Abstract
Objectives
The benefits of professional dental treatment for oral diseases have been widely investigated. However, it is unclear whether professional dental treatment provides additional benefits for improving general health.
Materials and methods
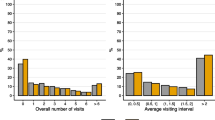
Data were obtained from the US National Health and Nutrition Examination Survey (NHANES) 1999 to 2004 and 2011 to 2018 cycles. A total of 36,174 participants were included and followed-up for mortality until December 31, 2019. Dental visit behavior was defined as the time interval of last dental visit (TIDV, < 0.5 year, 0.5–1 year, 1–2 years, 2–5 years, and > 5 years) and the main reasons of the last dental visit (treatment, examination, and other reasons). The Cox proportional risk model was used to estimate the hazard ratio (HR) and 95% confidence interval (CI).
Results
Compared with participants with time interval of less than 0.5 year, the multivariate-adjusted HRs and 95%CI for participants with time interval of more than 5 years were 1.45 (1.31, 1.61) for all-cause mortality (P trend < 0.0001), 1.49 (1.23, 1.80) for cardiovascular diseases mortality (P trend = 0.0009) and 1.53 (1.29, 1.81) for cancer mortality (P trend = 0.013). Compared with dental visit for examination, participants who had their dental visit for treatment had higher risk for mortality. For participants with dental visit for examination, TIDV of less than 1 year showed lower risk for mortality, whereas TIDV of less than 0.5 year is recommend for population with dental visit for treatment.
Conclusions
Poor dental visit behavior is associated with an increased risk of mortality. Further well-designed studies are needed to confirm the association between professional dental visit and mortality.
Clinical relevance
This study highlights the potential benefits of regular dental visits in maintaining general health.



Similar content being viewed by others
References
Bernabe E, Marcenes W, Hernandez CR et al (2020) Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res 99(4):362–373
Marcenes W, Kassebaum NJ, Bernabé E et al (2013) Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res 92(7):592–597
Loe H, Theilade E, Jensen SB (1965) Experimental gingivitis in man. J Periodontol 36:177–187
Sanz M, Beighton D, Curtis MA et al (2017) Role of microbial biofilms in the maintenance of oral health and in the development of dental caries and periodontal diseases: consensus report of group 1 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal disease. J Clin Periodontol 44(Suppl 18):S5–S11
Kleinstein SE, Nelson KE, Freire M (2020) Inflammatory networks linking oral microbiome with systemic health and disease. J Dent Res 99(10):1131–1139. https://doi.org/10.1177/0022034520926126
Sanz M, Marco Del Castillo A et al (2020) Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol 47(3):268–288. https://doi.org/10.5334/gh.400
Xu K, Yu W, Li Y et al (2022) Association between tooth loss and hypertension: a systematic review and meta-analysis. J Dent 123:104178. https://doi.org/10.1016/j.jdent.2022.104178
Maisonneuve P, Amar S, Lowenfels AB (2017) Periodontal disease, edentulism, and pancreatic cancer: a meta-analysis. Ann Oncol 28(5):985–995. https://doi.org/10.1093/annonc/mdx019
Romandini M, Baima G, Antonoglou G et al (2021) Periodontitis, edentulism, and risk of mortality: a systematic review with meta-analyses. J Dent Res 100(1):37–49. https://doi.org/10.1177/0022034520952401
Weijden van der F, Slot DE (2011) Oral hygiene in the prevention of periodontal diseases: the evidence. Periodontol 2000 55:1:104–123. https://doi.org/10.1111/j.1600-0757.2009.00337.x
Newton JT, Asimakopoulou K (2015) Managing oral hygiene as a risk factor for periodontal disease: a systematic review of psychological approaches to behavior change for improved plaque control in periodontal management. J Clin Periodontol Suppl 16:S36–S46. https://doi.org/10.1111/jcpe.12356
Hujoel PP, Hujoel MLA, Kotsakis GA (2018) Personal oral hygiene and dental caries: a systematic review of randomised controlled trials. Gerodontology 35(4):282–289. https://doi.org/10.1111/ger.12331
Gholami M, Pakdaman A, Virtanen JI (2012) Common perceptions of periodontal health and illness among adults: a qualitative study. ISRN Dent 2012:671879. https://doi.org/10.5402/2012/671879
Park SY, Kim SH, Kang SH et al (2019) Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: a population-based study from Korea. Eur Heart J 40(14):1138–1145. https://doi.org/10.1093/eurheartj/ehy836
Tonetti MS, D’Aiuto F, Nibali L et al (2007) Treatment of periodontitis and endothelial function. N Engl J Med 356(9):911–920. https://doi.org/10.1056/NEJMoa063186
Taylor HL, Rahurkar S, Treat TJ et al (2021) Does Nonsurgical Periodontal Treatment Improve Systemic Health? J Dent Res 100(3):253–260. https://doi.org/10.1177/0022034520965958
D’Aiuto F, Parkar M, Andreou G et al (2004) Periodontitis and systemic inflammation: control of the local infection is associated with a reduction in serum inflammatory markers. J Dent Res 83(2):156–160. https://doi.org/10.1177/154405910408300214
Di Mario S, Spettoli D, Alessandrini C et al (2011) Periodontal infection and preterm birth: successful periodontal therapy reduces the risk of preterm birth. BJOG 118(5):635–636. https://doi.org/10.1111/j.1471-0528.2011.02913.x
D’Aiuto F, Gkranias N, Bhowruth D et al (2018) Systemic effects of periodontitis treatment in patients with type 2 diabetes: a 12 month, single-centre, investigator-masked, randomised trial. Lancet Diabetes Endocrinol 6(12):954–965. https://doi.org/10.1016/S2213-8587(18)30038-X
Bellissimo-Rodrigues WT, Menegueti MG, Gaspar GG et al (2014) Effectiveness of a dental care intervention in the prevention of lower respiratory tract nosocomial infections among intensive care patients: a randomized clinical trial. Infect Control Hosp Epidemiol 35(11):1342–1348. https://doi.org/10.1086/678427
Zhou X, Han J, Liu Z et al (2014) Effects of periodontal treatment on lung function and exacerbation frequency in patients with chronic obstructive pulmonary disease and chronic periodontitis: a 2-year pilot randomized controlled trial. J Clin Periodontol 41(6):564–572. https://doi.org/10.1111/jcpe.12247
Liu J, Zong X, Vogtmann E et al (2022) Tooth count, untreated caries and mortality in US adults: a population-based cohort study. Int J Epidemiol 51(4):1291–1303. https://doi.org/10.1093/ije/dyac072
Gupta A, Felton DA, Jemt T, Koka S (2019) Rehabilitation of edentulism and mortality: a systematic review. J Prosthodont 28(5):526–535. https://doi.org/10.1111/jopr.12792
Sabbah W, Slade GD, Sanders AE, Bernabé E (2020) Denture wearing and mortality risk in edentulous American adults: a propensity score analysis. J Dent 100:103360. https://doi.org/10.1016/j.jdent.2020.103360
Dai J, Li A, Liu Y et al (2022) Denture wearing status, cardiovascular health profiles, and mortality in edentulous patients: a prospective study with a 27-year follow-up. J Dent 126:104287. https://doi.org/10.1016/j.jdent.2022.104287
Engebretson SP, Hyman LG, Michalowicz BS et al (2013) The effect of nonsurgical periodontal therapy on hemoglobin A1c levels in persons with type 2 diabetes and chronic periodontitis: a randomized clinical trial. JAMA 310(23):2523–2532. https://doi.org/10.1001/jama.2013.282431
Janket SJ, Wightman A, Baird AE et al (2005) Does periodontal treatment improve glycemic control in diabetic patients? A meta-analysis of intervention studies. J Dent Res 84(12):1154–1159. https://doi.org/10.1177/154405910508401212
Centers for Disease Control and Prevention. 2019 Public-Use Linked Mortality Files. https://www.cdc.gov/nchs/data-linkage/mortality-public.htm. Acaccessed 9 Sept 2022
Zhao H, Pan Y, Wang C et al (2021) The effects of metal exposures on charlson comorbidity index using zero-inflated negative binomial regression model: NHANES 2011–2016. Biol Trace Elem Res 199(6):2104–2111. https://doi.org/10.1007/s12011-020-02331-4
Martinez-Herrera M, López-Domènech S, Silvestre FJ et al (2018) Dietary therapy and non-surgical periodontal treatment in obese patients with chronic periodontitis. J Clin Periodontol 45:1448–1457. https://doi.org/10.1111/jcpe.13030
Erciyas K, Sezer U, Ustun K et al (2013) Effects of periodontal therapy on disease activity and systemic inflammation in rheumatoid arthritis patients. Oral Dis 19:394–400. https://doi.org/10.1111/odi.12017
Teeuw WJ, Slot DE, Susanto H et al (2014) Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J Clin Periodontol 41:70–79. https://doi.org/10.1111/jcpe.12171
Lee K, Lee JS, Kim J et al (2020) Oral health and gastrointestinal cancer: a nationwide cohort study. J Clin Periodontol 47:796–808. https://doi.org/10.1111/jcpe.13304
Nishide A, Fujita M, Sato Y, Nagashima K, Takahashi S, Hata A (2017) Income-related inequalities in access to dental care services in Japan. Int J Environ Res Public Health 14(5):524. https://doi.org/10.3390/ijerph14050524
Simon L, Choi SE, Ticku S, Fox K, Barrow J, Palmer N (2020) Association of income inequality with orthodontic treatment use. J Am Dent Assoc 151(3):190–196. https://doi.org/10.1016/j.adaj.2019.11.021
Green CA, Gender PCR (1999) Psychosocial factors and the use of medical services: a longitudinal analysis. Soc Sci Med 48(10):1363–1372. https://doi.org/10.1016/s0277-9536(98)00440-7
Wamala S, Merlo J, Boström G (2006) Inequity in access to dental care services explains current socioeconomic disparities in oral health: the Swedish National Surveys of Public Health 2004–2005. J Epidemiol Community Health 60(12):1027–1033. https://doi.org/10.1136/jech.2006.046896
Locker D, Maggirias J, Quiñonez C (2011) Income, dental insurance coverage, and financial barriers to dental care among Canadian adults. J Public Health Dent 71(4):327–334. https://doi.org/10.1111/j.1752-7325.2011.00277.x
Christian B, Chattopadhyay A, Kingman A, Boroumand S, Adams A, Garcia I (2013) Oral health care services utilisation in the adult US population: medical expenditure panel survey 2006. Community Dent Health 30(3):161–167
Bisquera A, Turner EB, Ledwaba-Chapman L, Dunbar-Rees R, Hafezparast N, Gulliford M et al (2021) Inequalities in developing multimorbidity over time: a population-based cohort study from an urban, multi-ethnic borough in the United Kingdom. Lancet Reg Health Eur 12:100247. https://doi.org/10.1016/j.lanepe.2021.100247
Martin LJ, Chen Y, Serrano-Lomelin J, Talbot J, Yasui Y (2020) Higher levels of social and material deprivation are associated with higher rates of influenza-like illness-related emergency department visits: Edmonton, Alberta, 2004–2014. Public Health 189:117–122. https://doi.org/10.1016/j.puhe.2020.06.039
Wu Y, Qi D (2020) Material deprivation, parenting practices, and children’s psychological health and wellbeing in China. J Community Psychol 48(8):2644–2662. https://doi.org/10.1002/jcop.22441
Bui FQ, Almeida-da-Silva CLC, Huynh B et al (2019) Association between periodontal pathogens and systemic disease. Biomed J 42:27–35. https://doi.org/10.1111/jcpe.13304
Kitamoto S, Nagao-Kitamoto H, Hein R et al (2020) The bacterial connection between the oral cavity and the gut diseases. J Dent Res 99:1021–1029. https://doi.org/10.1177/0022034520924633
van der Meulen TA, Harmsen H, Bootsma H et al (2016) The microbiome-systemic diseases connection. Oral Dis 22:719–734. https://doi.org/10.1111/odi.12472
Acknowledgements
The authors acknowledge the financial support from grant number 2019KB01 from the State Key Laboratory of Military Stomatology, China, grant LCA202004 and LCB202209 from National Clinical Research Centre for Oral Diseases, and grant 2020TD-033 from the Shaanxi Key Scientific and Technological Innovation Team and by the Youth Innovation Team of Shaanxi Universities.
Funding
Financial support from grant number 2019KB01 from the State Key Laboratory of Military Stomatology, China, grant LCA202004 from National Clinical Research Centre for Oral Diseases, grant LCB202209 from National Clinical Research Centre for Oral Diseases and grant 2020TD-033 from the Shaanxi Key Scientific and Technological Innovation Team and by the Youth Innovation Team of Shaanxi Universities.
Author information
Authors and Affiliations
Contributions
Contributions are as follows: design, L.N.N., K.H.X., S.M., S.L.J.; analysis: K.H.X., J.T.G., Q.L.; methodology: L.N.N., K.H.X; project administration: L.N.N., T.Z., F.T.; resources: K.H.X., S.M., Y.Y.L.; software: S.L.J., Z.H.J., Q.L.; supervision: L.N.N., T.Z., F.T.; writing (original draft): K.H.X., S.M. All authors participated in the decision to submit.
Corresponding authors
Ethics declarations
Ethical approval
The NHANES data is publicly available data from the National Center for Health Statistics, and thus, the work was deemed to be exempt.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, K., Ma, S., Gu, J. et al. Association between dental visit behavior and mortality: a nationwide longitudinal cohort study from NHANES. Clin Oral Invest 28, 37 (2024). https://doi.org/10.1007/s00784-023-05471-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05471-8