Abstract
Purpose
To elucidate the minimum clinically important change (MCIC) of the physical component summary (PCS) of the Short Form-12, Oswestry Disability Index (ODI), EuroQOL-5 dimensions (EQ-5D), and the Core Outcome Measures Index (COMI) in patients aged ≥ 75 years undergoing lumbar spine surgery.
Methods
We retrospectively reviewed patients aged ≥ 75 years with degenerative lumbar spine disease who underwent lumbar spine decompression or fusion surgery within three levels between April 2017 and June 2018. We also evaluated patients aged < 75 years in the same period as reference. We evaluated the baseline and postoperative PCS, ODI, EQ-5D, and COMI scores. Patients were asked to answer an anchor question regarding health transition for MCICs using the anchor-based method.
Results
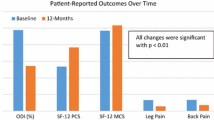
A total of 247 patients aged ≥ 75 years and 398 patients aged < 75 years were included for analysis. Of patients aged ≥ 75 years, 83.4% showed at least “somewhat improved” outcomes, while 91.0% of patients aged < 75 years reported this outcome. PCS change score was not adequately correlated to health transition in patients aged ≥ 75 years. Receiver operating characteristic curve analyses revealed MCICs of 17.8 for ODI, 0.18 for EQ-5D, and 1.6 for COMI in patients aged ≥ 75 years, and 12.7 for ODI, 0.19 for EQ-5D, and 2.3 for COMI in patients aged < 75 years.
Conclusion
In patients aged ≥ 75 years, PCS may not be feasible for evaluation of health transition. The MCIC value for ODI score was higher and that for EQ-5D/COMI score was lower in patients aged ≥ 75 years, compared with those in patients aged < 75 years.

Similar content being viewed by others
References
Fekete TF, Loibl M, Jeszenszky D, Haschtmann D, Banczerowski P, Kleinstuck FS, Becker HJ, Porchet F, Mannion AF (2018) How does patient-rated outcome change over time following the surgical treatment of degenerative disorders of the thoracolumbar spine? Eur Spine J 27:700–708. https://doi.org/10.1007/s00586-017-5358-2
Szpalski M, Gunzburg R, Mélot C, Aebi M (2003) The aging of the population: a growing concern for spine care in the twenty-first century. Eur Spine J 12(2):S81-83
World health organization (WHO) (2003) Regional office for the western pacific. Ageing and Health: A Health Promotion Approach for Developing Countries.
Parker SL, Adogwa O, Mendenhall SK, Shau DN, Anderson WN, Cheng JS, Devin CJ, McGirt MJ (2012) Determination of minimum clinically important difference (MCID) in pain, disability, and quality of life after revision fusion for symptomatic pseudoarthrosis. Spine J 12:1122–1128. https://doi.org/10.1016/j.spinee.2012.10.006
Fukuhara S, Suzumoto Y (2004) Manual of the SF-12 Japanese version, (in Japanese). Kyoto Institute for Health Outcomes and Process Evaluation Research, pp. 7-145
Ware JE Jr (2000) SF-36 Health survey update. Spine Phila Pa 25:3130–3139
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine Phila Pa 25:2940–2952. https://doi.org/10.1097/00007632-200011150-00017
Roland M, Fairbank J (2000) The Roland-Morris disability questionnaire and the Oswestry disability questionnaire. Spine (Phila Pa) 25:3115–3124. https://doi.org/10.1097/00007632-200012150-00006
EuroQo LGE (1990) A new facility for the measurement of health-related quality of life. Health Policy 16:199–208. https://doi.org/10.1016/0168-8510(90)90421-9
Tsuchiya A, Ikeda S, Ikegami N, Nishimura S, Sakai I, Fukuda T, Hamashima C, Hisashige A, Tamura M (2002) Estimating an EQ-5D population value set: the case of Japan. Health Econ 11:341–353. https://doi.org/10.1002/hec.673
Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective. Part 1: the Core Outcome Measures Index in clinical practice. Eur Spine J 183:367–373. https://doi.org/10.1007/s00586-009-0942-8
Kato S, Oshima Y, Matsubayashi Y, Taniguchi Y, Tanaka S, Takeshita K (2019) Minimum clinically important difference in outcome scores among patients undergoing cervical laminoplasty. Eur Spine J 28:1234–1241. https://doi.org/10.1007/s00586-019-05945-y
Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7:541–546. https://doi.org/10.1016/j.spinee.2007.01.008
de Vet HC, Terwee C (2010) The minimal detectable change should not replace the minimal important difference. J Clin Epidemiol 63:804–805
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14:598–604. https://doi.org/10.3171/2010.12.SPINE10472
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry disability Index, medical outcomes study questionnaire short form 36, and pain scales. Spine J 8:968–974. https://doi.org/10.1016/j.spinee.2007.11.006
Nagata K, Oshima Y, Nakamoto H, Sakamoto R, Ohtomo N, Izuka M, Nakajima K, Yoshimoto T, Fujii T, Matsudaira K, Tanaka S, Oka H (2019) Validity of the Japanese Core Outcome Measures Index (COMI)-Back for thoracic and lumbar spine surgery: a prospective cohort study. Eur Spine J. https://doi.org/10.1007/s00586-019-06249-x
Ames CP, Smith JS, Pellise F, Kelly MP, Gum JL, Alanay A, Acaroglu E, Perez-Grueso FJS, Kleinstuck FS, Obeid I, Vila-Casademunt A, Burton DC, Lafage V, Schwab FJ, Shaffrey CI, Bess S, Serra-Burriel M, European Spine Study Group ISSG (2019) Development of deployable predictive models for minimal clinically important difference achievement across the commonly used health-related quality of life instruments in adult spinal deformity surgery. Spine (Phila Pa) 44:1144-1153. doi: https://doi.org/10.1097/BRS.0000000000003031
Yoshizawa K, Kobayashi H, Fujie M, Ogawa Y, Yajima T, Kawai K (2016) Estimation of minimal clinically important change of the Japanese version of EQ-5D in patients with chronic noncancer pain: a retrospective research using real-world data. Health Qual Life Outcomes. https://doi.org/10.1186/s12955-016-0438-2
Hashimoto H, Komagata M, Nakai O, Morishita M, Tokuhashi Y, Sano S, Nohara Y, Okajima Y (2006) Discriminative validity and responsiveness of the Oswestry disability index among Japanese outpatients with lumbar conditions. Eur Spine J 15:1645–1650
Jansson KA, Nemeth G, Granath F, Jönsson B, Blomqvist P (2009) Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. J Bone Joint Surg Br 91:210–216. https://doi.org/10.1302/0301-620X.91B2.21119
Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD (1999) Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care 37:469–478. https://doi.org/10.1097/00005650-199905000-00006
Wyrwich KW, Tierney WM, Wolinsky FD (1999) Further evidence supporting an SEM-based criterion for identifying meaningful intra-individual changes in health-related quality of life. J Clin Epidemiol 52:861–873. https://doi.org/10.1016/s0895-4356(99)00071-2
Ware JE, Kosinski M, Keller SK (1994) SF-36 physical and mental health summaries scales: a user’s manual. The Health Institute, Boston, MA
Fritz JM, Irrgang JJ (2001) A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther 81:776–788. https://doi.org/10.1093/ptj/81.2.776
Janssen MF, Birnie E, Haagsma JA, Bonsel GJ (2008) Comparing the standard EQ-5D three-level system with a five-level version. Value Health 11:275–284. https://doi.org/10.1111/j.1524-4733.2007.00230.x
Turner D, Schünemann HJ, Griffith LE, Beaton DE, Griffiths AM, Critch JN, Guyatt GH (2010) The minimal detectable change cannot reliably replace the minimal important difference. J Clin Epidemiol 63:28–36. https://doi.org/10.1016/j.jclinepi.2009.01.024
Kobayashi K, Ando K, Nishida Y, Ishiguro N, Imagama S (2018) Epidemiological trends in spine surgery over 10 years in a multicenter database. Eur Spine J 27:1698–1703. https://doi.org/10.1007/s00586-018-5513-4
Liao J-C, Chiu P-Y, Chen W-J, Chen L-H, Niu C-C (2016) Surgical outcomes after instrumented lumbar surgery in patients of eighty years of age and older. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-016-1239-9
https://www8.cao.go.jp/kourei/whitepaper/w-2017/html/zenbun/index.html [database online] (2017).
Asher AL, Kerezoudis P, Mummaneni PV, Bisson EF, Glassman SD, Foley KT, Slotkin JR, Potts EA, Shaffrey ME, Shaffrey CI, Coric D, Knightly JJ, Park P, Fu KM, Devin CJ, Archer KR, Chotai S, Chan AK, Virk MS, Bydon M (2018) Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the Quality Outcomes Database. Neurosurg Focus 44:E2. https://doi.org/10.3171/2017.10.FOCUS17554
Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective: part 2. Minimal clinically important difference for improvement and deterioration as measured with the Core Outcome Measures Index. Eur Spine J 18:374–379. https://doi.org/10.1007/s00586-009-0931-y
Tonosu J, Takeshita K, Hara N, Matsudaira K, Kato S, Masuda K, Chikuda H (2012) The normative score and the cut-off value of the Oswestry disability index (ODI). Eur Spine J 21:1596–1602. https://doi.org/10.1007/s00586-012-2173-7
Hung M, Saltzman CL, Kendall R, Bounsanga J, Voss MW, Lawrence B, Spiker R, Brodke D (2018) What Are the MCIDs for PROMIS, NDI, and ODI instruments among patients with spinal conditions? Clin Orthop Relat Res 476:2027–2036. https://doi.org/10.1097/CORR.0000000000000419
Kulkarni AV (2006) Distribution-based and anchor-based approaches provided different interpretability estimates for the hydrocephalus outcome questionnaire. J Clin Epidemiol 59:176–184
van der Roer N, Ostelo RW, Bekkering GE (2006) Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine (Phila Pa) 31:578
Funding
No funds were received in support of this work.
Author information
Authors and Affiliations
Contributions
KN and YO contributed to the conception and design of the study and the acquisition and interpretation of the data, and critically revised the drafted manuscript for important intellectual content. HN and SK contributed to the analysis of the data and critically revised the drafted manuscript for important intellectual content. KM, HO, and ST made substantial contributions to the conception of the study and drafted the manuscript. YT, NK, TO, AH, MF, SA, and NH contributed to the data registration and critically revised the drafted manuscript. All authors approved the final version of the manuscript to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. The manuscript submitted does not contain information about medical device (s)/drug (s).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (institutional review board of the Clinical Research Support Center of the University of Tokyo Hospital, Yokohama Rosai Hospital, Japanese Red Cross Medical Center, Japan Community Health-care Organization Tokyo Shinjuku Medical Center, Kanto Rosai Hospital, Toranomon Hospital, Saitama Red Cross Hospital, and Japanese Red Cross Musashino Hospital) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nagata, K., Nakamoto, H., Kato, S. et al. Minimum clinically important change for outcome scores among patients aged 75 or over undergoing lumbar spine surgery. Eur Spine J 30, 1226–1234 (2021). https://doi.org/10.1007/s00586-021-06815-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06815-2