Abstract
Background
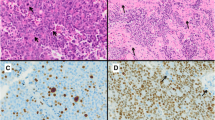
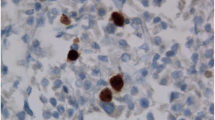
The World Health Organization (WHO) defines atypical pituitary adenomas as tumours with a MIB-1 labelling index ≥3%, p53 positivity and increased mitotic activity. Although a few reports have described the clinical and radiological correlates of atypia in pituitary adenomas, its impact on postoperative outcomes is not clearly defined.
Method
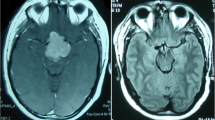
We reviewed preoperative and postoperative records of patients undergoing surgery for pituitary adenomas. Postoperative outcomes for functional adenomas (FPAs) were assessed according to contemporary definitions of remission and recurrence. For non-functional pituitary adenomas (NFPAs), extent of resection and disease progression were defined on the basis of postoperative magnetic resonance imaging.
Results
Of 394 patients included for analysis, 29 cases (7.4%) fulfilled criteria for atypia. Patients with atypical tumours were significantly younger than those with typical adenomas. Remission was possible in 47.4% of FPAs, and was unrelated to the presence of atypia. In NFPAs, local invasiveness was negatively associated with extent of resection (OR, 0.255; 95% CI, 0.086–0.753; p < 0.001). In 93 NFPAs followed postoperatively with serial imaging over a mean duration of 37.5 months, disease progression/recurrence was significantly associated with the presence of atypia (OR, 5.058; 95% CI, 1.273–20.098; p = 0.021) on multivariate analysis.
Conclusions
Patients with atypical non-functional pituitary adenomas are at risk for postoperative recurrence and disease progression, suggesting a need for adjuvant therapy. However, only a small fraction of pituitary tumours demonstrate atypia, as defined by the WHO, limiting its clinical utility.
Similar content being viewed by others
References
Alahmadi H, Lee D, Wilson JR, Hayhurst C, Mete O, Gentili F, Asa SL, Zadeh G (2012) Clinical features of silent corticotroph adenomas. Acta Neurochir (Wein) 154:1493–1498
Batisse M, Raverot G, Maqdasy S, Durando X, Sturm N, Montoriol PF, Kemeny JL, Chazal J, Trouillas J, Tauveron I (2013) Aggressive silent GH pituitary tumor resistant to multiple treatments, including temozolomide. Cancer Investig 31:190–196
Brochier S, Galland F, Kujas M, Parker F, Gaillard S, Raftopoulos C, Young J, Alexopoulou O, Maiter D, Chanson P (2010) Factors predicting relapse of nonfunctioning pituitary macroadenomas after neurosurgery: a study of 142 patients. Eur J Endocrinol 163:193–200
Chacko G, Chacko AG, Kovacs K, Scheithauer BW, Mani S, Muliyil J, Seshadri M (2010) The clinical significance of MIB-1 labeling index in pituitary adenomas. Pituitary 13:337–344
Chang EF, Zada G, Kim S, Lamborn KR, Quinones-Hinojosa A, Tyrrell JB, Wilson CB, Kunwar S (2008) Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J Neurosurg 108:736–745
Chinezu L, Jouanneau E, Vasiljevic A, Trouillas J, Raverot G (2013) Silent GH pituitary tumor: diagnostic and therapeutic challenges. Ann Endocrinol (Paris) 74:491–495
Chinezu L, Vasiljevic A, Trouillas J, Lapoirie M, Jouanneau E, Raverot G (2017) Silent somatotroph tumour revisited from a study of 80 patients with and without acromegaly and a review of the literature. Eur J Endocrinol 176:195–201
Cho HY, Cho SW, Kim SW, Shin CS, Park KS, Kim SY (2010) Silent corticotroph adenomas have unique recurrence characteristics compared with other nonfunctioning pituitary adenomas. Clin Endocrinol 72:648–653
De Caro MDB, Solari D, Pagliuca F, Villa A, Guadagno E, Cavallo LM, Colao A, Pettinato G, Cappabianca P (2017) Atypical pituitary adenomas: clinical characteristics and role of Ki-67 and p53 in prognostic and therapeutic evaluation. A series of 50 patients. Neurosurg Rev 40:105–114
De Paiva Neto MA, Vandergrift A, Fatemi N, Gorgulho AA, DeSalles AA, Cohan P, Wang C, Swerdloff R, Kelly DF (2010) Endonasal transsphenoidal surgery and multimodality treatment for giant pituitary adenomas. Clin Endocrinol 72:512–519
Dekkers O, Pereira A, Roelfsema F, Voormolen J, Neelis K, Schroijen M, Smit J, Romijn J (2006) Observation alone after transsphenoidal surgery for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab 91:1796–1801
DeLellis RA (2004) Pathology and genetics of tumours of endocrine organs. IARC Press, Lyon
Figarella-Branger D, Trouillas J (2006) The new WHO classification of human pituitary tumors: comments. Acta Neuropathol 111:71–72
Gejman R, Swearingen B, Hedley-Whyte ET (2008) Role of Ki-67 proliferation index and p53 expression in predicting progression of pituitary adenomas. Hum Pathol 39:758–766
Grossman AB (2006) The 2004 World Health Organization classification of pituitary tumors: is it clinically helpful? Acta Neuropathol 111:76–77
Hadzhiyanev A, Ivanova R, Nachev E, Elenkova A, Yaneva M, Zaharieva S, Marinov M, Surchev J, Ivanova A (2014) Evaluation of prognostic utility of MIB-1 and p53 expression in pituitary adenomas: correlations with clinical behaviour and follow-up results. Biotechnol Biotechnol Equip 28:502–507
Hentschel SJ, McCutcheon IE, Moore W, Durity FA (2003) P53 and MIB-1 immunohistochemistry as predictors of the clinical behavior of nonfunctioning pituitary adenomas. Can J Neurol Sci 30:215–219
Hofstetter CP, Nanaszko MJ, Mubita LL, Tsiouris J, Anand VK, Schwartz TH (2012) Volumetric classification of pituitary macroadenomas predicts outcome and morbidity following endoscopic endonasal transsphenoidal surgery. Pituitary 15:450–463
Hofstetter CP, Shin BJ, Mubita L, Huang C, Anand VK, Boockvar JA, Schwartz TH (2011) Endoscopic endonasal transsphenoidal surgery for functional pituitary adenomas. Neurosurg Focus 30:E10
Honegger J, Prettin C, Feuerhake F, Petrick M, Schulte-Mönting J, Reincke M (2003) Expression of Ki-67 antigen in nonfunctioning pituitary adenomas: correlation with growth velocity and invasiveness. J Neurosurg 99:674–679
Ioachimescu AG, Eiland L, Chhabra VS, Mastrogianakis GM, Schniederjan MJ, Brat D, Pileggi AV, Oyesiku NM (2012) Silent corticotroph adenomas: Emory University cohort and comparison with ACTH-negative nonfunctioning pituitary adenomas. Neurosurgery 71:296–304
Jane JA Jr, Starke RM, Elzoghby MA, Reames DL, Payne SC, Thorner MO, Marshall JC, Laws ER Jr, Vance ML (2011) Endoscopic transsphenoidal surgery for acromegaly: remission using modern criteria, complications, and predictors of outcome. J Clin Endocrinol Metab 96:2732–2740
Kakade HR, Kasaliwal R, Khadilkar KS, Jadhav S, Bukan A, Khare S, Budyal SR, Goel A, Lila AR, Bandgar T (2014) Clinical, biochemical and imaging characteristics of Cushing’s macroadenomas and their long-term treatment outcome. Clin Endocrinol 81:336–342
Kleinschmidt-DeMasters B (2006) Subtyping does matter in pituitary adenomas. Acta Neuropathol 111:84–85
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–618
Kontogeorgos G (2006) Innovations and controversies in the WHO classification of pituitary adenomas. Acta Neuropathol 111:73–75
Kovacs K (2006) The 2004 WHO classification of pituitary tumors: comments. Acta Neuropathol 111:62–63
Laws ER, Lopes MBS (2006) The new WHO classification of pituitary tumors: highlights and areas of controversy. Acta Neuropathol 111:80–81
Losa M, Franzin A, Mangili F, Terreni MR, Barzaghi R, Veglia F, Mortini P, Giovanelli M (2000) Proliferation index of nonfunctioning pituitary adenomas: correlations with clinical characteristics and long-term follow-up results. Neurosurgery 47:1313–1319
Losa M, Mortini P, Barzaghi R, Ribotto P, Terreni MR, Marzoli SB, Pieralli S, Giovanelli M (2008) Early results of surgery in patients with nonfunctioning pituitary adenoma and analysis of the risk of tumor recurrence. J Neurosurg 108:525–532
Mindermann T, Kovacs K, Wilson CB (1994) Changes in the immunophenotype of recurrent pituitary adenomas. Neurosurgery 35:39–44
Ozer E, Canda MS, Ulukus C, Guray M, Erbayraktar S (2003) Expression of Bcl-2, Bax and p53 proteins in pituitary adenomas: an immunohistochemical study. Tumori 89:54–59
Park P, Chandler WF, Barkan AL, Orrego JJ, Cowan JA, Griffith KA, Tsien C (2004) The role of radiation therapy after surgical resection of nonfunctional pituitary macroadenomas. Neurosurgery 55:100–107
Perry A, Scheithauer BW (2006) Commentary: classification and grading of pituitary tumors. Observations of two working neuropathologists. Acta Neuropathol 111:68–70
Ragel BT, Couldwell WT (2004) Pituitary carcinoma: a review of the literature. Neurosurg Focus 16:E7
Salehi F, Agur A, Scheithauer BW, Kovacs K, Lloyd RV, Cusimano M (2009) Ki-67 in pituitary neoplasms: a review—part I. Neurosurgery 65:429–437
Sarkar S, Rajaratnam S, Chacko G, Chacko AG (2014) Endocrinological outcomes following endoscopic and microscopic transsphenoidal surgery in 113 patients with acromegaly. Clin Neurol Neurosurg 126:190–195
Scheithauer BW, Gaffey TA, Lloyd RV, Sebo TJ, Kovacs KT, Horvath E, Yapcer Ö, Young WF Jr, Meyer FB, Kuroki T (2006) Pathobiology of pituitary adenomas and carcinomas. Neurosurgery 59:341–353
Scheithauer BW, Kurtkaya-Yapcer Ö, Kovacs KT, Young WF Jr, Lloyd RV (2005) Pituitary carcinoma: a clinicopathological review. Neurosurgery 56:1066–1074
Schwyzer L, Starke RM, Jane JA Jr, Oldfield EH (2015) Percent reduction of growth hormone levels correlates closely with percent resected tumor volume in acromegaly. J Neurosurg 122:798–802
Tanaka Y, Hongo K, Tada T, Sakai K, Kakizawa Y, Kobayashi S (2003) Growth pattern and rate in residual nonfunctioning pituitary adenomas: correlations among tumor volume doubling time, patient age, and MIB-1 index. J Neurosurg 98:359–365
Thapar K, Kovacs K, Scheithauer BW, Stefaneanu L, Horvath E, Pernicone PJ, Murray D, Laws ER Jr (1996) Proliferative activity and invasiveness among pituitary adenomas and carcinomas: an analysis using the MIB-1 antibody. Neurosurgery 38:99–107
Thapar K, Scheithauer BW, Kovacs K, Pernicone PJ, Laws ER Jr (1996) p53 expression in pituitary adenomas and carcinomas: correlation with invasiveness and tumor growth fractions. Neurosurgery 38:765–771
Trouillas J, Roy P, Sturm N, Dantony E, Cortet-Rudelli C, Viennet G, Bonneville J-F, Assaker R, Auger C, Brue T (2013) A new prognostic clinicopathological classification of pituitary adenomas: a multicentric case–control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol 126:123–135
van Bunderen CC, van Varsseveld NC, Baayen JC, van Furth WR, Aliaga ES, Hazewinkel MJ, Majoie CB, Freling NJ, Lips P, Fliers E (2013) Predictors of endoscopic transsphenoidal surgery outcome in acromegaly: patient and tumor characteristics evaluated by magnetic resonance imaging. Pituitary 16:158–167
Widhalm G, Wolfsberger S, Preusser M, Fischer I, Woehrer A, Wunderer J, Hainfellner JA, Knosp E (2009) Residual nonfunctioning pituitary adenomas: prognostic value of MIB-1 labeling index for tumor progression. J Neurosurg 111:563–571
Wolfsberger S, Knosp E (2006) Comments on the WHO 2004 classification of pituitary tumors. Acta Neuropathol 111:66–67
Wolfsberger S, Wunderer J, Zachenhofer I, Czech T, Böcher-Schwarz H-G, Hainfellner J, Knosp E (2004) Expression of cell proliferation markers in pituitary adenomas–correlation and clinical relevance of MIB-1 and anti-topoisomerase-IIα. Acta Neurochir (Wein) 146:831–839
Zada G, Woodmansee WW, Ramkissoon S, Amadio J, Nose V, Laws ER Jr (2011) Atypical pituitary adenomas: incidence, clinical characteristics, and implications: clinical article. J Neurosurg 114:336–344
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Sarkar, S., Philip, V.J., Cherukuri, S.K. et al. Implications of the World Health Organization definition of atypia on surgically treated functional and non-functional pituitary adenomas. Acta Neurochir 159, 2179–2186 (2017). https://doi.org/10.1007/s00701-017-3223-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3223-z