Abstract
Background
In order to reduce the consequences of narcotic-related side effects and provide effective analgesia after craniotomy, we conducted a randomized trial to compare the analgesic efficacy of preemptive scalp infiltrations with 1 % lidocaine and 0.5 % ropivacaine on the postoperative pain.
Methods
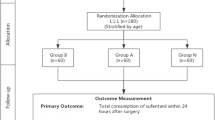
Sixty adult patients scheduled for craniotomy were enrolled. A solution contained 0.5 % ropivacaine and 1 % lidocaine (40 ml) was prepared. In group A, local anesthetic was injected throughout the entire thickness of the scalp before skin incision. In group B, it was injected before skin closure. Additional intravenous injection and patient-controlled analgesia with morphine was used to control postoperative pain if the verbal numerical rating scale > 4. Cumulative morphine consumption; numerical rating scale of pain at 1, 2, 4, 6, 8, 12, and 24 h; postoperative nausea, vomiting, and respiratory depression, were recorded for 24 h after the operation.
Results
Postoperative pain scores were lower in group A than in group B within the first 6 h after surgery. Mean time to demand for postoperative analgesic was statistically (p < 0.001) delayed in group A 300 (240, 360) min compared to group B 150 (105, 200) min. Ten patients in group A received morphine analgesia was half less than 21 patients in group B (p < 0.006). The median morphine consumption in 24 h after operation in group A 10.5 (8, 15) mg was less than that in group B 28 (22.5, 30.5) mg (p < 0.001).
Conclusions
Preemptive scalp infiltration with 0.5 % ropivacaine and 1 % lidocaine provides effective postoperative analgesia after craniotomy.

Similar content being viewed by others

References
Bao GX, Liu JJ, Zu TB (1987) Intravenous procaine is a useful addition to balanced anesthesia for thoracic surgery. J Cardiothorac Anesth 1:500–501
Barcznski M, Konturek A, Herman RM (2006) Superiority of preemptive analgesia with intraperitoneal instillation of bupivacaine before rather than after the creation of pneumoperitoneum for laparoscopic cholecystectomy: a randomized, double-blind, placebo-controlled study. Surg Endosc 20:1088–1093
Bashir MM, Shahzad MA, Yousaf MN (2014) Comparison of postoperative pain relief by intercostals block between pre-rib harvest and post-rib harvest groups. J Coll Physicians Surg Pak 24:43–46
Batoz H, Verdonck O, Pellerin C (2009) The analgesic properties of scalp infiltration with ropivacaine after intracranial tumoral resection. Anesth Analg 109:240–244
Benedittis DG, Lorenzetti A, Spagnoli D (1996) Postoperative pain in neurosurgery: a pilot study in brain surgery. Neurosurgery 38:466–470
Biswas BK, Bithal PK (2003) Preincision 0.25% bupivacaine scalp infiltration and postcraniotomy pain: a randomized double-blind, placebo-controlled study. J Neurosurg Anesthesiol 15:234–239
Bloomfield EL, Schubert A, Secic M (1998) The influence of scalp infiltration with bupivacaine on hemodynamics and postoperative pain in adult patients undergoing craniotomy. Anesth Analg 87:579–582
Coughlin SM, Karanicolas PJ, Emmerton-Coughlin HM (2010) Better late than never? Impact of local analgesia timing on postoperative pain in laparoscopic surgery: a systematic review and metaanalysis. Surg Endosc 24:3167–3176
Ersayli DT, Gurbet A, Bekar A (2006) Effects of perioperatively administered bupivacaine and bupivacaine-methylprednisolone on pain after lumbar discectomy. Spine 31:2221–2226
Gazoni FM, Pouratian N, Nemergut EC (2008) Effect of ropivacaine skull block on perioperative outcomes in patients with supratentorial brain tumors and comparison with remifentanil: a pilot study. J Neurosurg 109:44–49
Gray LC, Matta BF (2005) Acute and chronic pain following craniotomy: a review. Anaesthesia 60:693–704
Guilfoyle MR, Helmy A, Duane D (2013) Regional scalp block for postcraniotomy analgesia: a systematic review and meta-analysis. Anesth Analg 116:1093–1102
Gurbet A, Bekar A, Bilgin H (2008) Pre-emptive infiltration of levobupivacaine is superior to at-closure administration in lumbar laminectomy patients. Eur Spine J 17:1237–1241
Hansen MS, Brennum J, Moltke FB (2011) Pain treatment after craniotomy: where is the (procedure-specific) evidence? A qualitative systematic review. Eur J Anaesthesiol 28:821–829
Johnson SM, Saint John BE, Dine AP (2008) Local anesthetics as antimicrobial agents: a review. Surg Infect 9:205–213
Ju NY, Cui GX, Gao W (2013) Ropivacaine plus dexamethasone infiltration reduces postoperative pain after tonsillectomy and adenoidectomy. Int J Pediatr Otorhinolaryngol 77:1881–1885
Kampe S, Poetter C, Buzello S (2003) Ropivacaine 0.1% with sufentanil 1 microg/L inhibits in vitro growth of Pseudomonas aeruginosa and does not promote multiplication of Staphylococcus aureus. Anesth Analg 97:409–411
Katz J, Cohen L, Schmid R (2003) Postoperative morphine use and hyperalgesia are reduced by preoperative but not intraoperative epidural analgesia: implications for preemptive analgesia and the prevention of central sensitization. Anesthesiology 98:1449–1460
Kaufman E, Epstein JB, Gorsky M (2005) Preemptive analgesia and local anesthesia as a supplement to general anesthesia: a review. Anesth Prog 52:29–38
Kawamata M, Takahashi T, Kozuka Y (2002) Experimental incision-induced pain in human skin: effect of systemic lidocaine on flare formation and hyperalgesia. Pain 100:77–89
Lawkoune JD, Szekely B, Fermanian C (2005) Scalp infiltration with bupivacaine plus epinephrine or plain ropivacaine reduces postoperative pain after supratentorial craniotomy. J Neurosurg Anesthesiol 17:139–143
Lee IO, Kim SH, Kong MH (2001) Pain after laparoscopic cholecystectomy: the effect and timing of incisional and intraperitoneal bupivacaine. Can J Anaesth 48:545–550
Leone S, Di Cianni S, Casati A (2008) Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine, and levobupivacaine. Acta Biomed 79:92–105
Mordhorst C, Latz B, Kerz T (2010) Prospective assessment of postoperative pain after craniotomy. J Neurosurg Anesthesiol 22:202–206
Pakulski C, Nowicki R, Badowica B (2001) Effect of scalp infiltration with lidocaine on the circulatory response to craniotomy. Med Sci Monit 7:725–728
Pina-Vaz C, Rodrigues AG, Sansoenetty F (2000) Antifungal activity of local anesthetics against Candida species. Infect Dis Obstet Gynecol 8:124–137
Pogatzki-Zahn EM, Zahn PK (2006) From preemptive to preventive analgesia. Curr Opin Anaesthesiol 19:551–555
Rodrigues A, Pina-Vaz C, Mrdh PA (2000) Inhibition of germ tube formation by Candida albicans by local anesthetics: an effect related to ionic channel blockade. Curr Microbiol 40:145–148
Saringcarinkul A, Boonsri S (2008) Effect of scalp infiltration on postoperative pain relief in elective supratentorial craniotomy with 0.5% bupivacaine with adrenaline 1:400 000. J Med Assoc Thail 91:1518–1523
Tamanai-Shacoori Z, Shacorri V, Van Vo JM (2004) Sufentanil modifies the antibacterial activity of bupivacaine and ropivacaine. Can J Anaesth 51:911–914
Verchere E, Grenier B, Mesli A (2002) Postoperative pain management after supratentorial craniotomy. J Neurosurg Anesthesiol 14:96–101
Woolf CJ, Chong MS (1993) Preemptive analgesia: treating postoperative pain by preventing the establishment of sensitization. Anesth Analg 77:362–379
Yu H, Li ZY, Yu X (2013) Efficacy of postoperative continuous wound infiltration with local anesthesia after open hepatectomy. Zhonghua Yi Xue ZaZhi 93:2723–2726
Ethical standards
We state that all persons have given their informed consent prior to their inclusion in the study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Song, J., Li, L., Yu, P. et al. Preemptive scalp infiltration with 0.5 % ropivacaine and 1 % lidocaine reduces postoperative pain after craniotomy. Acta Neurochir 157, 993–998 (2015). https://doi.org/10.1007/s00701-015-2394-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2394-8