Abstract
Introduction
Repair materials for extensive cervical root defects may come in direct contact with periodontal tissues. This in vitro study compared the effects of four calcium silicate cements (CSC), one resin-modified glass ionomer cement, and one glass carbomer cement on primary human gingival fibroblasts (HGF), alveolar osteoblasts (HAO), and a human osteoblast cell line (hFOB 1.19).
Methods
HGF, HAO, and hFOB were seeded on discoid test specimens. Relative numbers of viable cells were quantitatively assessed after 1 and 24 h for cytotoxicity/adhesion assays and after 4, 24, 48, and 72 h for proliferation assays. Data were statistically analyzed using non-parametric tests (α = 0.05).
Results
Relative to the control (100 %), CSC allowed for mean numbers of 71–81 % viable HGF and 80–82 % viable HAO. Then, 64 % of HGF and 56 % of HAO were assessed on GC Fuji II LC. Mean numbers of viable cells were 59–64 % HGF and 67–68 % HAO for GCP Glass Fill specimens. Cells exposed to CSC over 24 h remained viable and even increased in number. Both cell types adhered almost equally well to CSC and GC Fuji II LC. GCP Glass Fill continued to decrease cell viability and adhesion. CSC-based materials and GC Fuji II LC allowed for HGF and hFOB proliferation; however, none of the tested materials specifically stimulated cell proliferation.
Conclusions
CSC characterized by low cytotoxicity. GC Fuji II LC shows moderate cytotoxic effects. ProRoot MTA, Harvard MTA, Biodentine, EndoSequence putty, and GC Fuji II LC allow HGF and HAO to adhere and HGF and hFOB to proliferate. GCP Glass Fill decreases cell viability, adhesion, and proliferation.
Clinical relevance
CSC remain the paramount biologic choice for the repair of extensive cervical root defects. GC Fuji II LC might be considered in addition to CSC when the defect comprises supracrestal areas and the restoration requires superior aesthetic and mechanical characteristics.






Similar content being viewed by others
References
Patel S, Kanagasingam S, Pitt Ford TR (2009) External cervical resorption: a review. J Endod 35:616–625
Torabinejad M, Parirokh M (2010) Mineral trioxide aggregate: a comprehensive literature review—part II: leakage and biocompatibility investigations. J Endod 36:190–202
Katsamakis S, Slot DE, Van der Sluis LW, Van der Weijden F (2013) Histological responses of the periodontium to MTA: a systematic review. J Clin Periodontol 40:334–344
Prati C, Gandolfi MG (2015) Calcium silicate bioactive cements: biological perspectives and clinical applications. Dent Mater 31:351–370
Krupp C, Bargholz C, Brüsehaber M, Hülsmann M (2013) Treatment outcome after repair of root perforations with mineral trioxide aggregate: a retrospective evaluation of 90 teeth. J Endod 39:1364–1368
Pontius V, Pontius O, Braun A, Frankenberger R, Roggendorf MJ (2013) Retrospective evaluation of perforation repairs in 6 private practices. J Endod 39:1346–1358
Mente J, Leo M, Panagidis D, Saure D, Pfefferle T (2014) Treatment outcome of mineral trioxide aggregate: repair of root perforations-long-term results. J Endod 40:790–796
Yilmaz HG, Kalender A, Cengiz E (2010) Use of mineral trioxide aggregate in the treatment of invasive cervical resorption: a case report. J Endod 36:160–163
Fernández R, Rincón JG (2011) Surgical endodontic management of an invasive cervical resorption class 4 with mineral trioxide aggregate: a 6-year follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:e18–e22
Parirokh M, Torabinejad M (2010) Mineral trioxide aggregate: a comprehensive literature review—part III: clinical applications, drawbacks, and mechanism of action. J Endod 36:400–413
Keskin C, Demiryurek EO (2015) Ozyurek T (2015) Color stabilities of calcium silicate-based materials in contact with different irrigation solutions. J Endod 41:409–411
Kim SY, Yang SE (2011) Surgical repair of external inflammatory root resorption with resin-modified glass ionomer cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:e33–e36
Nicholson JW, Czarnecka B (2008) The biocompatibility of resin-modified glass-ionomer cements for dentistry. Dent Mater 24:1702–1718
GCP Dental (2014) GCP Glass Fill: Tips & Tricks Glass Fill. Retrieved from http://www.gcp-dental.com/wp-content/uploads/2014/08/Tips_and_Tricks_GCP_April_2014.pdf
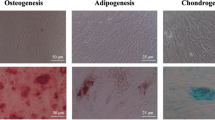
Diercke K, Sen S, Kohl A, Lux CJ, Erber R (2011) Compression-dependent up-regulation of ephrin-A2 in PDL fibroblasts attenuates osteogenesis. J Dent Res 90:1108–1115
Zingler S, Erber R, Lux CJ, Seeberger R, Bister D, Ludwig B (2013) Biocompatibility of gold and stainless steel chains used for forced eruption of impacted teeth—an in vitro investigation. Oral Surg Oral Med Oral Pathol Oral Radiol 116:159–168
Fuss Z, Trope M (1996) Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol 12:255–264
Martins TM, Bosco AF, Nóbrega FJ, Nagata MJ, Garcia VG, Fucini SE (2007) Periodontal tissue response to coverage of root cavities restored with resin materials: a histomorphometric study in dogs. J Periodontol 78:1075–1082
Zhou HM, Shen Y, Wang ZJ, Li L, Zheng YF, Häkkinen L, Haapasalo M (2013) In vitro cytotoxicity evaluation of a novel root repair material. J Endod 39:478–483
Al-Rabeah E, Perinpanayagam H, MacFarland D (2006) Human alveolar bone cells interact with ProRoot and tooth-colored MTA. J Endod 32:872–875
Schmalz G (1994) Use of cell cultures for toxicity testing of dental materials—advantages and limitations. J Dent 22:S6–S11
Ahmed HM, Luddin N, Kannan TP, Mokhtar KI, Ahmad A (2014) Cell attachment properties of Portland cement-based endodontic materials: biological and methodological considerations. J Endod 40:1517–1523
Buttke TM, McCubrey JA, Owen TC (1993) Use of an aqueous soluble tetrazolium/formazan assay to measure viability and proliferation of lymphokine-dependent cell lines. J Immunol Methods 157:233–240
Attik GN, Villat C, Hallay F, Pradelle-Plasse N, Bonnet H, Moreau K, Colon P, Grosgogeat B (2014) In vitro biocompatibility of a dentine substitute cement on human MG63 osteoblasts cells: Biodentine™ versus MTA®. Int Endod J 47:1133–1141
Camilleri J (2008) The biocompatibility of modified experimental Portland cements with potential for use in dentistry. Int Endod J 41:1107–1114
De Deus G, Ximenes R, Gurgel-Filho ED, Plotkowski MC, Coutinho-Filho T (2005) Cytotoxicity of MTA and Portland cement on human ECV 304 endothelial cells. Int Endod J 38:604–609
Camilleri J, Montesin FE, Di Silvio L, Pitt Ford TR (2005) The chemical constitution and biocompatibility of accelerated Portland cement for endodontic use. Int Endod J 38:834–842
Haglund R, He J, Jarvis J, Safavi KE, Spångberg LS, Zhu Q (2003) Effects of root-end filling materials on fibroblasts and macrophages in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95:739–745
Ma J, Shen Y, Stojicic S, Haapasalo M (2011) Biocompatibility of two novel root repair materials. J Endod 37:793–798
von Wilmowsky C, Vairaktaris E, Pohle D, Rechtenwald T, Lutz R, Munstedt H, Koller G, Schmidt M, Neukam FW, Schlegel KA, Nkenke E (2008) Effects of bioactive glass and beta-TCP containing three-dimensional laser sintered polyetheretherketone composites on osteoblasts in vitro. J Biomed Mater Res A 87:896–902
Willershausen I, Wolf T, Kasaj A, Weyer V, Willershausen B, Marroquin BB (2013) Influence of a bioceramic root end material and mineral trioxide aggregates on fibroblasts and osteoblasts. Arch Oral Biol 58:1232–1237
Samara A, Sarri Y, Stravopodis D, Tzanetakis GN, Kontakiotis EG, Anastasiadou E (2011) A comparative study of the effects of three root-end filling materials on proliferation and adherence of human periodontal ligament fibroblasts. J Endod 37:865–870
Montellano AM, Schwartz SA, Beeson TJ (2006) Contamination of tooth-colored mineral trioxide aggregate used as a root-end filling material: a bacterial leakage study. J Endod 32:452–455
Safar JA, Davis RD, Overton JD (1999) Effect of saliva contamination on the bond of dentin to resin-modified glass-ionomer cement. Oper Dent 24:351–357
Menne-Happ U, Ilie N (2013) Effect of gloss and heat on the mechanical behaviour of a glass carbomer cement. J Dent 41:223–230
Geurtsen W, Spahl W, Leyhausen G (1998) Residual monomer/additive release and variability in cytotoxicity of light-curing glass-ionomer cements and compomers. J Dent Res 77:2012–2019
Makkawy HA, Koka S, Lavin MT, Ewoldsen NO (1998) Cytotoxicity of root perforation repair materials. J Endod 24:477–479
Brackett MG, Bouillaguet S, Lockwood PE, Rotenberg S, Lewis JB, Messer RL, Wataha JC (2007) In vitro cytotoxicity of dental composites based on new and traditional polymerization chemistries. J Biomed Mater Res B Appl Biomater 81:397–402
Oliva A, Della Ragione F, Salerno A, Riccio V, Tartaro G, Cozzolino A, D’Amato S, Pontoni G, Zappia V (1996) Biocompatibility studies on glass ionomer cements by primary cultures of human osteoblasts. Biomaterials 17:1351–1356
Huang FM, Tai KW, Chou MY, Chang YC (2002) Resinous perforation-repair materials inhibit the growth, attachment, and proliferation of human gingival fibroblasts. J Endod 28:291–294
Schweikl H, Müller R, Englert C, Hiller KA, Kujat R, Nerlich M, Schmalz G (2007) Proliferation of osteoblasts and fibroblasts on model surfaces of varying roughness and surface chemistry. J Mater Sci Mater Med 18:1895–1905
Acknowledgments
The authors thank Mrs Tanja Krüger and Mrs Edith Daum for their invaluable expertise and support concerning the laboratory experiments. The linguistic support of Mrs Joanna Voerste and Mr Adam Gaier in preparing the manuscript is highly appreciated. The authors further thank Mrs Kirsten Stoik for assistance in preparation of the figures. The authors also thank the manufacturers for supplying the materials.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. All materials tested within this study project were provided by the manufacturers, but they did not fund this study. They had no influence on the study design, data collection and analysis, or on the decision to publish or in preparing the manuscript.
Funding
The study project was funded by the Department of Conservative Dentistry and the Department of Orthodontics of the Clinic for Oral, Dental, and Maxillofacial Diseases, University Hospital Heidelberg, Germany.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the University of Heidelberg (Ref. 80/94 and S147/2010) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study before the collection of alveolar bone cells (HAO) and/or primary human fibroblasts from the gingiva (HGF).
Rights and permissions
About this article
Cite this article
Michel, A., Erber, R., Frese, C. et al. In vitro evaluation of different dental materials used for the treatment of extensive cervical root defects using human periodontal cells. Clin Oral Invest 21, 753–761 (2017). https://doi.org/10.1007/s00784-016-1830-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1830-3