Abstract
Purpose
To evaluate changes in pulmonary function tests (PFT) at 5 years post-operatively in patients with adolescent idiopathic scoliosis (AIS) and to determine whether these changes are progressive or static after 2 years.
Methods
AIS surgical patients with pre-operative and 5 year post-operative forced expiratory volume (FEV) and forced vital capacity (FVC) were included. The percentage of patients with pulmonary impairment at 5 years was calculated. Repeated measures ANOVA was used to evaluate changes between pre-operative PFT and 5 years post-operative PFT and to determine whether the changes differed between curve types and approach. A sub-analysis of patients with 2 year data was performed to determine whether PFT changes were static or progressive.
Results
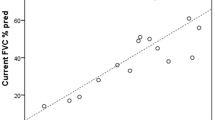
Two hundred and sixty-two patients had undergone pre-operative and 5 year post-operative PFTs. At 5 years, 42% were normal, 41% had mild impairment, and 17% had moderate-severe impairment. Overall, there was a decline in % predicted FVC (p < 0.05); FEV remained stable. There was no difference based on major curve type (p > 0.05). Anterior instrumentation cases declined significantly between pre-operative PFT and 5 years post-operative PFT (FEV: − 10% open, − 6% thoracoscopic; FVC: − 13% open, − 8% thoracoscopic) (p ≤ 0.02). The posterior cases remained stable (2% FEV, p = 0.7; − 0.6% FVC, p = 0.06). A subgroup of 90 patients with 2 year post-operative PFTs demonstrated that changes were progressive between 2 and 5 years post-operatively. The average change in FVC from 2 to 5 years was significantly different between the anterior open (− 9%) and posterior-only (0.7%) groups (p = 0.015).
Conclusion
In patients who underwent anterior instrumentation, PFTs declined from the pre-operative to the 5 years post-operative time point. There was a progressive decline of 4–10% beyond 2 years post-operatively. Patients who underwent posterior instrumentation remained stable.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.





Similar content being viewed by others
References
Aaro S, Ohlund C (1984) Scoliosis and pulmonary function. Spine 9:220–222
Kearon C, Viviani GR, Kirkley A, Killian KJ (1993) Factors determining pulmonary function in adolescent idiopathic thoracic scoliosis. Am Rev Respir Dis 148:288–294. https://doi.org/10.1164/ajrccm/148.2.288
Leong JC, Lu WW, Luk KD, Karlberg EM (1999) Kinematics of the chest cage and spine during breathing in healthy individuals and in patients with adolescent idiopathic scoliosis. Spine 24:1310–1315
Upadhyay SS, Mullaji AB, Luk KD, Leong JC (1995) Relation of spinal and thoracic cage deformities and their flexibilities with altered pulmonary functions in adolescent idiopathic scoliosis. Spine 20:2415–2420
Vedantam R, Crawford AH (1997) The role of preoperative pulmonary function tests in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion. Spine 22:2731–2734
Vedantam R, Lenke LG, Bridwell KH, Haas J, Linville DA (2000) A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine 25:82–90
Weinstein SL, Zavala DC, Ponseti IV (1981) Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am 63:702–712
Wood KB, Schendel MJ, Dekutoski MB, Boachie-Adjei O, Heithoff KH (1996) Thoracic volume changes in scoliosis surgery. Spine 21:718–723
Gagnon S, Jodoin A, Martin R (1989) Pulmonary function test study and after spinal fusion in young idiopathic scoliosis. Spine 14:486–490
Kim YJ, Lenke LG, Bridwell KH, Cheh G, Sides B, Whorton J (2008) Prospective pulmonary function comparison of anterior spinal fusion in adolescent idiopathic scoliosis: thoracotomy versus thoracoabdominal approach. Spine 33:1055–1060. https://doi.org/10.1097/brs.0b013e31816fc3a5
Lee AC, Feger MA, Singla A, Abel MF (2016) Effect of surgical approach on pulmonary function in adolescent idiopathic scoliosis patients: a systemic review and meta-analysis. Spine 41:E1343–E1355. https://doi.org/10.1097/brs.0000000000001619
Lenke LG, Newton PO, Marks MC, Blanke KM, Sides B, Kim YJ, Bridwell KH (2004) Prospective pulmonary function comparison of open versus endoscopic anterior fusion combined with posterior fusion in adolescent idiopathic scoliosis. Spine 29:2055–2060
Newton PO, Perry A, Bastrom TP, Lenke LG, Betz RR, Clements D, D’Andrea L (2007) Predictors of change in postoperative pulmonary function in adolescent idiopathic scoliosis: a prospective study of 254 patients. Spine 32:1875–1882. https://doi.org/10.1097/brs.0b013e31811eab09
Wang X, Dockery DW, Wypij D, Gold DR, Speizer FE, Ware JH, Ferris BG Jr (1993) Pulmonary function growth velocity in children 6 to 18 years of age. Am Rev Respir Dis 148:1502–1508. https://doi.org/10.1164/ajrccm/148.6_Pt_1.1502
Chen SH, Huang TJ, Lee YY, Hsu RW (2002) Pulmonary function after thoracoplasty in adolescent idiopathic scoliosis. Clin Orthop Relat Res 399:152–161
Graham EJ, Lenke LG, Lowe TG, Betz RR, Bridwell KH, Kong Y, Blanke K (2000) Prospective pulmonary function evaluation following open thoracotomy for anterior spinal fusion in adolescent idiopathic scoliosis. Spine 25:2319–2325
Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K (2005) Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am 87:1534–1541. https://doi.org/10.2106/JBJS.C.00978
Kinnear WJ, Kinnear GC, Watson L, Webb JK, Johnston ID (1992) Pulmonary function after spinal surgery for idiopathic scoliosis. Spine 17:708–713
Kumano K, Tsuyama N (1982) Pulmonary function before and after surgical correction of scoliosis. J Bone Joint Surg Am 64:242–248
Lenke LG, Bridwell KH, Blanke K, Baldus C (1995) Analysis of pulmonary function and chest cage dimension changes after thoracoplasty in idiopathic scoliosis. Spine 20:1343–1350
Newton PO, Faro FD, Gollogly S, Betz RR, Lenke LG, Lowe TG (2005) Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis. A study of six hundred and thirty-one patients. J Bone Joint Surg Am 87:1937–1946. https://doi.org/10.2106/JBJS.D.02209
Redding G, Song K, Inscore S, Effmann E, Campbell R (2008) Lung function asymmetry in children with congenital and infantile scoliosis. Spine J 8:639–644. https://doi.org/10.1016/j.spinee.2007.04.020
Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, Jeszenszky D, Beele B (1999) Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine 24:225–239
Tis JE, O’Brien MF, Newton PO, Lenke LG, Clements DH, Harms J, Betz RR (2010) Adolescent idiopathic scoliosis treated with open instrumented anterior spinal fusion: five-year follow-up. Spine 35:64–70. https://doi.org/10.1097/BRS.0b013e3181c4af52
Gitelman Y, Lenke LG, Bridwell KH, Auerbach JD, Sides BA (2011) Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure: a 10-year follow-up analysis. Spine 36:1665–1672. https://doi.org/10.1097/BRS.0b013e31821bcf4c
Sudo H, Ito M, Kaneda K, Shono Y, Takahata M, Abumi K (2013) Long-term outcomes of anterior spinal fusion for treating thoracic adolescent idiopathic scoliosis curves: average 15-year follow-up analysis. Spine 38:819–826. https://doi.org/10.1097/BRS.0b013e31827ddc60
Murray J, Nadel J (2000) Textbook of respiratory medicine. Saunders, Philadelphia
Yaszay B, Bastrom TP, Bartley CE, Parent S, Newton PO (2017) The effects of the three-dimensional deformity of adolescent idiopathic scoliosis on pulmonary function. Eur Spine J 26:1658–1664. https://doi.org/10.1007/s00586-016-4694-y
Udupa JK, Tong Y, Capraro A, McDonough JM, Mayer OH, Ho S, Wileyto P, Torigian DA, Campbell RM Jr (2018) Understanding respiratory restrictions as a function of the scoliotic spinal curve in thoracic insufficiency syndrome: a 4D dynamic MR imaging study. J Pediatr Orthop 10:15–20. https://doi.org/10.1097/bpo.0000000000001258
Acknowledgements
This study was supported in part by grants to the Setting Scoliosis Straight Foundation in support of Harms Study Group research from DePuy Synthes Spine, EOS imaging, K2M, Medtronic, NuVasive and Zimmer Biomet. Harms Study Group Investigators: Aaron Buckland, MD; New York University Amer Samdani, MD; Shriners Hospitals for Children—Philadelphia Amit Jain, MD; Johns Hopkins Hospital Baron Lonner, MD; Mount Sinai Hospital Benjamin Roye, MD; Columbia University Burt Yaszay, MD; Rady Children’s Hospital Chris Reilly, MD; BC Children’s Hospital Daniel Hedequist, MD; Boston Children’s Hospital Daniel Sucato, MD; Texas Scottish Rite Hospital David Clements, MD; Cooper Bone & Joint Institute New Jersey Firoz Miyanji, MD; BC Children’s Hospital Harry Shufflebarger, MD; Nicklaus Children's Hospital Jack Flynn, MD; Children’s Hospital of Philadelphia Jahangir Asghar, MD; Cantor Spine Institute Jean Marc Mac Thiong, MD; CHU Sainte-Justine Joshua Pahys, MD; Shriners Hospitals for Children—Philadelphia Juergen Harms, MD; Klinikum Karlsbad-Langensteinbach, Karlsbad Keith Bachmann, MD; University of Virginia Larry Lenke, MD; Columbia University Mark Abel, MD; University of Virginia Michael Glotzbecker, MD; Boston Children’s Hospital Michael Kelly, MD; Washington University Michael Vitale, MD; Columbia University Michelle Marks, PT, MA; Setting Scoliosis Straight Foundation Munish Gupta, MD; Washington University Nicholas Fletcher, MD; Emory University Patrick Cahill, MD; Children’s Hospital of Philadelphia Paul Sponseller, MD; Johns Hopkins Hospital Peter Gabos, MD: Nemours/Alfred I. duPont Hospital for Children Peter Newton, MD; Rady Children’s Hospital Peter Sturm, MD; Cincinnati Children’s Hospital Randal Betz, MD; Institute for Spine & Scoliosis Ron Lehman, MD; Columbia University Stefan Parent, MD: CHU Sainte-Justine Stephen George, MD; Nicklaus Children's Hospital Steven Hwang, MD; Shriners Hospitals for Children—Philadelphia Suken Shah, MD; Nemours/Alfred I. duPont Hospital for Children Tom Errico, MD; Nicklaus Children's Hospital Vidyadhar Upasani, MD; Rady Children’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors report grants to their institutions from the Setting Scoliosis Straight Foundation during the conduct of this study. The following conflicts of interest exist outside of the submitted work: Dr. Yaszay received grants and personal fees from K2M, grants and personal fees from DePuy Synthes Spine, personal fees from Nuvasive, personal fees from Medtronic, personal fees from Orthopediatrics, personal fees from Stryker, personal fees from Globus, grants from Setting Scoliosis Straight Foundation, and has a patent with K2M with royalties paid. Dr. Lonner reports received grants from Setting Scoliosis Straight Foundation, personal fees from DePuy Synthes Spine, personal fees from K2M, personal fees from Paradigm Spine, personal fees from Spine Search, personal fees from Ethicon, non-financial support from Spine Deformity Journal, grants from John and Marcella Fox Fund Grant, grants from OREF, personal fees from Zimmer Biomet, and personal fees from Apifix. Dr. Betz received personal fees and other from Abyrx, other from Advanced Vertebral Solutions, personal fees and other from ApiFix, personal fees from DePuy Synthes Spine, other from Electrocore, personal fees from Globus Medical, other from Medovex, personal fees from Medtronic, other from MiMedx, other from Orthobond, personal fees and other from SpineGuard, other from SpineMedica, personal fees from Thieme Medical Publishers, personal fees from Zimmer Biomet, and has an immediate family member who is an employee of DePuy Synthes Spine. Dr. Shah received personal fees from DePuy Synthes Spine and K2M. Dr. Asghar received personal fees and non-financial support from Omega innovative Technologies, and personal fees from Life Spine and Globus Medical. Dr. Samdani received personal fees from DePuy Synthes Spine, personal fees from Ethicon, personal fees from Globus Medical, personal fees from Misonix, personal fees from Stryker, personal fees from Zimmer Biomet, other from Setting Scoliosis Straight Foundation, other from Scoliosis Research Society, and other from Children's Spine Study Group. Dr. Newton received grants and other from Setting Scoliosis Straight Foundation, other from Rady Children's Specialists, grants, personal fees and non-financial support from DePuy Synthes Spine, grants and other from SRS, grants from EOS imaging, personal fees from Thieme Publishing, grants from NuVasive, other from Electrocore, personal fees from Cubist, other from International Pediatric Orthopedic Think Tank, grants, non-financial support and other from Orthopediatrics, grants, personal fees and non-financial support from K2M, grants and non-financial support from Alphatech, and has the following patents: Anchoring systems and methods for correcting spinal deformities (8540754) with royalties paid to DePuy Synthes Spine, a patent Low profile spinal tethering systems (8123749) licensed to DePuy Spine, Inc., a patent Screw placement guide (7981117) licensed to DePuy Spine, Inc., a patent Compressor for use in minimally invasive surgery (7189244) licensed to DePuy Spine, Inc., and a patent Posterior spinal fixation pending to K2M.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yaszay, B., Jankowski, P.P., Bastrom, T.P. et al. Progressive decline in pulmonary function 5 years post-operatively in patients who underwent anterior instrumentation for surgical correction of adolescent idiopathic scoliosis. Eur Spine J 28, 1322–1330 (2019). https://doi.org/10.1007/s00586-019-05923-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05923-4