Abstract
Objectives
Increased collagenolytic activity in diabetes may compromise collagen membrane (CM) survival. Tetracycline (TTC) possesses anti-collagenolytic properties and delays CM degradation. This study evaluated macrophage and capillary infiltration within CMs in diabetic rats.
Materials and methods
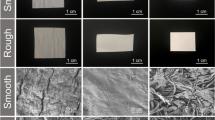
Diabetes was induced in 20 Wistar rats by streptozotocin and 20 served as controls. Biotin-labeled CM discs were immersed in either TTC (50 mg/ml) or PBS. In each animal, 2 discs (TTC and control) were implanted under the parietal periosteum and rats were sacrificed at 2 or 4 weeks post-implantation. The area and thickness of the residual disc collagen were measured following staining with streptavidin, and the number of macrophages and blood vessels within the membranes was determined using specific antibodies (to CD68 and transglutaminase II, respectively).
Results
Diabetes significantly reduced the area and thickness of the CMs, while TTC increased CM thickness significantly in both groups of rats at 2 and 4 weeks. Diabetes increased the number of macrophages (∼eightfold at 2 weeks and ∼fourfold at 4 weeks), but TTC had no significant effect. Finally, diabetes increased the number of blood vessels within the discs (∼threefold at 2 weeks and ∼twofold at 4 weeks), while TTC had no effect.
Conclusions
Diabetes increases degradation of native CMs and the number of blood vessels and macrophages within them. TTC immersion delays CM degradation without an apparent effect on macrophage and blood vessel penetration.
Clinical relevance
Enhanced CM degradation in diabetic conditions which impair guided regenerative procedure outcome is apparently related to increased blood vessel formation and macrophage infiltration.





Similar content being viewed by others
References
Lundgren D, Laurell L, Gottlow J, Rylander H, Mathisen T, Nyman S, Rask M (1995) The influence of the design of two different bioresorbable barriers on the results of guided tissue regeneration therapy. An intra-individual comparative study in the monkey. J Periodontol 66:605–612
Patino MG, Neiders ME, Andreana S, Noble B, Cohen RE (2002) Collagen as an implantable material in medicine and dentistry. J Oral Implantol 28:220–225
Pfeifer J, Van Swol RL, Ellinger R (1989) Epithelial exclusion and tissue regeneration using a collagen membrane barrier in chronic periodontal defects: a histologic study. Int J Periodontics Restorative Dent 9:262–273
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Cross-linked and non-cross-linked collagen barrier membranes disintegrate following surgical exposure to the oral environment: a histological study in the cat. Clin Oral Implants Res 19:760–766
Chung KM, Salking LM, Stein MD, Freedman AL (1990) Clinical evaluation of biodegradable collagen membrane in GTR. J Periodontol 61:732–736
Zitzmann NU, Naef R, Schärer P (1997) Resorbable versus nonresorbable membranes in combination with Bio-Oss for guided bone regeneration. Int J Oral Maxillofac Implants 12:844–852
Machtei EE (2001) The effect of membrane exposure on the outcome of regenerative procedures in humans: a meta-analysis. J Periodontol 72:512–516
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Long-term bio-degradation of cross-linked and non-cross-linked collagen barriers in human guided bone regeneration. Clin Oral Implants Res 19:295–230
Reynolds JJ, Hembry RM, Meikle MC (1994) Connective tissue degradation in health and periodontal disease and the roles of matrix metalloproteinases and their natural inhibitors. Adv Dent Res 8:312–319
Armstrong DG, Jude EB (2002) The role of matrix metalloproteinases in wound healing. J Am Podiatr Med Assoc 92:12–18
Visse R, Nagase H (2003) Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res 92:827–839
Minabe M, Kodama T, Kogou T, Tamura T, Hori T, Watanabe Y, Miyata T (1989) Different crosslinked types of collagen implanted in rat palatal gingiva. J Periodontol 60:35–43
Golub LM, McNamara TF, D’Angelo G, Greenwald RA, Ramamurthy NS (1987) A non-antimicrobial chemically modified tetracycline inhibits mammalian collagenase activity. J Dent Res 66:1310–1314
Golub LM, Lee HM, Ryan ME, Giannobile WV, Payne J, Sorsa T (1998) Tetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanisms. Adv Dent Res 12:12–26
Greenwald RA, Golub LM, Ramamurthy NS, Chowdhury M, Moak SA, Sorsa T (1998) In vitro sensitivity of the three mammalian collagenases to tetracycline inhibition: relationship to bone and cartilage degradation. Bone 22:33–38
Moses O, Nemcovsky CE, Tal H, Zohar R (2001) Tetracycline modulates collagen membrane degradation in vitro. J Periodontol 72:1588–1593
Zohar R, Nemcovsky CE, Artzi Z, Kebudi E, Tal H, Moses O (2004) Tetracycline inhibits collagen membrane degradation in-vivo in a dose-dependent manner. J Periodontol 75:1096–1101
Yang C, Zhu P, Yan L, Chen L, Meng R, Lao G (2009) Dynamic changes in matrix metalloproteinase 9 and tissue inhibitor of metalloproteinase1 levels during wound healing in diabetic rats. J Am Podiatr Med Assoc 99:489–496
Eliezer M, Nemcovsky C, Romanos G, Kozlovsky A, Tal H, Kolerman R, Weinreb M, Moses O (2013) Opposing effects of diabetes and tetracycline on the degradation of collagen membranes in rats. J Periodontol 84:529–534
Pfeiffer A, Schatz H (1995) Diabetic microvascular complications and growth factors. Exp Clin Endocrinol Diabetes 103:7–14
Schmidt AM, Yan SD, Brett J, Mora R, Nowygrod R, Stern D (1993) Regulation of human mononuclear phagocyte migration by cell surface-binding proteins for advanced glycation end products. J Clin Invest 91:2155–2168
Radoff S, Vlassara H, Cerami A (1988) Characterization of a solubilized cell surface binding protein on macrophages specific for proteins modified nonenzymatically by advanced glycosylated end products. Arch Biochem Biophys 263:418–423
Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56:549–580
Yamagishi S, Ueda S, Matsui T, Nakamura K, Okuda S (2008) Role of advanced glycation end products (AGEs) and oxidative stress in diabetic retinopathy. Curr Pharm Des 14:962–968 Review
Caldwell RB, Bartoli M, Behzadian MA, El-Remessy AE, Al-Shabrawey M, Platt DH, Liou GI, Caldwell RW (2005) Vascular endothelial growth factor and diabetic retinopathy: role of oxidative stress. Curr Drug Targets 6:511–524
Schwarz F, Rothamel D, Herten M, Sager M, Becker J (2006) Angiogenesis pattern of native and cross-linked collagen membranes: an immunohistochemical study in the rat. Clin Oral Implants Res 17(4):403–409
Han SY, Jee YH, Han KH, et al. (2006) An imbalance between matrix metalloproteinase-2 and tissue inhibitor of matrix metalloproteinase-2 contributes to the development of early diabetic nephropathy. Nephrol Dial Transplant 21:2406–2416
Tesch GH (2007) Role of macrophages in complications of type 2 diabetes. Clin Exp Pharmacol Physiol 34:1016–1019
Tahergorabi Z, Khazaei M (2012) Imbalance of angiogenesis in diabetic complications: the mechanisms. Int J Prev Med 3:827–838
Hoben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56:549–580
Hammes HP, Lin J, Bretzel RG, Brownlee M, Breier G (1998) Upregulation of the vascular endothelial growth factor/vascular endothelial growth factor receptor system in experimental background diabetic retinopathy of the rat. Diabetes 47:401–406
Gardlik R, Fusekova I (2014) Pharmacologic therapy for diabetic retinopathy. Semin Ophthalmol. doi:10.3109/08820538.2013.859280
Nakagawda T, Sato W, Kosugi T, Johnson RJ (2013) Uncoupling of VEGF with endothelial NO as a potential mechanism for abnormal angiogenesis in the diabetic nephropathy. J Diabetes Res 2013:184539
Tilton RG (2002) Diabetic vascular dysfunction: links to glucose-induced reductive stress. Micros Res Tech. 57:390–407
Mathews MK, Merges C, McLeod DS, Lutty GA (1997) Vascular endothelial growth factor and vascular permeability changes in human diabetic retinopathy. Invest Ophthalmol Vis Sci 38:2729–2741
Osaadon P, Fagan XJ, Lifshitz T, Levy J (2014) A review of anti-VEGF agents for proliferative diabetic retinopathy. Eye (Lond) 28:510–520
Unlü F, Güneri PG, Hekimgil M, Yeşilbek B, Boyacioğlu H (2003) Expression of vascular endothelial growth factor in human periodontal tissues: comparison of healthy and diabetic patients. J Periodontol 74:181–187
Carmeli E, Kodesh E, Nemcovsky CE (2009) Tetracycline therapy for muscle atrophy due to immobilization. J Musculoskelet Neuronal Interact 9:81–88
Golub LM, Ramamurthy NS, McNamara TF, Greenwald RA, Rifkin BR (1991) Tetracyclines inhibit connective tissue breakdown: new therapeutic implications for an old family of drugs. Crit Rev Oral Biol Med 2:297–321
Ramamurthy NS, Vernillo AT, Greenwald RA, Lee HM, Sorsa T, Golub LM, Rifkin BR (1993) Reactive oxygen species activate and tetracyclines inhibit rat osteoblast collagenase. J Bone Miner Res 8:1247–1253
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded by an external agency or institute but by internal (departmental) resources.
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in this study were in accordance with the ethical standards of the Tel-Aviv University Faculty of Medicine and were approved by its Animal Care and Use Committee.
Rights and permissions
About this article
Cite this article
Moses, O., Eliezer, M., Nemcovsky, C. et al. Accelerated degradation of collagen membranes in diabetic rats is associated with increased infiltration of macrophages and blood vessels. Clin Oral Invest 20, 1589–1596 (2016). https://doi.org/10.1007/s00784-015-1635-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1635-9