Abstract
Purpose
Although in recent years some randomized controlled trails (RCTs) have explored the analgesic effect of erector spinae plane block (ESPB) in spine surgery, their results are controversial. Our study aimed to examine the analgesic effect of preoperative ESPB in spine surgery by a meta-analysis of RCTs.
Methods
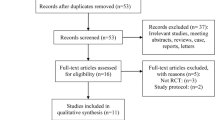
The articles of RCTs that compared preoperative ESPB with no block in terms of the analgesic effect in adult patients following spine surgery were eligible for inclusion. The primary outcome was the pain scores reported by Visual Analog Scale or Numerical Rating Scale of pain at different time intervals in 48 h after surgery. The secondary outcomes included postoperative opioid consumption, rescue analgesia requirement, opioid-related side effects and complications associated with ESPB.
Results
Twelve studies involving 828 patients were eligible for our study. Compared with no block, ESPB had a significant effect on reducing postoperative pain scores at rest and at movement at different time intervals except at movement at 48 h. ESPB significantly decreased opioid consumption in 24 h after surgery (SMD − 1.834; 95%CI − 2.752, − 0.915; p < 0.001; I2 = 89.0%), and reduced the incidence of rescue analgesia (RR 0.333; 95%CI 0.261, 0.425; p < 0.001; I2 = 0%) and postoperative nausea and vomiting (RR 0.380; 95%CI 0.272, 0.530; p < 0.001; I2 = 9.0%). Complications associated with ESPB were not reported in the included studies.
Conclusion
Our meta-analysis demonstrates that ESPB is effective in decreasing postoperative pain intensity and postoperative opioid consumption in spine surgery. Therefore, for the management of postoperative pain following spine surgery, preoperative ESPB is a good choice.








Similar content being viewed by others
Abbreviations
- RCTs:
-
Randomized controlled trails
- ESPB:
-
Erector spinae plane block
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PONV:
-
Postoperative nausea and vomiting
- MMA:
-
Multimodal analgesic
- VAS:
-
Visual analog scale
- NRS:
-
Numerical rating scale of pain
- SD:
-
Standard deviation
- SMDs:
-
Standardized mean differences
- WMDs:
-
Weighted mean differences
- CIs:
-
Confidence intervals
- RR:
-
Relative risk
- mTLIP:
-
Modified-thoracolumbar interfascial plane block
- MTP:
-
Mid-transverse process to pleura block
- RLB:
-
Retrolaminal block
- IF:
-
Incision infiltration
References
Hughey AB, Lesniak MS, Ansari SA, Roth S (2010) What will anesthesiologists be anesthetizing? trends in neurosurgical procedure usage. Anesth Analg 110(6):1686–1697. https://doi.org/10.1213/ANE.0b013e3181cbd9cc
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W (2013) Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 118(4):934–944. https://doi.org/10.1097/ALN.0b013e31828866b3
Bajwa SJ, Haldar R (2015) Pain management following spinal surgeries: an appraisal of the available options. Journal of craniovertebral junction & spine 6(3):105–110. https://doi.org/10.4103/0974-8237.161589
Dunn LK, Durieux ME, Nemergut EC (2016) Non-opioid analgesics: novel approaches to perioperative analgesia for major spine surgery. Best Pract Res Clin Anaesthesiol 30(1):79–89. https://doi.org/10.1016/j.bpa.2015.11.002
Perkins FM, Kehlet H (2000) Chronic pain as an outcome of surgery. A Review Predict Fact Anesthesiol 93(4):1123–1133. https://doi.org/10.1097/00000542-200010000-00038
Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10:2287–2298. https://doi.org/10.2147/jpr.s144066
Kurd MF, Kreitz T, Schroeder G, Vaccaro AR (2017) The role of multimodal analgesia in spine surgery. J Am Acad Orthop Surg 25(4):260–268. https://doi.org/10.5435/jaaos-d-16-00049
Mergeay M, Verster A, Van Aken D, Vercauteren M (2015) Regional versus general anesthesia for spine surgery. A comprehensive review Acta anaesthesiologica Belgica 66(1):1–9
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ (2016) The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med 41(5):621–627. https://doi.org/10.1097/aap.0000000000000451
Urits I, Charipova K, Gress K, Laughlin P, Orhurhu V, Kaye AD, Viswanath O (2019) Expanding role of the erector spinae plane block for postoperative and chronic pain management. Curr Pain Headache Rep 23(10):71. https://doi.org/10.1007/s11916-019-0812-y
Tulgar S, Aydin ME, Ahiskalioglu A, De Cassai A, Gurkan Y (2020) Anesthetic techniques: focus on lumbar erector spinae plane block. Local Reg Anesth 13:121–133. https://doi.org/10.2147/LRA.S233274
Chin KJ, Malhas L, Perlas A (2017) The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med 42(3):372–376. https://doi.org/10.1097/aap.0000000000000581
Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH, Kılıç CT (2018) Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: a randomized controlled study. J Clin Anesth 50:65–68. https://doi.org/10.1016/j.jclinane.2018.06.033
Ciftci B, Ekinci M, Celik EC, Tukac IC, Bayrak Y, Atalay YO (2020) Efficacy of an ultrasound-guided erector spinae plane block for postoperative analgesia management after video-assisted thoracic surgery: a prospective randomized study. J Cardiothorac Vasc Anesth 34(2):444–449. https://doi.org/10.1053/j.jvca.2019.04.026
Qiu Y, Zhang TJ, Hua Z (2020) Erector spinae plane block for lumbar spinal surgery: a systematic review. J Pain Res 13:1611–1619. https://doi.org/10.2147/jpr.s256205
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 343:d5928. https://doi.org/10.1136/bmj.d5928
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed) 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Wang W, Liu YL, Zhang YY (2018) Ultrasound-guided erector spine block as an adjuvant to general anesthesia and postoperative analgesia in patients undergoing lumbar spine surgery. J Clin Anesthesiol 34(12):1172–1175. https://doi.org/10.12089/jca.2018.12.007 (in Chinese)
Zhang XX (2018) Application of the Ultrasound-guided Erector Spinae Plane Block in Lumbar Spinal Surgery. Dissertation, North China University of Science and Technology. (in Chinese)
Yayik AM, Cesur S, Ozturk F, Ahiskalioglu A, Ay AN, Celik EC, Karaavci NC (2019) Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg 126:e779–e785. https://doi.org/10.1016/j.wneu.2019.02.149
Liu CF (2019) Effect of ultrasound-guided single erector spinae block for postoperative pain in lumbar spine surgery. Dissertation, Nanchang University (in Chinese)
Liu TZ, Hua L, Wan L (2019) Comparison of ultrasound-guided erector spinae plane block and retrolaminal block combined with general anesthesia for patients undergoing vertebral surgery. J Clin Anesthesiol 35(3):289–293. https://doi.org/10.12089/jca.2019.03.018 (in Chinese)
Wu X, Xue F, Wang J, Yang L, Chen XD, Yao SL (2019) Analgesic efficacy of ultrasound-guided bilateral erector spinae plane block in patients undergoing posterior lumbar interbody fusion. J Clin Anesthesiol 35(9):842–845. https://doi.org/10.12089/jca.2019.09.002 (in Chinese)
Ciftci B, Ekinci M, Celik EC, Yayik AM, Aydin ME, Ahiskalioglu A (2020) Ultrasound-guided erector spinae plane block versus modified-thoracolumbar interfascial plane block for lumbar discectomy surgery: a randomized. World Neurosurgery, Controlled Study. https://doi.org/10.1016/j.wneu.2020.09.077
Eskin MB, Ceylan A, Özhan MÖ, Atik B (2020) Ultrasound-guided erector spinae block versus mid-transverse process to pleura block for postoperative analgesia in lumbar spinal surgery. Anaesthesist 69(10):742–750. https://doi.org/10.1007/s00101-020-00848-w
Singh S, Choudhary NK, Lalin D, Verma VK (2020) Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol 32(4):330–334. https://doi.org/10.1097/ana.0000000000000603
Liu XM, Fu JN, Li J (2020) Postoperative analgesia effect of bilateral erector spinae plane block combined with intravenous analgesia in patients undergoing spinal surgery. People’s Military Surg 63(09):889–892 (in Chinese)
Peng C (2020) Effects of ultrasound-guided erector spinae plane block on analgesia and immune function in posterior lumbar surgery in elderly patients. Dissertation, Nanchang university. (in Chinese)
Zhang XQ (2020) Analgesic effect of erector spinae muscle block after posterior lumbar spine surgery. Dissertation, Xinjiang medical university. (in Chinese)
Yang HM, Choi YJ, Kwon HJ, O J, Cho TH, Kim SH (2018) Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia 73(10):1244–1250. https://doi.org/10.1111/anae.14408
Celik M, Tulgar S, Ahiskalioglu A, Alper F (2019) Is high volume lumbar erector spinae plane block an alternative to transforaminal epidural injection? evaluation with MRI. Reg Anesth Pain Med. https://doi.org/10.1136/rapm-2019-100514
Greenhalgh K, Womack J, Marcangelo S (2019) Injectate spread in erector spinae plane block. Anaesthesia 74(1):126–127. https://doi.org/10.1111/anae.14523
Vidal E, Giménez H, Forero M, Fajardo M (2018) Erector spinae plane block: a cadaver study to determine its mechanism of action. Rev Esp Anestesiol Reanim 65(9):514–519. https://doi.org/10.1016/j.redar.2018.07.004
Yamak Altinpulluk E, García Simón D, Fajardo-Pérez M (2018) Erector spinae plane block for analgesia after lower segment caesarean section: case report. Rev Esp Anestesiol Reanim 65(5):284–286. https://doi.org/10.1016/j.redar.2017.11.006
Chin KJ, Adhikary S, Sarwani N, Forero M (2017) The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia 72(4):452–460. https://doi.org/10.1111/anae.13814
Hacibeyoglu G, Topal A, Arican S, Kilicaslan A, Tekin A, Uzun ST (2018) USG guided bilateral erector spinae plane block is an effective and safe postoperative analgesia method for living donor liver transplantation. J Clin Anesth 49:36–37. https://doi.org/10.1016/j.jclinane.2018.06.003
Tulgar S, Kapakli MS, Senturk O, Selvi O, Serifsoy TE, Ozer Z (2018) Evaluation of ultrasound-guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. J Clin Anesth 49:101–106. https://doi.org/10.1016/j.jclinane.2018.06.019
Hand WR, Taylor JM, Harvey NR, Epperson TI, Gunselman RJ, Bolin ED, Whiteley J (2015) Thoracolumbar interfascial plane (TLIP) block: a pilot study in volunteers. Can J Anaesth 62(11):1196–1200. https://doi.org/10.1007/s12630-015-0431-y
Ahiskalioglu A, Alici HA, Selvitopi K, Yayik AM (2017) Ultrasonography-guided modified thoracolumbar interfascial plane block: a new approach. Can J Anaesth 64(7):775–776. https://doi.org/10.1007/s12630-017-0851-y
Ahiskalioglu A, Yayik AM, Alici HA (2017) Ultrasound-guided lateral thoracolumbar interfascial plane (TLIP) block: description of new modified technique. J Clin Anesth 40:62. https://doi.org/10.1016/j.jclinane.2017.04.015
Costache I, de Neumann L, Ramnanan CJ, Goodwin SL, Pawa A, Abdallah FW, McCartney CJL (2017) The mid-point transverse process to pleura (MTP) block: a new end-point for thoracic paravertebral block. Anaesthesia 72(10):1230–1236. https://doi.org/10.1111/anae.14004
Voscopoulos C, Palaniappan D, Zeballos J, Ko H, Janfaza D, Vlassakov K (2013) The ultrasound-guided retrolaminar block. Can J Anaesth 60(9):888–895. https://doi.org/10.1007/s12630-013-9983-x
Funding
Our study did not receive funding.
Author information
Authors and Affiliations
Contributions
All authors participated in the formulation of the study design and search strategy. JM, YB and JW searched and selected articles. YW, YY and TZ were responsible for the data extraction. JM, YB, YBZ and YCZ carried out data analysis and drafted the manuscript. All authors contributed to the discussion part. All authors were responsible for the integrity and accuracy of the data and agreed to publish the final version of the article.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethics approval and consent to participate
Our study was based on previously published RCTs, and no new patients were enrolled, so informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, J., Bi, Y., Zhang, Y. et al. Erector spinae plane block for postoperative analgesia in spine surgery: a systematic review and meta-analysis. Eur Spine J 30, 3137–3149 (2021). https://doi.org/10.1007/s00586-021-06853-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06853-w