Abstract
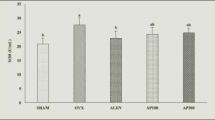
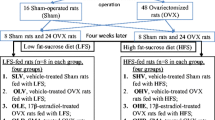
Calcium homeostasis plays vital roles in the management of bone health. Traditional herbal formula Gushukang (GSK) was clinically applied to treat primary osteoporosis. This study aimed to explore the osteoprotective effects of GSK and its roles in maintaining calcium homeostasis in ovariectomized (OVX) mice. The OVX mice were orally treated with low (0.38 g/kg), middle (0.76 g/kg) and high (1.52 g/kg) dose of GSK for 8 weeks. GSK treatment dramatically increased serum calcium level and decreased urinary calcium excretion as well as enhanced calcium content in bone of OVX mice. Serum level of 25-hydroxyvitamin D was significantly increased in OVX mice with exposure to GSK. Treatment with GSK improved bone mass and micro-structure of trabecular bone at distal metaphysis of femur and proximal metaphysis of tibia in OVX mice shown by safranin O staining and micro-CT measurement. GSK treatment at all doses up-regulated mRNA expression of calcium-binding protein-28k and vitamin D receptor in kidney of OVX mice, and dose-dependently decreased mRNA expression of claudin-14 and elevated mRNA expression of claudin-16 in duodenum of OVX mice. Taken together, GSK exerted beneficial effects on trabecular bone of OVX mice by improving calcium homeostasis via regulating paracellular calcium absorption in duodenum and transcellular calcium reabsorption in kidney.







Similar content being viewed by others
References
Tankeu AT, Ndip Agbor V, Noubiap JJ (2017) Calcium supplementation and cardiovascular risk: a rising concern. J Clin Hypertens (Greenwich) 19:640–646
Reid IR, Birstow SM, Bolland MJ (2017) Calcium and cardiovascular disease. Endocrinol Metab (Seoul) 32:339–349
Anderson JJ, Kruszka B, Delaney JA, He K, Burke GL, Alonso A, Bild DE, Budoff M, Michos ED (2016) Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the multi-ethnic study of atherosclerosis (MESA). J Am Heart Assoc 5:e003815
Che CT, Wong MS (2015) Ligustrum lucidum and its constituents: a mini-review on the anti-osteoporosis potential. Nat Prod Commun 10:2189–2194
Strehler EE (2015) Plasma membrane calcium ATPases: from generic Ca(2+) sump pumps to versatile systems for fine-tuning cellular Ca(2.). Biochem Biophys Res Commun 460:26–33
Yu AS (2015) Claudins and the kidney. J Am Soc Nephrol 26:11–19
Gong Y, Hou J (2014) Claudin-14 underlies Ca++-sensing receptor-mediated Ca++ metabolism via NFAT-microRNA-based mechanisms. J Am Soc Nephrol 25:745–760
Zhang Y, Lai WP, Leung PC, Che CT, Wong MS (2008) Improvement of Ca balance by Fructus Ligustri Lucidi extract in aged female rats. Osteoporos Int 19:235–242
Zhang Y, Dong XL, Leung PC, Che CT, Wong MS (2008) Fructus Ligustri Lucidi extract improves calcium balance and modulates the calciotropic hormones level and vitamin D-dependent gene expression in aged ovariectomized rats. Menopause 15:558–565
Feng X, Lyu Y, Wu Z, Fang Y, Xu H, Zhao P, Xu Y, Feng H (2014) Fructus ligustri lucidi ethanol extract improves bone mineral density and properties through modulating calcium absorption-related gene expression in kidney and duodenum of growing rats. Calcif Tissue Int 94:433–441
Lyu Y, Feng X, Zhao P, Wu Z, Xu H, Fang Y, Hou Y, Denney L, Xu Y, Feng H (2014) Fructus Ligustri Lucidi (FLL) ethanol extract increases bone mineral density and improves bone properties in growing female rats. J Bone Miner Metab 32:616–626
Li SQ, Pei ZG, Liu YM (2001) Clinical study on effect of gushukang granule in preventing and treating primary osteoporosis. Zhongguo Zhong Xi Yi Jie He Za Zhi 21:265–268
Wang XJ, Liang RX, Zhao L (2007) Progress of study on prevention and treatment of osteoporosis by compound Gushukang. Zhongguo Zhong Xi Yi Jie He Za Zhi 27:282–285
Zhang Y, Lai WP, Wu CF, Favus MJ, Leung PC, Wong MS (2007) Ovariectomy worsens secondary hyperparathyroidism in mature rats during low Ca diet. Am J Physiol Endocrinol Metab 292:E723–E731
Zhang Y, Papasian CJ, Deng H (2011) Alteration of vitamin D metabolic enzyme expression and calcium transporters abundance in kidney involved in type 1 diabetes-induced bone loss. Osteoporos Int 22:1781–1788
Vandenbroucke A, Luyten FP, Flamaing J, Gielen E (2017) Pharmacological treatment of osteoporosis in the oldest old. Clin Interv Aging 12:1065–1077
Lima GA, Lima PD, Barros Mda G, Vardiero LP, Melo EF, Paranhos-Neto Fde P, Madeira M, Farias ML (2016) Calcium intake: good for the bones but bad for the heart? An analysis of clinical studies. Arch Endocrinol Metab 60:252–263
Verbrugge FH, Gielen E, Milisen K, Boonen S (2012) Who should receive calcium and vitamin D supplementation? Age Ageing 41:576–580
Che CT, Wong MS, Lam CW (2016) Natural products from Chinese medicines with potential benefits to bone health. Molecules 21:239
Zhou ZL, Deng YF, Tao QS, Hu YF, Hou JF (2009) Effects of Gushukang, a Chinese herbal medicine, on bone characteristics and osteoporosis in laying hens. Poult Sci 88:2342–2345
Zhang Y, Diao TY, Wang L, Che CT, Wong MS (2014) Protective effects of water fraction of Fructus Ligustri Lucidi extract against hypercalciuria and trabecular bone deterioration in experimentally type 1 diabetic mice. J Ethnopharmacol 158:239–245
Zhang Y, Leung PC, Che CT, Chow HK, Wu CF, Wong MS (2008) Improvement of bone properties and enhancement of mineralization by ethanol extract of Fructus Ligustri Lucidi. Brit J Nutr 99:494–502
Brech GC, Ciolac EG, Peterson MD, Greve JM (2017) Serum 25-hydroxyvitamin D levels are associated with functional capacity but not with postural balance in osteoporotic postmenopausal women. Clinics (Sao Paulo) 72:11–16
Capatina C, Carsote M, Caragheorgheopol A, Poiana C, Berteanu M (2014) Vitamin D deficiency in postmenopausal women—biological correlates. Maedica (Buchar) 9:316–322
Dong XL, Cao SS, Zhou LP, Denney L, Wong MS, Feng HT (2016) Ethanol extract of Fructus ligustri lucidi increased circulating 1,25(OH)2D3 levels, but did not improve calcium balance in mature ovariectomized rats. Am J Chin Med 44:1237–1253
Will C, Breiderhoff T, Thumfart J, Stuiver M, Kopplin K, Sommer K, Günzel D, Querfeld U, Meij IC, Shan Q, Bleich M, Willnow TE, Müller D (2010) Targeted deletion of murine Cldn16 identifies extra- and intrarenal compensatory mechanisms of Ca2+ and Mg2+ wasting. Am J Physiol Renal Physiol 298:F1152–F1161
Moreira ML, Neto LV, Madeira M, Lopes RF, Farias ML (2018) Vitamin D deficiency and its influence on bone metabolism and density in a Brazilian population of healthy men. J Clin Densitom 21:91–97
Zhou P, Hu J, Xi P, Zhang N, Yang B, Zheng J, Wang X (2017) Survey on the levels of 25-hydroxy vitamin D and bone metabolic markers and evaluation of their correlations with osteoporosis in perimenopausal woman in Xi’an region. PLoS One 12:e0180366
Pike JW, Christakos S (2017) Biology and mechanisms of action of the vitamin D hormone. Endocrinol Metab Clin North Am 46:815–843
Meir T, Levi R, Lieben L, Libutti S, Carmeliet G, Bouillon R, Silver J, Naveh-Many T (2009) Deletion of the vitamin D receptor specifically in the parathyroid demonstrates a limited role for the receptor in parathyroid physiology. Am J Physiol Renal Physiol 297:F1192–F1198
Davey RA, Morris HA (2005) The effects of salmon calcitonin-induced hypocalcemia on bone metabolism in ovariectomized rats. J Bone Miner Metab 23:359–365
Li L, Chen X, Lv S, Dong M, Zhang L, Tu J, Yang J, Zhang L, Song Y, Xu L, Zou J (2014) Influence of exercise on bone remodeling-related hormones and cytokines in ovariectomized rats: a model of postmenopausal osteoporosis. PLoS One 9:e112845
Sela-Brown A, Russell J, Koszewski NJ, Michalak M, Naveh-Many T, Silver J (1998) Calreticulin inhibits vitamin D’s action on the PTH gene in vitro and may prevent vitamin D’s effect in vivo in hypocalcemic rats. Mol Endocrinol 12:1193–1200
Beggs MR, Appel I, Svenningsen P, Skjødt K, Alexander RT, Dimke H (2017) Expression of transcellular and paracellular calcium and magnesium transport proteins in renal and intestinal epithelia during lactation. Am J Physiol Renal Physiol 313:F629–F640
Alexander RT, Rievaj J, Dimke H (2014) Paracellular calcium transport across renal and intestinal epithelia. Biochem Cell Biol 92:467–480
Bouhtiauy I, Lajeunesse D, Christakos S, Brunette MG (1994) Two vitamin D3-dependent calcium binding proteins increase calcium reabsorption by different mechanisms. I. Effect of CaBP 28K. Kidney Int 45:461–468
Chen WF, Mok SK, Wang XL, Lai KH, Lai WP, Luk HK, Leung PC, Yao XS, Wong MS (2011) Total flavonoid fraction of the Herba epimedii extract suppresses urinary calcium excretion and improves bone properties in ovariectomised mice. Br J Nutr 105:180–189
Kim MH, Lee GS, Jung EM, Choi KC, Oh GT, Jeung EB (2009) Dexamethasone differentially regulates renal and duodenal calcium-processing genes in calbindin-D9k and -D28k knockout mice. Exp Physiol 94:138–151
Khanal RC, Nemere I (2008) Endocrine regulation of calcium transport in epithelia. Clin Exp Pharmacol Physiol 35:1277–1287
Gong Y, Hou J (2017) Claudins in barrier and transport function-the kidney. Pflugers Arch 469:105–113
Hou J (2016) Claudins and mineral metabolism. Curr Opin Nephrol Hypertens 25:308–313
Ikari A, Hirai N, Shiroma M, Harada H, Sakai H, Hayashi H, Suzuki Y, Degawa M, Takagi K (2004) Association of paracellin-1 with ZO-1 augments the reabsorption of divalent cations in renal epithelial cells. J Biol Chem 279:54826–54832
Negri AL (2015) Role of claudins in renal calcium handling. Nefrologia 35:347–352
Acknowledgements
This work was supported by Essential Drug Research and Development (2018ZX09201008-003-032) from Ministry of Science and Technology, National Natural Science Foundation of China (81774329), Natural Science Foundation of Shanghai (17ZR1430800), China Postdoctoral Science Foundation (2017M610272), University of Shanghai for Science and Technology (2017KJFZ167), and Longhua Medical Innovation Team Program (LYCX-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
About this article
Cite this article
Li, XL., Wang, L., Bi, XL. et al. Gushukang exerts osteopreserve effects by regulating vitamin D and calcium metabolism in ovariectomized mice. J Bone Miner Metab 37, 224–234 (2019). https://doi.org/10.1007/s00774-018-0924-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-018-0924-1