Abstract
Background
Selective amygdalohippocampectomy (SAH) is an accepted surgical procedure for treatment of pharmacoresistant mesial temporal lobe epilepsy, but it may lead to postoperative visual field deficits (VFDs). Here we present a prospective randomised trial comparing the postoperative VFDs after either a trans-sylvian or temporobasal approach for SAH.
Method
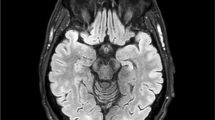
Forty-eight patients were randomly assigned to trans-sylvian (n = 24) or temporobasal (n = 24) SAH. Postoperative VFD were quantitatively evaluated using automated static and kinetic perimetry. In 24 cases, diffusion tensor imaging-based deterministic fibre-tracking of the optic radiation was performed. The primary endpoint was absence of postoperative VFD. The secondary endpoint was seizure outcome and driving ability.
Results
Three patients (13 %) from the trans-sylvian group showed no VFD, compared to 11 patients (46 %) from the temporobasal group without VFD (p = 0.01, RR = 3.7; CI = 1.2–11.5). Fifteen patients from each group (63 %) became completely seizure-free (ILAE1). Among those seizure-free cases, five trans-sylvian (33 %) and ten temporobasal (66 %) patients could apply for a driving licence (NNT = 3) when VFDs were considered. Although the trans-sylvian group experienced more frequent VFDs, the mean functional visual impairment showed a tendency to be less pronounced compared with the temporobasal group. DTI-based tracking of the optic radiation revealed that a lower distance of optic radiation to the temporal base correlated with increased rate of VFD in the temporobasal group.
Conclusions
Temporobasal SAH shows significantly fewer VFDs and equal seizure-free rate compared with the trans-sylvian SAH. However, in patients in whom the optic radiation is close to the temporal base, the trans-sylvian approach may be a preferred alternative.



Similar content being viewed by others
References
Bailey P, Gibbs F (1951) The surgical treatment of psychomotor epilepsy. J Am Med Assoc 145(6):365–370
Baker GA, Jacoby A, Buck D, Stalgis C, Monnet D (1997) Quality of life of people with epilepsy: a European study. Epilepsia 38(3):353–362
Behrens E, Schramm J, Zentner J, König R (1997) Surgical and neurological complications in a series of 708 epilepsy surgery procedures. Neurosurgery 41(1):1–10
Beisse F, Lagrèze WA, Schmitz J, Schulze-Bonhage A (2014) Visual field defects after epilepsy surgery. Ophthalmologe 111(10):942–947
Benjamin CFA, Singh JM, Prabhu SP, Warfield SK (2012) Optimization of tractography of the optic radiations. Hum Brain Mapp 35(2):683–697
Clusmann H, Kral T, Gleissner U, Sassen R, Urbach H, Blumcke I, Bogucki J, Schramm J (2004) Analysis of Different Types of Resection for Pediatric Patients with Temporal Lobe Epilepsy. Neurosurgery 54(4):847–860
Ebeling U, Reulen HJ (1988) Neurosurgical topography of the optic radiation in the temporal lobe. Acta Neurochir (Wien) 92(1–4):29–36
Egan RA, Shults WT, So N, Burchiel K, Kellogg JX, Salinsky M (2000) Visual field deficits in conventional anterior temporal lobectomy versus amygdalohippocampectomy. Neurology 55(12):1818–1822
Falconer MA, Wilson JL (1958) Visual field changes following anterior temporal lobectomy: their significance in relation to Meyer’s loop of the optic radiation. Brain 81(1):1–14
Falconer MA, Meyer A, Hill D, Mitchell W, Pond DA (1955) Treatment of temporal-lobe epilepsy by temporal lobectomy; a survey of findings and results. Lancet 268(6869):827–835
Helmstaedter C, Elger CE, Hufnagel A, Zentner J, Schramm J (1996) Different effects of left anterior temporal lobectomy, selective amygdalohippocampectomy, and temporal cortical lesionectomy on verbal learning, memory, and recognition. J Epilepsy 9:39–45
Hori T, Yamane F, Ochiai T, Kondo S, Shimizu S, Ishii K, Miyata H (2007) Selective subtemporal amygdalohippocampectomy for refractory temporal lobe epilepsy: operative and neuropsychological outcomes. J Neurosurg 106(1):134–141
Jeelani NUO, Jindahra P, Tamber MS, Poon TL, Kabasele P, James-Galton M, Stevens J, Duncan J, McEvoy AW, Harkness W, Plant GT (2010) ‘Hemispherical asymmetry in the Meyer’s Loop’: a prospective study of visual-field deficits in 105 cases undergoing anterior temporal lobe resection for epilepsy. J Neurol Neurosurg Psychiatr 81(9):985–991
Josephson CB, Dykeman J, Fiest KM, Liu X, Sadler RM, Jetté N, Wiebe S (2013) Systematic review and meta-analysis of standard vs selective temporal lobe epilepsy surgery. Neurology 80(18):1669–1676
Kral T, Clusmann H, Urbach J, Schramm J, Elger CE, Kurthen M, Grunwald T (2002) Preoperative evaluation for epilepsy surgery (Bonn Algorithm). Zentralbl Neurochir 63(3):106–110
Lilja Y, Ljungberg M, Starck G, Malmgren K, Rydenhag B, Nilsson DT (2014) Visualizing Meyer’s loop: a comparison of deterministic and probabilistic tractography. Epilepsy Res 108(3):481–490
Lutz MT, Mayer T, Schiefer U (2011) Recommendations for a standardized perimetry within the framework of epilepsy surgery. Ophthalmologe 108(7):628–636
Lutz MT, Clusmann H, Elger CE, Schramm J, Helmstaedter C (2004) Neuropsychological outcome after selective amygdalohippocampectomy with transsylvian versus transcortical approach: a randomized prospective clinical trial of surgery for temporal lobe epilepsy. Epilepsia 45(7):809–816
Manji H, Plant GT (2000) Epilepsy surgery, visual fields, and driving: a study of the visual field criteria for driving in patients after temporal lobe epilepsy surgery with a comparison of Goldmann and Esterman perimetry. J Neurol Neurosurg Psychiatr 68(1):80–82
Marino R, Rasmussen T (1968) Visual field changes after temporal lobectomy in man. Neurology 18(9):825–835
Martens T, Merkel M, Holst B, Brückner K, Lindenau M, Stodieck S, Fiehler J, Westphal M, Heese O (2014) Vascular events after transsylvian selective amygdalohippocampectomy and impact on epilepsy outcome. Epilepsia 55(5):763–769
Mengesha T, Abu-Ata M, Haas KF, Lavin PJ, Sun DA, Konrad PE, Pearson M, Wang L, Song Y, Abou-Khalil BW (2009) Visual field defects after selective amygdalohippocampectomy and standard temporal lobectomy. J Neuroophthalmol 29(3):208–213
Mills RP, Drance SM (1986) Esterman disability rating in severe glaucoma. Ophthalmology 93(3):371–378
Olivier A (2000) Transcortical selective amygdalohippocampectomy in temporal lobe epilepsy. Can J Neurol Sci 27(Suppl 1):S68–96
Penfield W, Baldwin M (1952) Temporal lobe seizures and the technic of subtotal temporal lobectomy. Ann Surg 136(4):625–634
Ray A, Pathak-Ray V, Walters R, Hatfield R (2002) Driving after epilepsy surgery: effects of visual field defects and epilepsy control. Br J Neurosurg 16(5):456–460
von Rhein B, Nelles M, Urbach H, von Lehe M, Schramm J, Helmstaedter C (2012) Neuropsychological outcome after selective amygdalohippocampectomy: subtemporal versus transsylvian approach. J Neurol Neurosurg Psychiatr 83(9):887–893
Rubino PA, Rhoton AL Jr, Tong X, de Oliveira E (2005) Three-dimensional relationships of the optic radiation. Neurosurgery 57(Suppl 4):219–227
Sander JW, Shorvon SD (1996) Epidemiology of the epilepsies. J Neurol Neurosurg Psychiatr 61(5):433–443
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7(6):525–537
Sperling MR, Feldman H, Kinman J, Liporace JD, O’Connor MJ (1999) Seizure control and mortality in epilepsy. Ann Neurol 46(1):45–50
Thudium MO, Campos AR, Urbach H, Clusmann H (2010) The basal temporal approach for mesial temporal surgery: sparing the Meyer loop with navigated diffusion tensor tractography. Neurosurgery 67(ONS Suppl 2):385–390
Weber J, Schiefer U, Kolling G (2004) Proposed scoring system for assessment of functional impairment due to visual field defects. Ophthalmologe 101(10):1030–1033
Wiebe S, Blume WT, Girvin JP, Eliasziw M, Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group (2001) A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 345(5):311–318
Wieser HG, Blume WT, Fish D, Goldensohn E, Hufnagel A, King D, Sperling MR, Lüders H, Pedley TA, Commission on Neurosurgery of the International League Against Epilepsy (ILAE) (2001) ILAE Commission Report. Proposal for a new classification of outcome with respect to epileptic seizures following epilepsy surgery. Epilepsia 42(2):282–286
Winston GP, Daga P, White MJ, Micaleff C, Miserocchi A, Mancini L, Modat M, Stretton J, Sidhu MK, Symms MR, Lythgoe DJ, Thornton J, Yousry TA, Ourselin S, Duncan JS, McEvoy AW (2014) Preventing visual field deficits from neurosurgery. Neurology 83(7):604–611
Winston GP (2013) Epilepsy surgery, vision, and driving: What has surgery taught us and could modern imaging reduce the risk of visual deficits? Epilepsia 54(11):1877–1888
Winston GP, Daga P, Stretton J, Modat M, Symms MR, McEvoy AW, Ourselin S, Duncan JS (2012) Optic radiation tractography and vision in anterior temporal lobe resection. Ann Neurol 71(3):334–341
Winston GP, Yogarajah M, Symms MR, McEvoy AW, Micallef C, Duncan JS (2011) Diffusion tensor imaging tractography to visualize the relationship of the optic radiation to epileptogenic lesions prior to neurosurgery. Epilepsia 52(8):1430–1438
Yamamoto T, Yamada K, Nishimura T, Kinoshita S (2005) Tractography to depict three layers of visual field trajectories to the calcarine gyri. Am J Ophthalmol 140(5):781–785
Yaşargil MG, Krayenbühl N, Roth P, Hsu SPC, Yaşargil DCH (2010) The selective amygdalohippocampectomy for intractable temporal limbic seizures. J Neurosurg 112(1):168–185
Yeni SN, Tanriover N, Uyanik Ö, Ulu MO, Özkara Ç, Karaağaç N, Ozyurt E, Uzan M (2008) Visual field defects in selective amygdalohippocampectomy for hippocampal sclerosis: the fate of Meyer’s loop during the transsylvian approach to the temporal horn. Neurosurgery 63(3):507–515
Acknowledgments
We thank R.D. Ormond MD for language editing of the manuscript. We thank R. Fimmers MD for providing the randomisation list. We wish to acknowledge the contribution of other colleagues who maintained the epilepsy surgery database in the past at the Department of Neurosurgery: T. Kral MD and E. Behrens MD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.S. received reimbursement for congress costs from several scientific societies. C.E.E. is consultant for Desitin and Novartis and received honoraria for talks from Pfizer and Eisai. The funding sources had no role in the design of the study, interpretation of the results, or in the writing of the manuscript. None of the other authors has any conflict of interest to disclose.
Funding
Patients’ follow-up was funded as part of the transregional collaborative research consortium SFB-TR3 “Mesial temporal lobe epilepsies” of the Deutsche Forschungsgemeinschaft (DFG).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Delev, D., Wabbels, B., Schramm, J. et al. Vision after trans-sylvian or temporobasal selective amygdalohippocampectomy: a prospective randomised trial. Acta Neurochir 158, 1757–1765 (2016). https://doi.org/10.1007/s00701-016-2860-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2860-y