Abstract
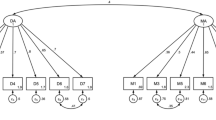
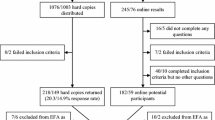
Despite evidence for its efficacy and effectiveness, the use of medication for the treatment of ADHD remains controversial. Little is known about the factors that influence clinicians’ decisions to use medication for ADHD. Here, we present initial data on the attitudes of prescribing clinicians from the Influences on Prescribing for ADHD Questionnaire (IPAQ)—a new clinician-completed, 40-item scale. The eight IPAQ subscales cover attitudes towards (1) treatment outcome optimisation, (2) the use of rule based over more informal approaches, (3) side effects, (4) symptoms control as the primary goal of treatment, (5) the influence of external pressure on medication-related decisions, (6) the value of taking the child’s views into account, (7) long-term medication use and (8) the value of psychosocial approaches for the treatment of ADHD. Sixty-eight clinicians from Belgium and the UK took part. All subscales had acceptable levels of internal reliability (Chronbach’s alpha = 0.62–0.78). Overall, clinicians reported taking a rule-based approach to prescribing with a focus on treatment optimisation, taking the child’s view into account and valuing psycho-social approaches. They focused on treating broader patterns of impairment, but were wary of the potential side effects and long-term treatment. Psychiatrists scored high on their focus on symptom control and preference for long-term medication use, while paediatricians reported using more rule-based approaches. We identified four distinctive response profiles: (1) pro-psychosocial; (2) medication focused; (3) unsystematic; and (4) response optimizers. Future larger scale studies are required to replicate these profiles and to explore their relationship with prescribing behaviour and treatment outcomes.

Similar content being viewed by others
References
Barkley RA et al (2004) Young adult follow-up of hyperactive children: antisocial activities and drug use. J Child Psychol Psychiatry 45(2):195–211
Jensen PS et al (2001) ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry 40(2):147–158
Kadesjo B, Gillberg C (2001) The comorbidity of ADHD in the general population of Swedish school age children. J Child Psychol Psychiatry 42:487–492
Thompson MJ et al (2004) Profiles, co-morbidity and their relationship to treatment of 191 children with AD/HD and their families. Eur Child Adolesc Psychiatry 13(4):234–242
Barkley RA, Fischer M, Smallish L, Fletcher K (2006) Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry 45(2):192–202
Barkley RA (2002) International consensus statement on ADHD. January 2002. Clin Child Fam Psychol Rev 5(2):89–111
Chitsabesan P et al (2006) Mental health needs of young offenders in custody and in the community. Br J Psychiatry 188:534–540
Gadow KD et al (2002) Tics and psychiatric comorbidity in children and adolescents. Dev Med Child Neurol 44(5):330–338
Johnston C, Mash EJ (2001) Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clin Child Fam Psychol Rev 4(3):183–207
Swensen AR et al (2003) Attention-deficit/hyperactivity disorder: increased costs for patients and their families. J Am Acad Child Adolesc Psychiatry 42(12):1415–1423
Pelham WE, Foster EM, Robb JA (2007) The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. J Pediatr Psychol 32(6):711–727
Excellence, N.I.f.C., Health NCCfM. Attention deficit hyperactivity disorder. Diagnosis and management of ADHD in children, young people, and adults (full NICE guideline) (2008)
Network SIG (2009) Management of attention deficit and hyperkinetic disorders in children and young people. SIGN, Edinburgh
Taylor E et al (2004) European clinical guidelines for hyperkinetic disorder—first upgrade. Eur Child Adolesc Psychiatry 13(Suppl 1):I7–I30
Subcommittee on Attention-Deficit/Hyperactivity Disorder, S.C.O.Q.I. and Management, ADHD: Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics (2011)
Pliszka S (2007) Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 46(7):894–921
Santosh PJ, Taylor E (2000) Stimulant drugs. Eur Child Adolesc Psychiatry 9(Suppl 1):I27–I43
Greenhill LL, Findling RL, Swanson JM (2002) A double-blind, placebo-controlled study of modified-release methylphenidate in children with attention-deficit/hyperactivity disorder. Pediatrics 109(3):E39
Greenhill L et al (2006) Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD. J Am Acad Child Adolesc Psychiatry 45(11):1284–1293
Biederman J et al (2009) Do stimulants protect against psychiatric disorders in youth with ADHD? A 10-year follow-up study. Pediatrics 124(1):71–78
Jensen DM et al (1999) Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: the Multimodal Treatment Study of children with Attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56(12):1088–1096
Michelson D et al (2001) Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose–response study. Pediatrics 108(5):E83–E83
Donnelly C et al (2009) Safety and tolerability of atomoxetine over 3 to 4 years in children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry 48(2):176–185
Jain R et al (2011) Clonidine extended-release tablets for pediatric patients with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 50(2):171–179
Greenhill LL et al (2001) Impairment and deportment responses to different methylphenidate doses in children with ADHD: the MTA titration trial. J Am Acad Child Adolesc Psychiatry 40(2):180–187
Banaschewski T et al (2006) Long-acting medications for the hyperkinetic disorders. A systematic review and European treatment guideline. Eur Child Adolesc Psychiatry 15(8):476–495
Kovshoff H et al (2012) The decisions regarding ADHD management (DRAMa) study: uncertainties and complexities in assessment, diagnosis and treatment, from the clinician’s point of view. Eur Child Adolesc Psychiatry 21(2):87–99
Banaschewski T et al (2008) Long-acting medications for the treatment of hyperkinetic disorders—a systematic review and European treatment guidelines. Part 2: a quantitative evaluation of long-acting medications. Z Kinder Jugendpsychiatr Psychother 36(2):97–106 (quiz 106-7)
Schachar R et al (2002) Attention-deficit hyperactivity disorder: critical apparaisal of extended treatment studies. Can J Psychiatry 47:337–348
Vitiello B (2001) Long-term effects of stimulant medications on the brain: possible relevance treatment of attention deficit hyperactivity disorder. J Child Psychol Psychiatry 11:25–34
Andersen SL (2005) Stimulants and the developing brain. Trends Pharmacol Sci 26:237–243
Grund T et al (2006) Influence of methylphenidate on brain development—an update of recent animal experiments. Behav Brain Funct 2:2
Pappadopulos E et al (2009) Medication adherence in the MTA: saliva methylphenidate samples versus parent report and mediating effect of concomitant behavioral treatment. J Am Acad Child Adolesc Psychiatry 48(5):501–510
Charach A et al (2008) A theoretical approach to medication adherence for children and youth with psychiatric disorders. Harv Rev Psychiatry 16(2):126–135
Coghill DR, Rhodes SM, Matthews K (2007) The neuropsychological effects of chronic methylphenidate on drug-naive boys with attention-deficit/hyperactivity disorder. Biol Psychiatry 62(9):954–962
Barbaresi WJ et al (2007) Modifiers of long-term school outcomes for children with attention-deficit/hyperactivity disorder: does treatment with stimulant medication make a difference? Results from a population-based study. J Dev Behav Pediatr 28(4):274–287
Powers RL et al (2008) Stimulant treatment in children with attention-deficit/hyperactivity disorder moderates adolescent academic outcome. J Child Adolesc Psychopharmacol 18(5):449–459
Scheffler RM et al (2009) Positive association between attention-deficit/hyperactivity disorder medication use and academic achievement during elementary school. Pediatrics 123(5):1273–1279
Krause J (2008) SPECT and PET of the dopamine transporter in attention-deficit/hyperactivity disorder. Expert Rev Neurother 8(4):611–625
Volkow ND et al (2009) Effects of modafinil on dopamine and dopamine transporters in the male human brain: clinical implications. JAMA 301(11):1148–1154
Acknowledgments
This work was supported by funding from Shire Development LLC.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kovshoff, H., Vrijens, M., Thompson, M. et al. What influences clinicians’ decisions about ADHD medication? Initial data from the Influences on Prescribing for ADHD Questionnaire (IPAQ). Eur Child Adolesc Psychiatry 22, 533–542 (2013). https://doi.org/10.1007/s00787-013-0393-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-013-0393-y