Abstract
Background
Traditional treatment recommendations in the surgical treatment of scoliosis in Duchenne muscular dystrophy have included instrumentation and fusion to the sacrum/pelvis to correct pelvic obliquity and to restore the sitting balance of the trunk. However, caudal extent of instrumentation and fusion has remained a matter of considerable debate. This study was performed to determine the efficacy and safety of stopping segmental pedicle screw constructs at L5 in the surgical treatment of scoliosis in Duchenne muscular dystrophy (DMD), with mild pelvic obliquity (<15°).
Materials and methods
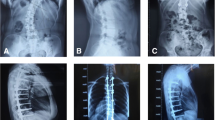
From May 2005 to June 2007, a total of 22 consecutive patients underwent posterior spinal fusion and segmental pedicle screw instrumentation only to L5 for scoliosis secondary to DMD. A minimum 2-year follow-up was required for inclusion in this study. Assessment was performed clinically and with radiologic measurements. Radiologic measurements included the Cobb angles of the curves in the coronal plane, thoracic kyphosis and lumbar lordosis in the sagittal plane, and pelvic obliquity. The operating time, blood loss, and complications were evaluated.
Results
Twenty patients, aged 11–17, were enrolled. The average follow-up period was 35 months. Preoperative coronal curves averaged 70° (range: 51–85°), with a postoperative mean of 15° (range: 8–25°) and 17° (range: 9–27°) at the last follow-up. Pelvic obliquity improved from 13° (range: 7–15°) preoperatively to 5° (range: 3–8°) postoperatively and 6° (range: 3–9°) at the last follow-up. Good sagittal plane alignment was recreated and maintained. No loss of correction of scoliosis and pelvic obliquity was noted. The mean operating time was 271 min (range: 232–308 min). The mean intraoperative blood loss was 890 ml (range: 660–1260 ml). The mean total blood loss was 2100 ml (range: 1250–2880 ml).There was no major complication.
Conclusion
Segmental pedicle screw instrumentation and fusion to L5 is effective and safe in patients with scoliosis secondary to DMD without significant pelvic obliquity initially and long term, obviating the need for fixation to the sacrum/pelvis. There was no major complication.


Similar content being viewed by others
References
Allen B Jr, Ferguson R (1982) The Galveston technique for L rod instrumentation of the scoliotic spine. Spine 10:276–284
Askin GN, Hallettv R, Hare N, Webb JK (1997) The outcome of scoliosis surgery in the severely handicapped child: an objective and subjective assessment. Spine 22:44–50
Basobas L, Mardjerko S, Hammerberg K, Lubicky J (2003) Selective anterior fusion and instrumentation for the treatment of neuromuscular scoliosis. Spine 28:S245–S248
Bell DF, Moseley CF, Koreska J (1989) Unit rod segmental spinal instrumentation in the management of patients with progressive neuromuscular spinal deformity. Spine 14:1301–1307
Benson ER, Thomson JD, Smith BG, Banta JV (1998) Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine 23:2308–2317
Bentley G, Haddad F, Bull TM, Seingry D (2001) The treatment of scoliosis in muscular dystrophy using modified Luque and Harrington-Luque instrumentation. J Bone Joint Surg Br 83:22–28
Daher Y, Lonstein J, Winter R, Bradford D (1985) Spinal surgery in spinal muscular atrophy. J Pediatr Orthop 5:391–395
Dias RC, Miller F, Dabney K, Lipton G, Thomas TT (1996) Surgical correction of spinal deformity using a unit rod in children with cerebral palsy. J Pediatr Orhop 16:734–740
Frischut B, Krismer M, Stoeckl B (2000) Pelvic tilt in neuromuscular disorders. J Pediatr Orthop B 9:221–228
Gaine WJ, Lim J, Stephenson W, Galasko CBS (2004) Progression of scoliosis after spinal fusion in Duchenne muscular dystrophy. J Bone Joint Surg Br 86:550–555
Galasko CBS, Delany C, Morris P (1992) Spinal stabilisation in Duchenne muscular dystrophy. J Bone Joint Surg Br 74:210–220
Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K (2005) Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J 17:255–261
Heller KD, Wirtz DC, Siebert CH, Forst R (2001) Spinal stabilization in Duchenne muscular dystrophy: principles of treatment and record of 31 operative treated cases. J Pediatr Orthop B 10:18–24
Hsu JD (1983) The natural history of spinal curve progression in the nonambulatory Duchenne muscular dystrophy patient. Spine 8:771–775
Lowenstein JE, Hiroko Matsumoto, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, Hyman JE, Roye DP (2007) Coronal and sagittal plane correction in adolescent idiopathic scoliosis–a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 32:448–452
Luk KD, Ho HC, Leong JC (1986) Iliolumbar ligament. J Bone Joint Surg Br 68:197–200
Marsh A, Edge G, Lehovsky J (2003) Spinal fusion in patients with Duchenne muscular dystrophy and a low forced vital capacity. Euro Spine J 12:507–512
McCall RE, Hayes B (2005) Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine 30:2056–2060
McCord DH, Cunningham BW, Shono Y et al (1992) Biomechanical analysis of lumbosacral fixation. Spine 17:S235–S243
Miladi LT, Ghanem TB, Draui MM, Zeller RD, Dubousset JF (1997) Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis. Spine 22:1722–1729
Modi HN, Suh SW, Song HR, Fernandez HM, Yang JH (2008) Treatment of neuromuscular scoliosis with posterior-only pedicle screw fixation. J Orthop Surg 3:23
Schoenfelder K, Cheng CL, Hsu LCS (1987) Pelvic obliquity in poliomyelitic scoliosis: correction of pelvic obliquity without fusion to the sacrum. Orthop Tran 32:240–333
Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK (2002) Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine 27:2072–2079
Shapio F, Sethna N (2004) Blood loss in pediatric spine surgery. Eur Spine J 13(Suppl 1):S6–S17
Sink EL, Newton PO, Mubarak SJ, Wenger DR (2003) Maintenance of sagittal plane alignment after surgical correction of spinal deformity in patients with cerebral palsy. Spine 28:1396–1403
Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB (1995) Segmental pedicle screw fixation in the treatment of adolescent idiopathic scoliosis. Spine 20:1399–1405
Sussman MD (1984) Advantage of early spinal stabilization and fusion in patients with Duchenne muscular dystrophy. J Pediatr Orthop 4:532–538
Whitacker C, Burton D, Asher M (2000) Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with pedicle screw anchorage. Spine 25:2312–2318
Wild A, Haak A, Kumar M (2001) Is sacral instrumentation mandatory neuromuscular thoracolumbar scoliosis due to myelomeningocele? Spine 26:E325–E329
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takaso, M., Nakazawa, T., Imura, T. et al. Segmental pedicle screws instrumentation and fusion to L5 for spinal deformity secondary to Duchenne muscular dystrophy: results with a minimum of 2 years follow-up. Eur J Orthop Surg Traumatol 20, 453–461 (2010). https://doi.org/10.1007/s00590-010-0589-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-010-0589-5