Abstract
Objectives
To assess the clinical and radiographic outcomes of implants treated by means of non-surgical debridement with systemic antibiotic therapy.
Materials and methods
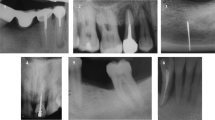
A prospective case series study evaluating the 12-month clinical and radiographic outcomes of peri-implantitis lesions treated with ultrasonic scaler debridement, a glycine air abrasive, and metronidazole followed by supportive maintenance. Clinical and radiographic variables and success criteria were defined a priori.
Results
Overall, 21 patients were included. One implant failed during the study period (implant survival rate 95.24%). Substantial changes occurred at 12 months in all the clinical and radiographic variables, reaching strong statistical significance in the majority of them. According to the success criteria applied, 40.90% of the peri-implantitis were arrested and resolved, while 59.1% presented with at least one probed site with bleeding on probing (BoP). Moreover, 95.45% exhibited peri-implant pocket depth (PPD) < 5 mm at the end of the study. None of the implants presented with progressive bone loss.
Conclusion
Non-surgical therapy of peri-implantitis is effective to arrest progressive bone loss, reduce PPD and suppuration, and achieve radiographic bone fill in the majority of cases. Nevertheless, it failed to be completely efficacious in the achievement of successful therapeutic outcomes as BoP remained frequently present.
Clinical relevance
Non-surgical therapy achieved significant clinical and radiological improvements.



Similar content being viewed by others
References
Derks J, Schaller D, Hakansson J, Wennstrom JL, Tomasi C, Berglundh T (2016) Peri-implantitis—onset and pattern of progression. J Clin Periodontol 43:383–388
Khoshkam V, Chan HL, Lin GH, MacEachern MP, Monje A, Suarez F, Giannobile WV, Wang HL (2013) Reconstructive procedures for treating peri-implantitis: a systematic review. J Dent Res 92:131S–138S
Chan HL, Lin GH, Suarez F, MacEachern M, Wang HL (2014) Surgical management of peri-implantitis: a systematic review and meta-analysis of treatment outcomes. J Periodontol 85:1027–1041
Mailoa J, Lin GH, Chan HL, MacEachern M, Wang HL (2014) Clinical outcomes of using lasers for peri-implantitis surface detoxification: a systematic review and meta-analysis. J Periodontol 85:1194–1202
Faggion CM Jr, Listl S, Fruhauf N, Chang HJ, Tu YK (2014) A systematic review and Bayesian network meta-analysis of randomized clinical trials on non-surgical treatments for peri-implantitis. J Clin Periodontol 41:1015–1025
Schou S, Berglundh T, Lang NP (2004) Surgical treatment of peri-implantitis. Int J Oral Maxillofac Implants 19(Suppl):140–149
Carcuac O, Derks J, Charalampakis G, Abrahamsson I, Wennstrom J, Berglundh T (2016) Adjunctive systemic and local antimicrobial therapy in the surgical treatment of peri-implantitis: a randomized controlled clinical trial. J Dent Res 95:50–57
Carcuac O, Derks J, Abrahamsson I, Wennstrom JL, Petzold M, Berglundh T (2017) Surgical treatment of peri-implantitis: 3-year results from a randomized controlled clinical trial. J Clin Periodontol 44:1294–1303
Berglundh T, Wennstrom JL, Lindhe J (2018) Long-term outcome of surgical treatment of peri-implantitis. A 2-11-year retrospective study. Clin Oral Implants Res 29:404–410
Heitz-Mayfield LJA, Salvi GE, Mombelli A, Faddy M, Lang NP (2012) Anti-infective surgical therapy of peri-implantitis. A 12-month prospective clinical study. Clin Oral Implants Res 23:205–210
Mettraux GR, Sculean A, Burgin WB, Salvi GE (2016) Two-year clinical outcomes following non-surgical mechanical therapy of peri-implantitis with adjunctive diode laser application. Clin Oral Implants Res 27:845–849
Teles RP, Haffajee AD, Socransky SS (2006) Microbiological goals of periodontal therapy. Periodontol 42:180–218
Roccuzzo M, Layton DM, Roccuzzo A, Heitz-Mayfield LJ (2018) Clinical outcomes of peri-implantitis treatment and supportive care: a systematic review. Clin Oral Implants Res 29(Suppl 16):331–350
Claffey N, Clarke E, Polyzois I, Renvert S (2008) Surgical treatment of peri-implantitis. J Clin Periodontol 35:316–332
Bassetti M, Schar D, Wicki B, Eick S, Ramseier CA, Arweiler NB, Sculean A, Salvi GE (2014) Anti-infective therapy of peri-implantitis with adjunctive local drug delivery or photodynamic therapy: 12-month outcomes of a randomized controlled clinical trial. Clin Oral Implants Res 25:279–287
Haffajee AD, Socransky SS, Gunsolley JC (2003) Systemic anti-infective periodontal therapy. A systematic review. Ann Periodontol 8:115–181
Stein JM, Hammacher C, Michael SS (2018) Combination of ultrasonic decontamination, soft tissue curettage, and submucosal air polishing with povidone-iodine application for non-surgical therapy of peri-implantitis: 12 month clinical outcomes. J Periodontol 89:139–147
Rodrigo D, Sanz-Sánchez I, Figuero E, Llodrá JC, Bravo M, Caffesse RG, Vallcorba N, Guerrero A, Herrera D (2018) Prevalence and risk indicators of peri-implant diseases in Spain. J Clin Periodontol 45(12):1510–1520
Monje A, Wang HL, Nart J (2017) Association of preventive maintenance therapy compliance and peri-implant diseases: a cross-sectional study. J Periodontol 88:1030–1041
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4(1):1–6
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43(1):38
Heitz-Mayfield LJA, Salvi GE, Mombelli A, Loup PJ, Heitz F, Kruger E, Lang NP (2018) Supportive peri-implant therapy following anti-infective surgical peri-implantitis treatment: 5-year survival and success. Clin Oral Implants Res 29(1):1–6
Koldsland OC, Wohlfahrt JC, Aass AM (2018) Surgical treatment of peri-implantitis: prognostic indicators of short-term results. J Clin Periodontol 45(1):100–113
La Monaca G, Pranno N, Annibali S, Cristalli MP, Polimeni A (2018) Clinical and radiographic outcomes of a surgical reconstructive approach in the treatment of peri-implantitis lesions: a 5-year prospective case series. Clin Oral Implants Res 29(10):1025–1037
Schwendicke F, Stolpe M, Graetz C (2017) Cost comparison of prediction-based decision-making for periodontally affected molars. J Clin Periodontol 44(11):1145–1152
Powell CA, Mealey BL, Deas DE, McDonnell HT, Moritz AJ (2005) Post-surgical infections: prevalence associated with various periodontal surgical procedures. J Periodontol 76(3):329–333
Hashim D, Cionca N, Combescure C, Mombelli A (2018) The diagnosis of peri-implantitis: a systematic review on the predictive value of bleeding on probing. Clin Oral Implants Res 29(Suppl 16):276–293
Roos-Jansåker AM, Almhojd US, Jansson H (2017) Treatment of peri-implantitis: clinical outcome of chloramine as an adjunctive to non-surgical therapy, a randomized clinical trial. Clin Oral Implants Res 28:43–48
Schwarz F, Becker K, Renvert S (2015) Efficacy of air polishing for the non-surgical treatment of peri-implant diseases: a systematic review. J Clin Periodontol 42:951–959
Loesche WJ (1992) The specific plaque hypothesis and the antimicrobial treatment of periodontal disease. Dent Update 19(68):70–2, 74
Lafaurie GI, Sabogal MA, Castillo DM, Rincón MV, Gómez LA, Lesmes YA, Chambrone L (2017) Microbiome and microbial biofilm profiles of Peri-Implantitis: a systematic review. J Periodontol 88:1066–1089
Listl S, Fruhauf N, Dannewitz B, Weis C, Tu YK, Chang HJ, Faggion CM Jr (2015) Cost-effectiveness of non-surgical peri-implantitis treatments. J Clin Periodontol 42:470–477
Fox SC, Moriarty JD, Kusy RP (1990) The effects of scaling titanium implant surface with a metal and plastic instruments: an in vitro study. J Periodontol 61:485–490
Steffensen B, Suzuki H, Caffesse RG, Ash MM (1987) Repair of periodontal angular bony defects evaluated by one- and two-dimensional radiographic analysis. Oral Surg Oral Med Oral Pathol 63:109–114
Steffensen B, Webert HP (1989) Relationship between the radiographic periodontal defect angle and healing after treatment. J Periodontol 60:248–254
Nibali L, Yeh YC, Pometti D, Tu YK (2018) Long-term stability of intrabony defects treated with minimally-invasive non-surgical therapy. J Clin Periodontol 45(12):1458–1464
Renvert S, Roos-Jansäker AM, Claffey N (2008) Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol 35(8 Suppl):305–315
Rams TE, Degener JE, van Winkelhoff AJ (2014) Antibiotic resistance in human peri-implantitis microbiota. Clin Oral Implants Res 225(1):82–90
Funding
The present investigation was a self-funded investigation by the Department of Periodontology of the Universitat Internacional de Catalunya.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This case series study was performed in accordance with the Universitat Internacional de Catalunya Ethical Committee (PERECL201802) and Helsinki Declaration.
Informed consent
All patients read and signed an appropriate informed consent document prior to participation in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nart, J., Pons, R., Valles, C. et al. Non-surgical therapeutic outcomes of peri-implantitis: 12-month results. Clin Oral Invest 24, 675–682 (2020). https://doi.org/10.1007/s00784-019-02943-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02943-8