Abstract
Purpose
Stand-alone zero-profile devices have already proven safety, and a reduced dysphagia rate was assumed. So far, no level-one evidence is available to prove the proposed advantages of zero-profile implants in multilevel procedures. The aim of this RCT was to compare the clinical and radiological outcome of a zero-profile spacer versus cage + plate in two-level ACDF.
Methods
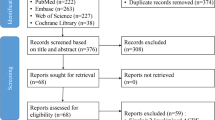
Consecutive patients with contiguous two-level cDD were randomly assigned either to the interventional group (zero-profile device) or to the control group (cage + plate). Primary endpoint of the study was the prevalence of dysphagia at 24 months. Disability, progress of adjacent segment degeneration, fusion status and loss of correction were analyzed as secondary outcome measure. Primary outcome parameter was statistically analyzed by Chi-square test.
Results
Forty-one patients met inclusion criteria and were randomly assigned to the interventional and the control group. Dysphagia was frequent in either group at 3 months FU favoring interventional group (p = 0.078). At final FU, less patients of the interventional group complained about dysphagia, but the difference was not significant. No relevant differences at final FU were recorded for NPDI, loss of correction and adjacent-level degeneration. Fusion rate was slightly lower in the interventional group.
Discussion
Two-level ACDF either by a stand-alone zero-profile spacer or cage + plate is safe. Using a zero-profile cage dysphagia was infrequent at 24 months, but the value did not reach statistical significance in comparison with the cage + plate. Hence, this randomized trial was not able to prove the proposed clinical superiority for dysphagia rates for zero-profile anchored spacer in two-level cDD.






Similar content being viewed by others
References
Matz PG, Holly LT, Mummaneni PV et al (2009) Anterior cervical surgery for the treatment of cervical degenerative myelopathy. J Neurosurg Spine 11:170–173. https://doi.org/10.3171/2009.3.spine08724
Matz PG, Holly LT, Groff MW et al (2009) Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine 11:174–182. https://doi.org/10.3171/2009.3.spine08720
Kim SW, Limson MA, Kim S-B et al (2009) Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J 18:218–231. https://doi.org/10.1007/s00586-008-0854-z
Korinth MC (2008) Treatment of cervical degenerative disc disease—current status and trends. Zentralbl Neurochir 69:113–124. https://doi.org/10.1055/s-2008-1081201
Scholz M, Schleicher P, Pabst S, Kandziora F (2015) A zero-profile anchored spacer in multilevel cervical anterior interbody fusion: biomechanical comparison to established fixation techniques. Spine 40:E375–E380. https://doi.org/10.1097/brs.0000000000000768
Song K-J, Taghavi CE, Lee K-B et al (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine 34:2886–2892. https://doi.org/10.1097/brs.0b013e3181b64f2c
Nambiar M, Phan K, Cunningham JE et al (2017) Locking stand-alone cages versus anterior plate constructs in single-level fusion for degenerative cervical disease: a systematic review and meta-analysis. Eur Spine J 26:2258–2266. https://doi.org/10.1007/s00586-017-5015-9
Fraser JF, Hartl R (2007) Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine 6:298–303. https://doi.org/10.3171/spi.2007.6.4.2
Scholz M, Reyes PM, Schleicher P et al (2009) A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine 34:156–160. https://doi.org/10.1097/brs.0b013e31818ff9c4
Kim HJ, Kelly MP, Ely CG et al (2012) The risk of adjacent-level ossification development after surgery in the cervical spine. Spine 37:S65–S74. https://doi.org/10.1097/brs.0b013e31826cb8f5
Yang J-Y, Song H-S, Lee M et al (2009) Adjacent level ossification development after anterior cervical fusion without plate fixation. Spine 34:30–33
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458. https://doi.org/10.1097/01.brs.0000031407.52778.4b
Riley LH, Skolasky RL, Albert TJ et al (2005) Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine 30:2564–2569
Kasimatis GB, Panagiotopoulos E, Gliatis J et al (2009) Complications of anterior surgery in cervical spine trauma: an overview. Clin Neurol Neurosurg 111:18–27. https://doi.org/10.1016/j.clineuro.2008.07.009
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on Dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Techn 18:406–409
Cagli S, Isik HS, Zileli M (2009) Cervical screw missing secondary to delayed esophageal fistula: case report. Turk Neurosurg 19:437–440
Gazzeri R, Tamorri M, Faiola A, Gazzeri G (2008) Delayed migration of a screw into the gastrointestinal tract after anterior cervical spine plating. Spine 33:E268–E271. https://doi.org/10.1097/brs.0b013e31816b8831
McAfee PC, Cappuccino A, Cunningham BW et al (2010) Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Techn 23:1–8. https://doi.org/10.1097/bsd.0b013e31819e2ab8
Schleicher P, Gerlach R, Schär B et al (2008) Biomechanical comparison of two different concepts for stand alone anterior lumbar interbody fusion. Eur Spine J 17:1757–1765. https://doi.org/10.1007/s00586-008-0797-4
Scholz M, Schnake KJ, Pingel A et al (2010) A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res 469:666–673. https://doi.org/10.1007/s11999-010-1597-9
Xiao S, Liang Z, Wei W, Ning J (2017) Zero-profile anchored cage reduces risk of postoperative dysphagia compared with cage with plate fixation after anterior cervical discectomy and fusion. Eur Spine J 26:975–984. https://doi.org/10.1007/s00586-016-4914-5
Yun D-J, Lee S-J, Park S-J et al (2017) Use of a zero-profile device for contiguous 2-level anterior cervical diskectomy and fusion: comparison with cage with plate construct. World Neurosurg 97:189–198. https://doi.org/10.1016/j.wneu.2016.09.065
Liu Y, Wang H, Li X et al (2016) Comparison of a zero-profile anchored spacer (ROI-C) and the polyetheretherketone (PEEK) cages with an anterior plate in anterior cervical discectomy and fusion for multilevel cervical spondylotic myelopathy. Eur Spine J 25:1881–1890. https://doi.org/10.1007/s00586-016-4500-x
Scholz M, Pingel A, Schleicher P, Kandziora F (2014) A cervical “zero-profile” cage with integrated angle-stable fixation: 24-months results. Acta Orthop Belg 80:558–566
Pitzen TR, Chrobok J, Stulik J et al (2009) Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: two-year results of a multi-centric, randomized, controlled study. Spine 34:641–646. https://doi.org/10.1097/brs.0b013e318198ce10
Faldini C, Pagkrati S, Leonetti D et al (2010) Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin Orthop Relat Res 469:674–681. https://doi.org/10.1007/s11999-010-1614-z
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502. https://doi.org/10.1136/ard.16.4.494
Gerszten PC, Paschel E, Mashaly H et al (2016) Outcomes evaluation of zero-profile devices compared to stand-alone PEEK cages for the treatment of three- and four-level cervical disc disease. Cureus 8:e775. https://doi.org/10.7759/cureus.775
Vaccaro AR, Falatyn SP, Scuderi GJ et al (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11:410–415
He S, Feng H, Lan Z et al (2017) A randomized trial comparing clinical outcomes between zero-profile and traditional multi-level anterior cervical discectomy and fusion surgery for cervical myelopathy. Spine. https://doi.org/10.1097/brs.0000000000002323
Rihn JA, Kane J, Albert TJ et al (2010) What is the incidence and severity of dysphagia after anterior cervical surgery? Clin Orthop Relat Res 469:658–665. https://doi.org/10.1007/s11999-010-1731-8
Fountas KN, Kapsalaki EZ, Nikolakakos LG et al (2007) Anterior cervical discectomy and fusion associated complications. Spine 32:2310–2317. https://doi.org/10.1097/brs.0b013e318154c57e
Findlay C, Ayis S, Demetriades AK (2018) Total disc replacement versus anterior cervical discectomy and fusion: a systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes. Bone Joint J 100-B:991–1001. https://doi.org/10.1302/0301-620x.100b8.bjj-2018-0120.r1
Anderson PA, Nassr A, Currier BL et al (2017) Evaluation of adverse events in total disc replacement: a meta-analysis of FDA summary of safety and effectiveness data. Global Spine J 7:76S–83S. https://doi.org/10.1177/2192568216688195
Chin KR, Eiszner JR, Adams SB Jr (2007) Role of plate thickness as a cause of dysphagia after anterior cervical. Spine 32:2585–2590. https://doi.org/10.1097/brs.0b013e318158dec8
Yin M, Ma J, Huang Q et al (2016) The new Zero-P implant can effectively reduce the risk of postoperative dysphagia and complications compared with the traditional anterior cage and plate: a systematic review and meta-analysis. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-016-1274-6
Duan Y, Yang Y, Wang Y et al (2016) Comparison of anterior cervical discectomy and fusion with the zero-profile device versus plate and cage in treating cervical degenerative disc disease: a meta-analysis. J Clin Neurosci 33:11–18. https://doi.org/10.1016/j.jocn.2016.01.046
Nemoto O, Kitada A, Naitou S et al (2015) Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol 25(Suppl 1):S127–S134. https://doi.org/10.1007/s00590-014-1547-4
Lee D-H, Lee J-S, Yi J-S et al (2013) Anterior cervical plating technique to prevent adjacent-level ossification development. Spine J 13:823–829. https://doi.org/10.1016/j.spinee.2013.03.009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors M.S. and F.K. have received consulting and speakers honorarium for company Depuy Synthes. The other authors declare no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scholz, M., Onal, B., Schleicher, P. et al. Two-level ACDF with a zero-profile stand-alone spacer compared to conventional plating: a prospective randomized single-center study. Eur Spine J 29, 2814–2822 (2020). https://doi.org/10.1007/s00586-020-06454-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06454-z