Abstract
Objectives
Sleep bruxism (SB) is associated with physiological activities including sympathetic autonomic system dominance and sleep micro-arousal. While oral appliances (OA) are used to prevent SB harmful effects, the influence of OAs physiological mechanisms during sleep is unknown. The aim of this study is to assess whether heart rate variability (HRV) changes, as a marker of autonomic nervous system activity, would be associated with the OA mechanism of action on SB using occlusal splint (OS) and mandibular advancement splint (MAS).
Materials and methods
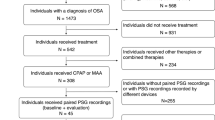
A retrospective analysis, from data previously collected in 21 participants with SB (25.6 ± 4.5 years) with polysomnographic recordings, was done. HRV data were compared between a reference night (no-device) and ones during which OS or MAS was used in a crossover study design. Rhythmic masticatory muscle activity (RMMA) index was compared between nights. HRV was evaluated using autoregressive model analysis for three sections: baseline (distance from RMMA), immediately before, and after RMMA period.
Results
A significant reduction in RMMA index, when wearing OA during sleep, was observed (P < 0.01), but was not associated with HRV parameters change. HRV significantly changed after RMMA onset for nights with OA during non-REM sleep in comparison with baseline (P < 0.02).
Conclusions
The usage of OAs for SB participants reduced RMMA, but most likely independently of changes in HRV linked to the mechanism associated with SB genesis.
Clinical relevance
Wearing OA seems to reduce grinding noise and protect from dental injuries but does not seem to influence SB genesis.

Similar content being viewed by others
References
Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, de Leeuw R, Manfredini D, Svensson P, Winocur E (2013) Bruxism defined and graded: an international consensus. J Oral Rehabil 40:2–4. https://doi.org/10.1111/joor.12011
Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, Santiago V, Winocur E, De Laat A, De Leeuw R, Koyano K, Lavigne GJ, Svensson P, Manfredini D (2018) International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. https://doi.org/10.1111/joor.12663
Medicine AAoS (2014) International classification of sleep disorders–third edition (ICSD-3). American Academy of Sleep Medicine, Westchester, NY
Raphael KG, Santiago V, Lobbezoo F (2016) Is bruxism a disorder or a behaviour? Rethinking the international consensus on defining and grading of bruxism. J Oral Rehabil 43:791–798. https://doi.org/10.1111/joor.12413
Mayer P, Heinzer R, Lavigne G (2016) Sleep bruxism in respiratory medicine practice. Chest 149:262–271. https://doi.org/10.1378/chest.15-0822
van Selms MK, Visscher CM, Knibbe W, Thymi M, Lobbezoo F (2020) The association between self-reported awake oral behaviors and orofacial pain depends on the belief of patients that these behaviors are harmful to the jaw. J Oral Facial Pain Headache 34:273–280. https://doi.org/10.11607/ofph.2629
Lavigne G, Kato T, Herrero Babiloni A, Huynh N, Dal Fabbro C, Svensson P, Aarab G, Ahlberg J, Baba K, Carra MC, Cunha TCA, Gonçalves DAG, Manfredini D, Stuginski-Barbosa J, Wieckiewicz M and Lobbezoo F (2021) Research routes on improved sleep bruxism metrics: toward a standardised approach. J Sleep Res:e13320. https://doi.org/10.1111/jsr.13320
Harada T, Ichiki R, Tsukiyama Y, Koyano K (2006) The effect of oral splint devices on sleep bruxism: a 6-week observation with an ambulatory electromyographic recording device. J Oral Rehabil 33:482–488. https://doi.org/10.1111/j.1365-2842.2005.01576.x
Nikolopoulou M, Ahlberg J, Visscher CM, Hamburger HL, Naeije M, Lobbezoo F (2013) Effects of occlusal stabilization splints on obstructive sleep apnea: a randomized controlled trial. J Orofac Pain 27:199–205. https://doi.org/10.11607/jop.967
Carra MC, Huynh NT, El-Khatib H, Remise C, Lavigne GJ (2013) Sleep bruxism, snoring, and headaches in adolescents: short-term effects of a mandibular advancement appliance. Sleep Med 14:656–661. https://doi.org/10.1016/j.sleep.2013.03.009
Franco L, Rompré PH, de Grandmont P, Abe S, Lavigne GJ (2011) A mandibular advancement appliance reduces pain and rhythmic masticatory muscle activity in patients with morning headache. J Orofac Pain 25:240–249
Landry ML, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ (2006) Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont 19:549–556
Landry-Schonbeck A, de Grandmont P, Rompré PH, Lavigne GJ (2009) Effect of an adjustable mandibular advancement appliance on sleep bruxism: a crossover sleep laboratory study. Int J Prosthodont 22:251–259
Mainieri VC, Saueressig AC, Fagondes SC, Teixeira ER, Rehm DD, Grossi ML (2014) Analysis of the effects of a mandibular advancement device on sleep bruxism using polysomnography, the BiteStrip, the sleep assessment questionnaire, and occlusal force. Int J Prosthodont 27:119–126. https://doi.org/10.11607/ijp.3675
Solanki N, Singh BP, Chand P, Siddharth R, Arya D, Kumar L, Tripathi S, Jivanani H, Dubey A (2017) Effect of mandibular advancement device on sleep bruxism score and sleep quality. J Prosthet Dent 117:67–72. https://doi.org/10.1016/j.prosdent.2016.04.009
Kato T, Montplaisir JY, Guitard F, Sessle BJ, Lund JP, Lavigne GJ (2003) Evidence that experimentally induced sleep bruxism is a consequence of transient arousal. J Dent Res 82:284–288. https://doi.org/10.1177/154405910308200408
Lavigne GJ, Huynh N, Kato T, Okura K, Adachi K, Yao D, Sessle B (2007) Genesis of sleep bruxism: motor and autonomic-cardiac interactions. Arch Oral Biol 52:381–384. https://doi.org/10.1016/j.archoralbio.2006.11.017
Carra MC, Huynh N, Morton P, Rompré PH, Papadakis A, Remise C, Lavigne GJ (2011) Prevalence and risk factors of sleep bruxism and wake-time tooth clenching in a 7- to 17-yr-old population. Eur J Oral Sci 119:386–394. https://doi.org/10.1111/j.1600-0722.2011.00846.x
Kato T, Rompré P, Montplaisir JY, Sessle BJ, Lavigne GJ (2001) Sleep bruxism: an oromotor activity secondary to micro-arousal. J Dent Res 80:1940–1944. https://doi.org/10.1177/00220345010800101501
Huynh N, Kato T, Rompré PH, Okura K, Saber M, Lanfranchi PA, Montplaisir JY, Lavigne GJ (2006) Sleep bruxism is associated to micro-arousals and an increase in cardiac sympathetic activity. J Sleep Res 15:339–346. https://doi.org/10.1111/j.1365-2869.2006.00536.x
Inano S, Mizumori T, Kobayashi Y, Sumiya M, Yatani H (2013) Identification of sleep bruxism with an ambulatory wireless recording system. Int J Prosthodont 26:527–535. https://doi.org/10.11607/ijp.3331
Kostka PS, Tkacz EJ (2015) Multi-sources data analysis with sympatho-vagal balance estimation toward early bruxism episodes detection. Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Annual Conference 2015:6010–6013. https://doi.org/10.1109/embc.2015.7319761
Huynh N, Lavigne GJ, Lanfranchi PA, Montplaisir JY, de Champlain J (2006) The effect of 2 sympatholytic medications–propranolol and clonidine–on sleep bruxism: experimental randomized controlled studies. Sleep 29:307–316. https://doi.org/10.1093/sleep/29.3.307
Sakai T, Kato T, Yoshizawa S, Suganuma T, Takaba M, Ono Y, Yoshizawa A, Yoshida Y, Kurihara T, Ishii M, Kawana F, Kiuchi Y, Baba K (2017) Effect of clonazepam and clonidine on primary sleep bruxism: a double-blind, crossover, placebo-controlled trial. J Sleep Res 26:73–83. https://doi.org/10.1111/jsr.12442
Vanderveken OM, Devolder A, Marklund M, Boudewyns AN, Braem MJ, Okkerse W, Verbraecken JA, Franklin KA, De Backer WA, Van de Heyning PH (2008) Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med 178:197–202. https://doi.org/10.1164/rccm.200701-114OC
Rechtschaffen A and Kales A (1968) A manual of standardized terminology, techniques and scoring techniques for sleep stages of human subjects. Brain Research Institute, Los Angeles
Bonnet M, Carley D, Carskadon M, Easton P, Guilleminault C, Harper RM, Hayes B, Hirshkowitz M, Ktonas P, Keenan S (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
TRoaAAoSMT Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Lavigne GJ, Guitard F, Rompré PH, Montplaisir JY (2001) Variability in sleep bruxism activity over time. J Sleep Res 10:237–244. https://doi.org/10.1046/j.1365-2869.2001.00261.x
Lavigne GJ, Rompré PH, Montplaisir JY (1996) Sleep bruxism: validity of clinical research diagnostic criteria in a controlled polysomnographic study. J Dent Res 75:546–552. https://doi.org/10.1177/00220345960750010601
Lavigne GJ, Rompré PH, Poirier G, Huard H, Kato T, Montplaisir JY (2001) Rhythmic masticatory muscle activity during sleep in humans. J Dent Res 80:443–448. https://doi.org/10.1177/00220345010800020801
Rompré PH, Daigle-Landry D, Guitard F, Montplaisir JY, Lavigne GJ (2007) Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res 86:837–842. https://doi.org/10.1177/154405910708600906
Electrophysiology TFotESoCatNASoPa (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17:354–81
Lanfranchi PA, Fradette L, Gagnon JF, Colombo R, Montplaisir J (2007) Cardiac autonomic regulation during sleep in idiopathic REM sleep behavior disorder. Sleep 30:1019–1025. https://doi.org/10.1093/sleep/30.8.1019
Lavigne GJ, Okura K, Abe S, Colombo R, Huynh N, Montplaisir JY, Marchand S, Lanfranchi PA (2011) Gender specificity of the slow wave sleep lost in chronic widespread musculoskeletal pain. Sleep Med 12:179–185. https://doi.org/10.1016/j.sleep.2010.07.015
Burr RL (2007) Interpretation of normalized spectral heart rate variability indices in sleep research: a critical review. Sleep 30:913–919. https://doi.org/10.1093/sleep/30.7.913
Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K (2008) Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil 35:476–494. https://doi.org/10.1111/j.1365-2842.2008.01881.x
Dube C, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ (2004) Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res 83:398–403. https://doi.org/10.1177/154405910408300509
Huynh NT, Rompré PH, Montplaisir JY, Manzini C, Okura K, Lavigne GJ (2006) Comparison of various treatments for sleep bruxism using determinants of number needed to treat and effect size. Int J Prosthodont 19:435–441
Saueressig AC, Mainieri VC, Grossi PK, Fagondes SC, Shinkai RS, Lima EM, Teixeira ER, Grossi ML (2010) Analysis of the influence of a mandibular advancement device on sleep and sleep bruxism scores by means of the BiteStrip and the Sleep Assessment Questionnaire. Int J Prosthodont 23:204–213
Singh PK, Alvi HA, Singh BP, Singh RD, Kant S, Jurel S, Singh K, Arya D, Dubey A (2015) Evaluation of various treatment modalities in sleep bruxism. J Prosthet Dent 114:426–431. https://doi.org/10.1016/j.prosdent.2015.02.025
Abekura H, Yokomura M, Sadamori S, Hamada T (2008) The initial effects of occlusal splint vertical thickness on the nocturnal EMG activities of masticatory muscles in subjects with a bruxism habit. Int J Prosthodont 21:116–120
Arima T, Tomonaga A, Toyota M, Inoue SI, Ohata N, Svensson P (2012) Does restriction of mandibular movements during sleep influence jaw-muscle activity? J Oral Rehabil 39:545–551. https://doi.org/10.1111/j.1365-2842.2012.02310.x
Avivi-Arber L, Martin R, Lee JC, Sessle BJ (2011) Face sensorimotor cortex and its neuroplasticity related to orofacial sensorimotor functions. Arch Oral Biol 56:1440–1465. https://doi.org/10.1016/j.archoralbio.2011.04.005
Dao TT, Lavigne GJ (1998) Oral splints: the crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med 9:345–361. https://doi.org/10.1177/10454411980090030701
Ikuta M, Iida T, Kothari M, Shimada A, Komiyama O, Svensson P (2019) Impact of sleep bruxism on training-induced cortical plasticity. J Prosthodont Res 63:277–282. https://doi.org/10.1016/j.jpor.2018.12.008
Matsumoto H, Tsukiyama Y, Kuwatsuru R, Koyano K (2015) The effect of intermittent use of occlusal splint devices on sleep bruxism: a 4-week observation with a portable electromyographic recording device. J Oral Rehabil 42:251–258. https://doi.org/10.1111/joor.12251
Clark GT, Beemsterboer PL, Solberg WK, Rugh JD (1979) Nocturnal electromyographic evaluation of myofascial pain dysfunction in patients undergoing occlusal splint therapy. J Am Dent Assoc 99:607–611. https://doi.org/10.14219/jada.archive.1979.0348
Van der Zaag J, Lobbezoo F, Wicks DJ, Visscher CM, Hamburger HL, Naeije M (2005) Controlled assessment of the efficacy of occlusal stabilization splints on sleep bruxism. J Orofac Pain 19:151–158
Macaluso GM, Guerra P, Di Giovanni G, Boselli M, Parrino L, Terzano MG (1998) Sleep bruxism is a disorder related to periodic arousals during sleep. J Dent Res 77:565–573. https://doi.org/10.1177/00220345980770040901
Badilini F, Maison-Blanche P, Coumel P (1998) Heart rate variability in passive tilt test: comparative evaluation of autoregressive and FFT spectral analyses. Pacing Clin Electrophysiol 21:1122–1132. https://doi.org/10.1111/j.1540-8159.1998.tb00159.x
Fagard RH, Pardaens K, Staessen JA, Thijs L (1998) Power spectral analysis of heart rate variability by autoregressive modelling and fast Fourier transform: a comparative study. Acta Cardiol 53:211–218
Li K, Rudiger H, Ziemssen T (2019) Spectral analysis of heart rate variability: time window matters. Front Neurol 10:545. https://doi.org/10.3389/fneur.2019.00545
Acknowledgements
The authors would like to thank Keigo Miyata and Yusuke Kameoka in Chest Co. for their support of RemLogic software in the study. This paper was based on data from sleep studies supported by the Canadian Institutes of Health Research (CIHR) and the Fonds de la Recherche en Santé du Québec (FRSQ) grants to G. Lavigne who holds a Canada Research Chair in Pain, Sleep and Trauma. Susumu Abe was a visiting scholar from Tokushima University Graduate School, Tokushima, Japan, during his stay in Montreal, Canada. Recognition to Margaret Mckyes and Joshua Wolfe for English editing.
Funding
This paper was based on data from sleep studies supported by the Canadian Institutes of Health Research (CIHR) and the Fonds de la Recherche en Santé du Québec (FRSQ) grants to G. Lavigne who holds a Canada Research Chair in Pain, Sleep and Trauma.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Pierre de Grandmont is deceased.
Rights and permissions
About this article
Cite this article
Abe, S., Huynh, N.T., Kato, T. et al. Oral appliances reduce masticatory muscle activity-sleep bruxism metrics independently of changes in heart rate variability. Clin Oral Invest 26, 5653–5662 (2022). https://doi.org/10.1007/s00784-022-04520-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04520-y