Abstract
Purpose
The aim of this study was to evaluate the prevalence and risk factors for postoperative pulmonary complications (PPC) after posterior instrumentation and fusion (PIF) in patients with non-degenerative scoliosis.
Methods
We retrospectively evaluated 703 patients (224 males, 479 females) diagnosed with non-degenerative scoliosis who underwent PIF in our center from January 2010 to January 2018. Preoperative, perioperative, demographic data, surgical methods and radiographic parameters were extracted and analyzed to identify risk factors for PPC.
Results
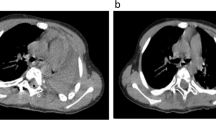
The mean age of the patients was 20.8 ± 9.0 years with the following diagnoses: congenital scoliosis (287/703, 40.8%), idiopathic scoliosis (281/703, 40.0%), neuromuscular scoliosis (103/703, 14.7%) and syndromic scoliosis (32/703, 4.5%). PPC manifested in 82 patients (11.7%) including pleural effusion (39/82, 47.6%), pneumonia (33/82, 40.2%), pneumothorax (3/82, 3.7%), respiratory failure (3/82, 3.7%), hemothorax (2/82, 2.4%), pulmonary edema (1/82, 1.2%) and pulmonary embolism (1/82, 1.2%). Multifactorial regression analysis confirmed that revision surgery [odds ratio (OR) = 2.320, P = 0.030], preoperative respiratory disease (OR = 14.286, P < 0.001), preoperative Cobb angle of main curve > 75° (OR = 1.701, P = 0.046) and thoracoplasty (OR = 4.098 P < 0.001) were risk factors for PPC after PIF in patients with non-degenerative scoliosis.
Conclusions
A prevalence of 11.7% PPC was observed after PIF. Risk factors were preoperative Cobb angle of main curve > 75°, preoperative respiratory disease, revision surgery and thoracoplasty. Surgeons should recognize and pay attention to these risk factors and take appropriate preventive measures to prevent severe pulmonary complications.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
References
Liang J, Qiu G, Shen J et al (2010) Predictive factors of postoperative pulmonary complications in scoliotic patients with moderate or severe pulmonary dysfunction. J Spinal Disord Tech 23(6):388–392
Greggi T, Bakaloudis G, Fusaro I et al (2010) Pulmonary function after thoracoplasty in the surgical treatment of adolescent idiopathic scoliosis. J Spinal Disord Tech 23(8):e63–e69
Reames DL, Smith JS, Fu KM et al (2011) Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976) 36(18):1484–1491
Fu KM, Smith JS, Polly DW et al (2011) Morbidity and mortality associated with spinal surgery in children: a review of the Scoliosis Research Society morbidity and mortality database. J Neurosurg Pediatr 7(1):37–41
Sansur CA, Smith JS, Coe JD et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine (Phila Pa 1976) 36(9):E593–E597
Seo HJ, Kim HJ, Ro YJ, Yang HS (2013) Non-neurologic complications following surgery for scoliosis. Korean J Anesthesiol 64(1):40–46
Lao L, Weng X, Qiu G, Shen J (2013) The role of preoperative pulmonary function tests in the surgical treatment of extremely severe scoliosis. J Orthop Surg Res 8:32
De la Garza Ramos R, Goodwin CR, Abu-Bonsrah N et al (2016) Patient and operative factors associated with complications following adolescent idiopathic scoliosis surgery: an analysis of 36,335 patients from the nationwide Inpatient Sample. J Neurosurg Pediatr 25(6):730–736
Taniguchi Y, Oichi T, Ohya J et al (2018) In-hospital mortality and morbidity of pediatric scoliosis surgery in Japan: analysis using a national inpatient database. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000010277
Levy BJ, Schulz JF, Fornari ED, Wollowick AL (2015) Complications associated with surgical repair of syndromic scoliosis. Scoliosis 10:14
Bendon AA, George KA, Patel D (2016) Perioperative complications and outcomes in children with cerebral palsy undergoing scoliosis surgery. Paediatr Anaesth 26(10):970–975
Kang GR, Suh SW, Lee IO (2011) Preoperative predictors of postoperative pulmonary complications in neuromuscular scoliosis. J Orthop Sci 16(2):139–147
Vedantam R, Lenke LG, Bridwell KH et al (2000) A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine (Phila Pa 1976) 25(1):82–90
Yaszay B, Jazayeri R, Lonner B (2009) The effect of surgical approaches on pulmonary function in adolescent idiopathic scoliosis. J Spinal Disord Tech 22(4):278–283
Bjure J, Grimby G, Kasalický J et al (1970) Respiratory impairment and airway closure in patients with untreated idiopathic scoliosis. Thorax 25(4):451–456
Xue X, Shen J, Zhang J et al (2015) An analysis of thoracic cage deformities and pulmonary function tests in congenital scoliosis. Eur Spine J 24(7):1415–1421
Fu J, Liu C, Zhang YG et al (2015) Three-dimensional computed tomography for assessing lung morphology in adolescent idiopathic scoliosis following posterior spinal fusion surgery. Orthop Surg 7(1):43–49
Shi Z, Wu Y, Huang J et al (2013) Pulmonary function after thoracoplasty and posterior correction for thoracic scoliosis patients. Int J Surg 11(9):1007–1009
Gitelman Y, Lenke LG, Bridwell KH et al (2011) Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure: a 10-year follow-up analysis. Spine (Phila Pa 1976) 36(20):1665–1672
Toll BJ, Samdani AF, Janjua MB et al (2018) Perioperative complications and risk factors in neuromuscular scoliosis surgery. J Neurosurg Pediatr 22(2):207–213
Han K, Wang Y, Cui S, Xu C, Su P (2018) Successful surgery for a neuromuscular scoliosis patient by pulmonary rehabilitation with forced vital capacity below 30. Eur Spine J 27(9):2072–2075
Hicks JM, Singla A, Shen FH, Arlet V (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 35(11):465–470
Liang W, Yu B, Wang Y et al (2016) Pleural effusion in spinal deformity correction surgery—a report of 28 cases in a single center. PLoS ONE. https://doi.org/10.1371/journal.pone.0154964
Jain A, Marks MC, Kelly MP et al (2018) Cost-utility analysis of operative vs. nonoperative treatment of thoracic AIS. Spine. https://doi.org/10.1097/BRS.0000000000002936 (Epub ahead of print)
Acknowledgements
The authors gratefully acknowledge the support from Beijing Chaoyang Hospital affiliated to China Capital Medical University. The author also thanks Dr. Yong Hai who supervised the study, provided technique support and corrected some mistakes.
Funding
This study has not received any fund support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Y., Hai, Y., Liu, Y. et al. Risk factors for postoperative pulmonary complications in the treatment of non-degenerative scoliosis by posterior instrumentation and fusion. Eur Spine J 28, 1356–1362 (2019). https://doi.org/10.1007/s00586-019-05968-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05968-5