Abstract
Purpose
The feasibility of living donor liver transplantation (LDLT) using left lobe (LL) grafts has been demonstrated. However, the long-term outcome of the hepatocellular carcinoma (HCC) patients with LL grafts has not been elucidated. The aim of this study was to analyze the long-term outcomes after LDLT for HCC according to the graft type.
Methods
A retrospective analysis was performed evaluating the outcomes of LL graft recipients (n = 82) versus recipients of RL grafts (n = 46). The analysis endpoints were the overall and recurrence-free survival after LDLT. The demographics of both recipients and donors, and the tumor characteristics associated with the graft type were also analyzed.
Results
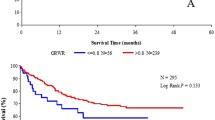
The graft volume (436 ± 74 g), as well as the graft volume-standard liver volume rate (38.3 ± 6.2%) of the LL graft group were significantly decreased as compared to those of the RL graft group (569 ± 82 g, 46.3 ± 6.7%; p < 0.01). The 1-, 3-, 5- and 7-year overall survival rates of the LL graft group were 88.2, 80.2, 75.7 and 72.4%, respectively, which were not significantly different compared to those of the RL graft group (95.4, 87.3, 87.3 and 87.3%). The recurrence-free survival rates of the LL graft group (89.1% at 1 year, 78.8% at 3 years, 75.8% at 5 years and 70.3% at 7 years) were similar to those of the RL graft group (88.6, 88.6, 88.6 and 88.6%). The mean peak postoperative total bilirubin levels and duration of hospital stay after surgery for the LL grafting donors were significantly decreased as compared to those of the RL grafting donors (p < 0.01). The rate of severe complications (over Clavien’s IIIa) associated with LL graft procurement was 6.2%, which was lower than that in the RL graft group (15.6%).
Conclusions
The long-term outcomes in the HCC patients with LL grafts were similar to those of patients receiving RL grafts, and the outcomes of the donors of LL grafts were more favorable. Therefore, LL grafts should be considered when selecting LDLT for HCC to ensure donor safety.


Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- CL:
-
Caudate lobe
- CT:
-
Computed tomography
- DCP:
-
Des-gamma-carboxy prothrombin
- DDLT:
-
Deceased donor liver transplantation
- GRWR:
-
Graft-recipient weight ratio
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- LDLT:
-
Living donor liver transplantation
- LL:
-
Left lobe
- LT:
-
Liver transplantation
- MMF:
-
Mycophenolate mofetil
- RL:
-
Right lobe
- RV:
-
Remnant liver volume
- SLV:
-
Standard liver volume
- TLV:
-
Total liver volume
References
Todo S, Furukawa H. Living donor liver transplantation for adult patients with hepatocellular carcinoma: experience in Japan. Ann Surg.2004;240:451–9 (discussion).
Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10:35–43.
Yao FY. Liver transplantation for hepatocellular carcinoma: beyond the Milan criteria. Am J Transplant. 2008;8:1982–9.
Taketomi A, Sanefuji K, Soejima Y, Yoshizumi T, Uhciyama H, Ikegami T, et al. Impact of des-gamma-carboxy prothrombin and tumor size on the recurrence of hepatocellular carcinoma after living donor liver transplantation. Transplantation. 2009;87:531–7.
Fujiki M, Takada Y, Ogura Y, Oike F, Kaido T, Teramukai S, et al. Significance of des-gamma-carboxy prothrombin in selection criteria for living donor liver transplantation for hepatocellular carcinoma. Am J Transplant. 2009;9:2362–71.
Sugawara Y, Tamura S, Makuuchi M. Living donor liver transplantation for hepatocellular carcinoma: Tokyo University series. Dig Dis. 2007;25:310–2.
Konishi N, Ishizaki Y, Sugo H, Yoshimoto J, Miwa K, Kawasaki S. Impact of a left-lobe graft without modulation of portal flow in adult-to-adult living donor liver transplantation. Am J Transplant. 2008;8:170–4.
Yonemura Y, Taketomi A, Soejima Y, Yoshizumi T, Uchiyama H, Gion T, et al. Validity of preoperative volumetric analysis of congestion volume in living donor liver transplantation using three-dimensional computed tomography. Liver Transpl. 2005;11:1556–62.
Fisher RA, Kulik LM, Freise CE, Lok AS, Shearon TH, Brown RS Jr, et al. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007;7:1601–8.
Taketomi A, Soejima Y, Yoshizumi T, Uchiyama H, Yamashita Y, Maehara Y. Liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2008;15:124–30.
Soejima Y, Taketomi A, Yoshizumi T, Uchiyama H, Harada N, Ijichi H, et al. Feasibility of left lobe living donor liver transplantation between adults: an 8-year, single-center experience of 107 cases. Am J Transplant. 2006;6:1004–11.
Taketomi A, Kayashima H, Soejima Y, Yoshizumi T, Uchiyama H, Ikegami T, et al. Donor risk in adult-to-adult living donor liver transplantation: impact of left lobe graft. Transplantation. 2009;87:445–50.
Taketomi A, Morita K, Toshima T, Takeishi K, Kayashima H, Ninomiya M, et al. Living donor hepatectomies with procedures to prevent biliary complications. J Am Coll Surg. 2010;211:456–64.
Bhangui P, Vibert E, Majno P, Salloum C, Andreani P, Zocrato J, et al. Intention-to-treat analysis of liver transplantation for hepatocellular carcinoma: living versus deceased donor transplantation. Hepatology. 2011;53:1570–9.
Shi JH, Huitfeldt HS, Suo ZH, Line PD. Growth of hepatocellular carcinoma in the regenerating liver. Liver Transpl. 2011; doi:10.1002/lt.22325.
Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Small-sized liver graft does not increase the risk of hepatocellular carcinoma recurrence after living donor liver transplantation. Transplant Proc. 2007;39:1526–9.
Hwang S, Lee SG, Joh JW, Suh KS, Kim DG. Liver transplantation for adult patients with hepatocellular carcinoma in Korea: comparison between cadaveric donor and living donor liver transplantations. Liver Transpl. 2005;11:1265–72.
Li C, Wen TF, Yan LN, Li B, Yang JY, Wang WT, et al. Outcome of hepatocellular carcinoma treated by liver transplantation: comparison of living donor and deceased donor transplantation. Hepatobiliary Pancreat Dis Int. 2010;9:366–9.
Trotter JF, Adam R, Lo CM, Kenison J. Documented deaths of hepatic lobe donors for living donor liver transplantation. Liver Transpl. 2006;12:1485–8.
Acknowledgments
We thank Professor Brian Quinn for his review of this manuscript.
Conflict of interest
None of the authors has any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taketomi, A., Shirabe, K., Toshima, T. et al. The long-term outcomes of patients with hepatocellular carcinoma after living donor liver transplantation: a comparison of right and left lobe grafts. Surg Today 42, 559–564 (2012). https://doi.org/10.1007/s00595-011-0086-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-011-0086-4