JL (2015) Longitudinal pathways from early maternal depression to children’s dysregulated representations: a moderated mediation analysis of harsh parenting and gender. Attach Hum Dev 18:46–68
Kim J, Cicchetti D (2004) A longitudinal study of child maltreatment, mother-child relationship quality and maladjustment: the role of self-esteem and social competence. J Abnorm Child Psychol 32:341–354
Chaplin TM, Aldao A (2013) Gender differences in emotion expression in children: a meta-analytic review. Psychol Bull 139:735–765
Gartland D, Riggs E, Muyeen S, Giallo R et al (2019) What factors are associated with resilient outcomes in children exposed to social adversity? A systematic review. BMJ Open 9:e024870. https://doi.org/10.1136/bmjopen-2018-024870
Barry MM, Clarke AM, Jenkins R, Patel V (2013) A systematic review of the effectiveness of mental health promotion interventions for young people in low- and middle-income countries. BMC Public Health 13:835. https://doi.org/10.1186/1471-2458-13-835
Piedvache A, van Buuren S, Barros H, Ribeiro AI, Draper E, Zeitlin J (2021) Strategies for assessing the impact of loss to follow-up on estimates of neurodevelopmental impairment in a very preterm cohort at 2 years of age. BMC Med Res Methodol 21:118. https://doi.org/10.1186/s12874-021-01264-3
Osler M, Kriegbaum M, Christensen U, Lund R, Nybo Andersen AM (2008) Loss to follow up did not bias associations between early life factors and adult depression. J clin epidemiol 61:958–963
Lev-Wiesel R, Massrawa N, Binson B (2019) Parents’ and children’s perceptions of child maltreatment. J Soc Work 20:395–410
McAdams TA, Rijsdijk FV, Narusyte J, Ganiban JM et al (2017) Associations between the parent-child relationship and adolescent self-worth: a genetically informed study of twin parents and their adolescent children. J Child Psychol Psychiatry 58:46–54
McGue M, Osler M, Christensen K (2010) Causal inference and observational research: the utility of twins. Perspect Psychol Sci 5:546–556
Savage LE, Tarabulsy GM, Pearson J, Collin-Vézina D, Gagné LM (2019) Maternal history of childhood maltreatment and later parenting behavior: a meta-analysis. Dev psychopathol 31:9–21
Ogbo FA, Eastwood J, Hendry A, Jalaludin B, Agho KE, Barnett B, Page A (2018) Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry 18:49. https://doi.org/10.1186/s12888-018-1598-x
Acknowledgements
The authors would like to thank the participating families and staff who collaborated in the various stages of the 2004 Pelotas Birth Cohort study. This work was supported by the Brazilian Association of Public Health (ABRASCO); the Children's Pastorate; the World Health Organization [Grant no. 03014HNI]; the National Support Program for Centers of Excellence (PRONEX) [Grant no. 04/0882.7]; the Brazilian National Research Council (CNPq) [Grant no. 481012-2009-5; 484077-2010-4; 470965-2010-0; 481141-2007-3; 426024/2016-8]; the Brazilian Ministry of Health [Grant no. 25000.105293/2004-83]; the São Paulo Research Foundation (FAPESP) [Grant no. 2014/13864-6; 2020/07730-8]. JMM is supported by FAPESP [Grant no. 2017/22723-5]. LTR, ISS, AJDB, JM and AM are supported by CNPq Research Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All 2004 Pelotas Birth Cohort follow-ups were approved by the Federal University of Pelotas Medical School Research Ethics Committee. Principal caregivers of the participants signed an informed consent form. At ages 11 and 15 years, adolescents signed an informed assent form. The present study was also approved by the Research Committee of the University of São Paulo (Research Protocol no. 402/18).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Maruyama, J.M., Valente, J.Y., Tovo-Rodrigues, L. et al. Maternal depression trajectories in childhood, subsequent maltreatment, and adolescent emotion regulation and self-esteem: the 2004 Pelotas birth cohort. Eur Child Adolesc Psychiatry 32, 1935–1945 (2023). https://doi.org/10.1007/s00787-022-02022-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-022-02022-6