Abstract
Purpose
Primary vascular bone tumors of the spine represent a challenge for oncology surgeons, due to the need of planning a surgical strategy appropriate to the tumor behavior. But these tumors represent a challenge also for pathologists, as immunohistochemical and molecular analyses have recently refined the terminology.
Methods
A cohort of 81 cases was retrospectively reviewed, targeting the evolution of diagnoses and the treatment-related outcome. Sixty-six cases (including one case originally diagnosed as chordoma) were diagnosed before 2011, and 15 were diagnosed and treated in the period 2011–2017. Fully documented outcome studies are available for 46 patients whose immunohistochemical and molecular analyses were available. The follow-up ranges from 6 months of the early patient death to 300 months of the longest disease-free survival.
Results
The outcome was related not only to the treatment performed, but also to the evolution of diagnoses. The term Hemangioendothelioma that defined a benign aggressive (Enneking stage 3) tumor is now obsolete and replaced by the diagnosis of Epithelioid Hemangioma for benign aggressive tumor and Epithelioid Hemangioendothelioma for low-grade malignant tumor. En bloc resection was appropriate for local control, but 2 out of 7 cases of epithelioid Hemangioendotheliomas died due to the spread of the disease None of the Hemangiomas recurred after intralesional excision with or without radiotherapy, or after vertebroplasty. Both cases of Angiosarcoma had a fast and lethal evolution.
Conclusions
Surgeons must be aware of the evolution of terminology to decide the most appropriate treatment options.
Graphical abstract
These slides can be retrieved from Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary vascular bone tumors appear as lytic lesions, sometimes multiple, that should be differentiated radiologically by metastatic carcinoma or multiple myeloma. These tumors represent a challenge for pathologists: Most vascular neoplasms originating in the bone show an epithelioid morphology and can express epithelial markers such as keratin, being possibly misdiagnosed as metastatic carcinoma. Moreover, recent advances by new diagnostic tools like immunohistochemistry and molecular analyses did contribute to a deeper knowledge of these neoplasms, with new terminology and a more detailed classification [1,2,3]. As a consequence, primary vascular tumors of bone represent a serious diagnostic and therapeutic pitfall for oncology surgeons. The anatomical constraints of the spine combined with the difficult assessment of tumor biological behavior increase the complexity of decision-making process in spinal localizations. These tumors range from indisputably benign lesions like Hemangiomas to high-grade malignant tumors like Angiosarcomas, including intermediate conditions, whose features and terminology have changed over time due to the evolution of diagnostic tools, from morphology to immunohistochemical and molecular analyses.
Surgeons must be aware of this evolution of terminology not just to decide the most appropriate treatment options, but also for critical appraisal of the evolution of cases treated in the past, based on a diagnosis which changed at retrospective immunohistochemical/molecular revision [4, 5].
The purpose of this article is to remark the evolution of diagnostic techniques and classification from the 1990s [6] to nowadays [7]. This will allow the understanding of the biological behavior of the single entities as actually defined, and the evaluation of the middle- and long-term outcomes of primary vascular bone tumors of the spine related to the treatment was performed, in order to plan the most appropriate surgical solution.
Materials and methods
A cohort of 81 cases was retrospectively reviewed. These cases were observed and treated from 1990 to 2017 by the same surgical team, and all specimens were evaluated and stored in the same Bone Tumor Center. Dossier, radiographic images and histology were reviewed and discussed by the senior surgeon (SB) and by the pathologists (AR, ADT). The study was approved by the Ethical Committee of Rizzoli Institute of Bologna (protocol number CE22814 of December 15, 2016, Bologna).
In the years 1990 to 2011, the terminology of bone vascular tumors included: Hemangioma, Hemangioendothelioma and Angiosarcoma. Hemangioma is a frankly benign tumor, mostly asymptomatic and incidentally found (Enneking Stage 1, latent) [8].
Treatment is always palliative, limited to the rare symptomatic cases, targeted to relieve symptoms like pain, pathologic fracture, neurological symptoms produced by encroachment of the canal (Fig. 1).
A 34-year-old female: sudden occurrence of incomplete tetraplegia at the 6th month of pregnancy. No previous symptoms. a, b MRI shows a huge mass invading the spinal canal. c CT scan shows the typical polka dot pattern pathognomonic of Hemangioma. CT guide biopsy confirmed the histological diagnosis of Hemangioma. The patient was monitored under corticoid treatment until delivery was possible. Laminectomy and fixation followed selective arterial embolization. Radiotherapy was later given. d Two-year follow-up. No evidence of progression; neurological functions are recovered
Angiosarcoma is defined as a high-grade malignant tumor (Enneking Stage II, mostly B as extracompartmental) [8].
The term Hemangioendothelioma was used to identify all the intermediate conditions, staged as Enneking Stage 3 benign aggressive, extracompartmental [8], able to metastasize in few cases (as in some Giant Cell Tumors of bone). As a peculiar feature of vascular tumors, both the possibility of multicentric occurrence with the same morphological findings, and also the progression of histological malignancy in local recurrences have been accepted [6].
In 65 cases treated over the years 1990 to 2011, the old terminology included: 45 Hemangiomas, 18 Hemangioendotheliomas and 2 Angiosarcomas.
Since 2011, after the publication of specific genetic changes and the definitions of Epithelioid Hemangioma, Pseudomyogenic Hemangioendothelioma and Epithelioid Hemangioendothelioma [1, 3, 9,10,11], a new classification was proposed including Hemangioma, with the same histological and clinical pattern, Epithelioid Hemangioma (Fig. 2) as a benign aggressive condition, Epithelioid Hemangioendothelioma (Figs. 3, 4, 5), as a low-grade malignancy and Angiosarcoma, as a high-grade malignant tumor. Pseudomyogenic and Retiform Hemangioendothelioma are soft tissue tumors, in very rare cases arising in bone [2, 12]. A retrospective review was decided of the 65 cases of primary bone vascular tumors of the spine diagnosed before 2011 using the immunohistochemical and molecular analyses not available before.
A 58-year-old male: a T11 lytic lesion, intracompartmental, diagnosed by transpedicular biopsy as Hemangioendothelioma in March 2001. Staged as intermediate, Enneking benign aggressive, St.3. b Submitted to en bloc resection. Margins were defined as wide/marginal. c He is still under regular yearly clinical and radiographic follow-up (16 years). Here is the sagittal CT scan reconstruction showing bone ingrowth inside the carbon fiber cage at 12 years. The histological revision of the specimen changed the diagnosis to Epithelioid Hemangioma
A 44-year-old male: a, b lytic intracompartmental lesion of the body of L4, diagnosed by TC-guided trocar biopsy chordoma. It was staged as St.IA (low-grade malignant, intracompartmental). The radiologist even remarked that the adjacent sclerotic region could have been interpreted as the benign notochordal tumor, sometimes observed adjacent to a chordoma. c In August 2005, he was submitted to en bloc resection whose margins were reported as tumor-free. d Seven years later, a neoplastic lesion was resected en bloc from the left trapezius muscle. It was diagnosed as Epithelioid Hemangioendothelioma with the aspect of malignancy. The critical revision of the L4 lesion, submitted to immunohistochemical studies, confirmed the same diagnosis in the previous vertebral localization. Due to the violation of the margins (tumor found at the surface of the specimen in one small are), he was also submitted to radiotherapy. e Sagittal CT reconstruction showing bone ingrowth inside the carbon fiber cage, without any evidence of tumor recurrence. He is free from any local and systemic disease at 149 months from the L4 en bloc resection, at 74 months from the muscle metastasis
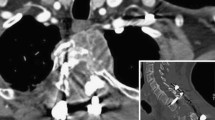
An example of a case of Epithelioid Hemangioendothelioma (arising in L4) including cords, strands and nests of epithelioid cells in a myxohyaline stroma on hematoxylin and eosin (a ×200 of magnification) associated with a strong nuclear reactivity for CAMTA1 antibody (b ×200 of magnification). A second example of Epithelioid Hemangioendothelioma (arising in T12) that showed mature vessel lumen formation, in addition to intracytoplasmic vacuoles on hematoxylin and eosin (c ×200 of magnification) associated with a strong nuclear reactivity for TFE3 antibody (d ×200 of magnification). TFE3 and CAMTA1 markers are specific of Epithelioid Hemangioendothelioma and are mutually exclusive
A 59-year-old female: a, b lytic, extracompartmental L1 tumor, expanding to L2. TC-guided trocar biopsy allowed the diagnosis of Hemangioendothelioma, Enneking St. 3. c In February 2000, she was submitted to en bloc resection. The margins were reported as tumor-free. d Sagittal CT scan reconstruction 16 years after the en bloc resection. No evidence of local disease, bone ingrowth inside the carbon fiber cage. Previously, 10 and 12 years after the diagnosis, erosive lesions were found, respectively, in the left olecranon and at the acromion: submitted to intralesional extracapsular excision and cement filling of the residual cavity. The pathologist diagnosed the metastasis as Epithelioid Hemangioendothelioma with the aspect of malignancy. The revision of the L1L2 tumor found the same elements, and the primary diagnosis was changed from Hemangioendothelioma to Epithelioid Hemangioendothelioma with the aspect of malignancy. She had other bone metastases and died due to lung disease on January 2017
Due to the limited quality of the tissue (very old tissue paraffin blocks, poor fixation or decalcification of the tumoral sample), the immunohistochemical and/or molecular analyses was feasible on 33 out of these 65 cases.
The revision allowed these diagnoses: Hemangioma (20), Epithelioid Hemangioma (4), Epithelioid Hemangioendothelioma (3), Pseudomyogenic Hemangioendothelioma (1), Angiosarcoma (2).
A tumor of L4, submitted to en bloc resection in August 2005 and diagnosed as chordoma at that time, recurred in the trapezius muscle 8 years later (Fig. 3). The specimen of the soft tissue en bloc resection was diagnosed as Epithelioid Hemangioendothelioma based on morphology, immunohistochemical and molecular features. The revision of the primary tumor, using immunohistochemical and molecular studies (not available 8 years before), allowed the diagnostic change (Fig. 4a, b), thus increasing the number of Epithelioid Hemangioendotheliomas to 4 cases.
The cohort also includes 15 bone vascular tumors of the spine observed from 2011 to 2017 and diagnosed according to the new classification. The final number of cases submitted to fully immunohistochemical and molecular studies and is available for outcome evaluation ranges to 46 (Fig. 6), including 26 Hemangiomas, 8 Epithelioid Hemangiomas, 7 Epithelioid Hemangioendotheliomas, 2 Pseudomyogenic Hemangioendotheliomas, 1 Retiform Hemangioendothelioma, 2 Angiosarcomas.
Analysis of the 81 cases discussed in the text, observed and treated by the same team in the years 1990 to 2017. The cohort includes 65 cases of spine tumors diagnosed as bone vascular tumors in the years 1990 to 2011, plus 1 case diagnosed as Chordoma which was at the revision changed to Epithelioid Hemangioendothelioma. Fifteen cases of bone vascular tumors were diagnosed according to the new terminology and treated in the years 2011 to 2017. Thirty-four out of the 66 were available for revision, ending in 31 confirmed diagnoses of bone vascular tumors, as 3 cases had different diagnoses. The final number of confirmed bone vascular tumors of the spine is therefore 46
Results
None of the 18 cases of Hemangioma on which immunohistochemical and molecular revision was performed received a different diagnosis. Their number raised up to 20 due to 2 cases previously diagnosed as Hemangioendothelioma.
The 2 cases of Angiosarcoma were confirmed as high-grade malignant tumor with epithelioid features.
The tumoral sample was adequate for molecular and immunohistochemical analysis in 13 of the 18 tumors originally diagnosed as Hemangioendothelioma. These 13 tumors received a broad spectrum of different diagnoses among vascular bone tumors: Hemangioma (2), Epithelioid Hemangioma (4), Epithelioid Hemangioendothelioma (3), Pseudomyogenic Hemangioendothelioma (1). Further, three cases received the diagnoses of Solitary Fibrous Tumor, Myoepithelioma, Sclerosing Epithelioid Fibrosarcoma.
A case of Chordoma submitted to en bloc resection in 2005 was later diagnosed as Epithelioid Hemangioendothelioma (Figs. 3 and 4a, b).
To summarize, after the morphological, immunohistochemical and molecular revision of bone vascular tumor with an available material diagnosed between 1990 and 2011, 31 out of 33 cases were confirmed as vascular tumors with these diagnoses: 20 Hemangiomas, 4 Epithelioid Hemangiomas, 4 Epithelioid Hemangioendothelioma, 1 Pseudomyogenic Hemangioendothelioma and 2 Angiosarcoma.
In the following years, till 2017, 15 new cases were observed, bringing up the number of primary bone vascular tumors of the spine confirmed by immunohistochemical and molecular studies to 46 (Fig. 6).
Twenty-six cases of Hemangiomas were treated by radiation therapy alone (5), palliative surgery (decompression and/or fixation) combined with radiotherapy (18), vertebroplasty (3). Hemangioma is a benign tumor, relatively frequent in the spine as an incidental finding. Treatment is provided when it becomes symptomatic because of vertebral body collapse or of the neurological symptoms given by epidural mass or of local pain resistant to pain killers. Indeed, these symptoms frequently and suddenly occur during pregnancy (Fig. 1), or at the pubertal spurt. The histological pattern of these symptomatic cases is identical to the latent ones.
Vertebroplasty was performed in cases of local pain, surgical decompression in case of canal impingement and fixation in case of pathologic fracture. No local recurrence was observed at the final follow-up, ranging from 6 to 300 months (average 99.7 months).
Epithelioid Hemangiomas (8 cases): Three were submitted to en bloc resection with a diagnosis at the time of Hemangioendothelioma and do not present any local or systemic disease at 48, 96, 205 months of follow-up (Fig. 2). Three cases were submitted to intralesional excision combined with radiotherapy and had a similar course at 12, 20 and 58 months. Two more cases were submitted to simple embolization (underestimating the different behaviors between Hemangioma and Epithelioid Hemangioma): one is stable at 12 months, and the other is slowly progressing at 8 months.
A clinical and radiological follow-up is available for all the seven Epithelioid Hemangioendotheliomas. Four were submitted to en bloc resection without any other adjuvant treatments, according to the diagnosis of Hemangioendothelioma: one died after 6 months, another after 204 months with bone and lung metastases (Fig. 5), while the two survivors are free of disease at 18 and at 160 months (Figs. 3 and 4a: this second case had soft tissue distant metastasis 7 years after the vertebrectomy performed on the histological diagnosis of Chordoma on CT-guided trocar biopsy and is now free of disease 74 months after soft tissue en bloc resection and radiotherapy, as margins were violated). One case evolved to radio-induced Sarcoma 52 months after intralesional excision and radiotherapy. Two cases are free from local and systemic disease 2 and 4 years after gross total intralesional excision and radiotherapy.
Morphologically, two of these cases of Epithelioid Hemangioendothelioma (the one who died after 204 months and the one who was first misdiagnosed as Chordoma) showed malignant features (nuclear pleomorphism, necrosis and high mitotic activity). The presence of TFE3 gene rearrangements, typical of Epithelioid Hemangioendothelioma, excluded the diagnosis of Angiosarcoma (Fig. 4c, d).
The course of the 2 cases of Angiosarcoma, both with epithelioid morphology features, was fast and lethal. Both cases were so huge at the clinical onset to make en bloc resection impossible. Intralesional excision was combined with radiotherapy and chemotherapy. Both patients died after 4 and 12 months with local progression and lung metastases.
The cohort also includes 2 cases of Pseudomyogenic Hemangioendothelioma (one of them first diagnosed as Hemangioendothelioma) and one case of Retiform Hemangioendothelioma. All of them were submitted to gross total excision and radiotherapy and are alive without any sign of local or systemic disease at 12, 55, 73 months of follow-up.
Seven en bloc resections were performed: 3 in Epithelioid Hemangioma that succeeded to achieve local and systemic control. The 4 en bloc resections performed in tumors which resulted to be Epithelioid Hemangioendothelioma always achieved local control, but were unable to prevent metastases in 3 cases and the course was lethal in 2 cases.
Discussion
Primary vascular bone tumors are rare and difficult to diagnose. The symptoms are specific and the radiological findings not conclusive: They are lytic and sometimes multicentric in the skeleton-like metastases or myeloma. Furthermore, surgeons can be misled in the decision-making process by the recent studies based on immunohistochemical and molecular analyses. The new classification of bone vascular tumors as proposed in 2013 is supported by the rapid elucidation of novel, characteristic translocations in the different entities [2]. In the last 4 years, there have been further several important refinements in the classification of vascular neoplasms of bone, including the description of vascular tumor types previous reported only in soft tissues such as Pseudomyogenic Hemangioendothelioma and Retiform Hemangioendothelioma, along with the identification of novel and recurrent molecular genetic findings, broadening the spectrum of available ancillary tests for the pathologist [1, 2, 7, 9,10,11,12,13].
The term Hemangioendothelioma is now obsolete: It is replaced by a broad spectrum of different vascular tumor entities, with relative therapeutic recommendations. This is particularly relevant in the spine: These tumors are highly vascular, possibly life-threatening in intralesional surgery [4, 5]. Conversely, en bloc resection is highly demanding and morbid due to the infiltrative pattern of the more aggressive bone vascular tumors, with the possible need of relevant anatomical structures sacrifice to achieve appropriate oncological margins [14, 15].
A retrospective change of diagnosis after revision of the specimens by immunohistochemical and molecular studies also generates possible misleading at follow-up and creates communication problems with the patients.
In our review, all cases previously diagnosed as Hemangioma did not change at the immunohistochemical and molecular revision, as well as the two cases of Angiosarcomas.
Functional surgery, to treat pain, pathological fracture and/or encroachment of the content of the canal, remains the recommended treatment for Hemangioma. This corresponds to Enneking indication [8] for St.1 lesions. In the literature, some cases of Hemangiomas treated by en bloc resection are reported [16]. This option looks like an overtreatment in light of the outcome reported in this review (no local recurrence out of 26 confirmed cases treated by palliative surgery, vertebroplasty and/or radiation), unless some of the reported cases submitted to en bloc resection be indeed Epithelioid Hemangioma.
Angiosarcoma is confirmed to be a high malignant tumor (St.II, almost always found as B, extracompartmental): The Enneking appropriate indication [8] is the chemotherapy associated with en bloc resection (wide margin) when feasible with acceptable morbidity. However, few protocols of chemotherapy have been proposed [17], and the effects of neoadjuvant chemotherapy are not as relevant as in Osteosarcoma or Ewing sarcoma [18]. Tumor-free margin en bloc resection is seldom feasible due to the fast infiltrative behavior. Few successful cases are reported [19].
In this perspective, medical oncology and radiation oncology progresses could be helpful. Multidisciplinary approach is mandatory, and surgery should be planned according to the timing of chemotherapy and allowing the most effective radiation by the use of radiolucent hardware [21].
The entity previously diagnosed as Hemangioendothelioma does not exist anymore. Out of 13 cases which could be revised (on the 18 cases observed between 1990 and 2011), 4 were diagnosed as Epithelioid Hemangioma, 3 as Epithelioid Hemangioendothelioma, 1 as Pseudomyogenic Hemangioendothelioma, 2 as Hemangioma and finally 3 cases were even not diagnosed as vascular tumors but, respectively, as Solitary Fibrous Tumor, Myoepithelioma, Sclerosing Epithelioid Fibrosarcoma.
The long-term outcome study confirmed that en bloc resection with tumor-free margin is appropriate for Epithelioid Hemangioma. This is acceptable even from the perspective of the Enneking staging system [8] as Epithelioid Hemangioma is defined as benign aggressive tumor (Enneking St.3).
Epithelioid Hemangioendothelioma has a more aggressive behavior, and it is now considered as a low-grade malignant tumor which could be staged as Enneking Stage I. Enneking appropriate surgery [8] is therefore marginal/wide en bloc resection.
In our study, we reported 3 cases of confirmed Epithelioid Hemangioendothelioma out of four submitted to en bloc resection that developed bone, soft tissues and lung metastases, and two died (one after 6 months, the other 204 months after surgery). Other 3 cases were submitted to intralesional excision and radiation: 2 are living without evidence of disease at 2 years; the other developed a radio-induced sarcoma after 52 months. This experience helps to identify Epithelioid Hemangioendothelioma as a condition of which is wary, as occurred in other experiences [20]. If feasible, a tumor-free margin en bloc resection seems to be the best local treatment [5]. When the criteria to perform a tumor-free margin en bloc resection are not fulfilled [14], the combination of surgery and radiotherapy is a reasonable option. In these cases, the use of composite PEEK/carbon fiber implants [21] is helpful to allow early detection of local recurrence and to allow better radiotherapy planning due to the implant radiolucency, which is able to prevent any scattering effect and over irradiation of neighboring structures. As a consequence, the doses on the target can be higher.
A careful follow-up should be set up for early surgical, radiation and/or chemotherapic treatment of possible bone and soft tissue metastases.
In conclusion, spine oncology surgeons must be confident with the terminology actually accepted by pathologists, where the integration of morphology, immunohistochemical and molecular features allows better stratification of primary epithelioid vascular tumors of bone.
To allow pathologists to achieve a circumstantial diagnosis, biopsy must always be performed, best by trocar under CT scan control, aiming at reaching the most representative tumoral tissue.
As a final remark, due to the evolution of terminology here discussed, the interpretation of the outcome data reported in the literature results is difficult and possibly misleading if the diagnosis is not supported by the actually required studies.
Change history
26 August 2019
Unfortunately, the affiliation for the following authors was incorrectly published in the original publication.
References
Antonescu CR, Le Loarer F, Mosquera J-M, Sboner A, Zhang L, Chen C-L, Chen H-W, Pathan N, Krausz T, Dickson BC, Weinreb I, Rubin MA, Hameed M, Fletcher CDM (2013) Novel YAP1-TFE3 fusion defines a distinct subset of epithelioid hemangioendothelioma. Gene Chromosome Cancer 52:775–784
Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F (eds) (2013) World Health Organization Classification of Tumours. Pathology and genetics of tumours of soft tissue and bone. IARC Press, Lyon, pp 153–154
Errani C, Zhang L, Sung YS, Hajdu M, Singer S, Maki RG, Healey JH, Antonescu CR (2011) A novel WWTR1-CAMTA1 gene fusion is a consistent abnormality in epithelioid hemangioendothelioma of different anatomic sites. Genes Chromosomes Cancer 50:644–653
Marks DS, Thomas AMC, Thompson AG, Mills S (1995) Surgical management of haemangioendothelioma of the spine. Eur Spine J 4:186–190
Luzzati A, Gagliano F, Perrucchini G, Scotto G, Zoccali C (2014) Epithelioid hemangioendothelioma of the spine: results at seven years of average follow-up in a series of 10 cases surgically treated and a review of literature. Eur Spine J 24(10):2156–2164
Campanacci M, Boriani S, Giunti A (1980) Hemangioendothelioma of bone. Cancer 46(4):804–814
van IJzendoorn DGP, Bovée JVMG (2017) Vascular tumors of bone: the evolvement of a classification based on molecular developments. Surg Pathol Clin 10(3):621–635
Enneking W, Spainer SS, Goodman MA (1980) A system for the surgical staging of muscoloskeletal sarcomas. Clin Orthop 153:106–120
van IJzendoorn DG, de Jong D, Romagosa C, Picci P, Benassi MS, Gambarotti M, Daugaard S, van de Sande M, Szuhai K, Bovée JV (2015) Fusion events lead to truncation of FOS in epithelioid hemangioma of bone. Genes Chromosomes Cancer 54(9):565–574
Walther C, Tayebwa J, Lilljebjörn H, Magnusson L, Nilsson J, von Steyern FV, Øra I, Domanski HA, Fioretos T, Nord KH, Fletcher CD, Mertens F (2014) A novel SERPINE1-FOSB fusion gene results in transcriptional up-regulation of FOSB in pseudomyogenic haemangioendothelioma. J Pathol 232(5):534–540
Righi A, Gambarotti M, Picci P, Dei Tos AP, Vanel D (2015) Primary pseudomyogenic haemangioendothelioma of bone: report of two cases. Skelet Radiol 44(5):727–731
Inyang A, Mertens F, Puls F, Sumathi V, Inwards C, Folpe A, Lee CH, Zhang Y, Symmans P, Rubin B, Nielsen GP, Nguyen VH, Rosenberg AE (2016) Primary pseudomyogenic hemangioendothelioma of bone. Am J Surg Pathol 40(5):587–598
Antonescu CR (2014) Malignant vascular tumors: an update. Mod Pathol 27(Suppl 1):S30–S38
Boriani S, Bandiera S, Colangeli S, Ghermandi R, Gasbarrini A (2014) En bloc resection of primary tumors of the thoracic spine: indications, planning, morbidity. Neurol Res 36:566–576
Luzzati AD, Shah S, Gagliano F, Perrucchini G, Scotto G, Alloisio M (2014) Multilevel en bloc spondylectomy for tumors of the thoracic and lumbar spine is challenging but rewarding. Clin Orthop Relat Res 473(3):858–867
Goldstein CL, Varga PP, Gokaslan ZL, Boriani S, Luzzati A, Rhines L et al (2015) Spinal hemangiomas. Spine 40(9):656–664
Asmane I, Litique V, Heymann S, Marcellin L, Métivier AC, Duclos B, Bergerat JP, Kurtz JE (2008) Adriamycin, cisplatin, ifosfamide and paclitaxel combination as front-line chemotherapy for locally advanced and metastatic angiosarcoma. Analysis of three case reports and review of the literature. Anticancer Res 28(5B):3041–3045
Pülhorn H, Elliot T, Clark J, Gonzalvo A (2017) Case report: angiosarcoma of the cervical spine. J Clin Neurosci 45:129–131
Kawashima H, Ishikawa S, Fukase M, Ogose A, Hotta T (2004) Successful surgical treatment of angiosarcoma of the spine: a case report. Spine (Phila Pa 1976) 29(13):E280–E283
Albakr A, Schell M, Drew B, Cenic A (2017) Epithelioid hemangioendothelioma of the spine: case report and review of the literature. J Spine Surg 3(2):250–259
Boriani S, Tedesco G, Ming L, Ghermandi R, Amichetti M, Fossati P et al (2018) Carbon-fiber-reinforced PEEK fixation system in the treatment of spine tumors: a preliminary report. Eur Spine J 27(4):874–881
Acknowledgements
AA is indebted to Carlo Piovani for his excellent activity as imaging archivist and for data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Boriani, S., Cecchinato, R., Righi, A. et al. Primary vascular bone tumors in the spine: a challenge for pathologists and spine oncology surgeons. Eur Spine J 28, 1502–1511 (2019). https://doi.org/10.1007/s00586-019-05930-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05930-5