Abstract
Purpose
To investigate whether pre-operative magnetic resonance imaging (MRI) of the lumbar multifidus muscle (LMM) would predict clinical outcomes following lumbar spinal decompression for symptomatic spinal stenosis.
Methods
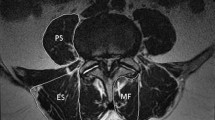
A prospective cohort of patients with symptomatic neurogenic claudication, documented spinal stenosis on pre-operative MRI underwent spinal decompression. All subjects completed standardised outcome measures (Core Outcome Measures Index (COMI), Oswestry Disability Index (ODI v2.1) pre-operatively, 1 and 2 years post-surgery. Surgery was performed using a standardised lumbar spinous process osteotomy for access, followed by a decompression of the central canal, lateral recess and foraminal zones as indicated by the pre-operative MRI. Lumbar MRI scans were evaluated by two independent observers who assessed the axial CSA of the LMM bilaterally and the degree of muscle atrophy according to the Kader classification (2000). Changes in COMI and ODI scores at 1 and 2 years were investigated for statistically significant correlations with CSA of LMM and Kader grading. Statistical analyses utilised Student’s t test, kappa coefficient for inter-observer agreement and Bland–Altman Limits of Agreement (BALOA).
Results
66 patients (41 female) aged between 29 and 86 years underwent single-level decompression in 44, two-level decompression in 16 and three-level decompression in 6 cases. No significant correlation was observed between improvements in ODI and COMI relative to age, degree of stenosis, posterior fat thickness or psoas CSA. Those subjects with the greatest LMM atrophy relative to psoas CSA and L5 vertebral body area on pre-operative MRI had the least absolute improvement in both ODI and COMI scores (p = 0.006).
Conclusions
Reduced LMM CSA (<8.5 cm2) and muscle atrophy were associated with less favourable outcomes following lumbar spinal decompression. Pre-operative CSA of LMM appeared to be a more reliable predictor of post-operative clinical outcomes compared to the Kader Grading Score. This is the first study to investigate the prognostic value of pre-operative MRI appearance and CSA of LMM with respect to post-operative outcome following lumbar decompression surgery. Healthy pre-operative LMM is associated with better outcomes following lumbar spinal decompression.






Similar content being viewed by others
References
Sobottke R, Aghayey E, Roder C, Eysel P, Delank SK, Zweig T (2013) Predictors of surgical, general and follow-up complications in lumbar spinal; relative to patient age as emerged from the Spine Tango Registry. Eur Spine J 21:411–417
Tomkins-Lane CC, Melloh M, Lurie J, Smuck M, Freeman BJC, Samartzis D, Hu R, Barz T, Stuber K, Schneider M, Haig A, Schizas C, Cheung J, Mannion AF, Staub L, Comer C, Macedo L, Ahn S, Takahashi K, Sandella D (2016) International Society for the Study of the Lumbar Spine (ISSLS) prize winner: consensus on the clinical diagnosis of lumbar spinal stenosis: results of an International Delphi Study. Spine (Phila Pa 1976) 41(15):1239–1246
Anjarwalla N, Brown L, McGregor A (2007) The outcome of spinal decompression surgery 5 years on. Eur Spine J 16:1842–1847
Aalto TJ, Malmivaara A, Kovacs F et al (2006) Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine J 31(18):E648–E663
Kader DF, Wardlaw D, Smith FW (2000) Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol 55(2):145–149
Macintosh J, Valencia F, Bogduk N et al (1986) The morphology of the human lumbar multifidus. Clin Biomech 1(4):196–204
Wilke HJ, Wolf S, Claes LE et al (1995) Stability increase of the lumbar spine with different muscle groups: A biomechanical in vitro study. Spine J. 20(2):192–197
Panjabi MM (1992) The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Dis 5:390–397
Ward SR, Kim CK, Eng CM et al (2009) Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J Bone Joint Surg Am 91:176–185
Hides J, Stanton W, Mendis D et al (2011) The relationship of transversus abdominus and lumbar multifidus clinical muscle tests in patients with chronic lower back pain. Man Ther 16(6):573–577
Hides JA, Lambrecht G, Stanton WR, Damann V (2016) Changes in multifidus and abdominal muscle size in response to microgravity: possible implications for low back pain research. Eur Spine J 25(Suppl 1):S175–S182
Kääriäinen T, Leinonen V, Taimela S et al (2013) Lumbar paraspinal and biceps brachii muscle function and movement perception in lumbar spinal stenosis. Eur Spine J 22(4):788–793
Hides JA, Richardson CA, Jull GA (1996) Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine J. 21(23):2763–2769
Lee H, Song J, Lee H et al (2011) Association between cross-sectional areas of lumbar muscles on magnetic resonance imaging and chronicity of low back pain. Ann Rehabil Med 35(6):852–859
Ali I, Ulbricht C, McGregor AH (2011) Degeneration of the extensor muscle group in a surgical low back and leg pain population. J Back Musculoskelet Rehabil 24:23–30
Kim DY, Lee SH, Chung SK (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine J 30(1):123–129
Ghiasi M, Arjman N, Shirazi-Adl A et al (2016) Cross-sectional area of human trunk paraspinal muscles before and after posterior lumbar surgery using magnetic resonance imaging. Eur Spine J 25(3):774–782
Motosuneya T, Asazuma R, Tsuji T et al (2006) Postoperative change of the cross-sectional area of back musculature after 5 surgical procedures as assessed by magnetic resonance imaging. J Spin Dis Tech 19(5):318–322
Airaksinen O, Herno E, Kaukanen T et al (1996) Density of lumbar muscles 4 years after decompressive spinal surgery. Eur Spine J 5(3):193–197
Gille O, Jolivet E, Dousset V (2007) Erector spinae muscle changes on magnetic resonance imaging following lumbar surgery through a posterior approach. Spine. 32(11):1236–1241
Chen YY, Pao JL, Liaw CK et al (2014) Image changes of paraspinal muscles and clinical correlations in patients with unilateral lumbar spinal stenosis. Eur Spine J 23:999–1006
Bhadresha A, Lawrence OJ, McCarthy MJ et al (2016) A comparison of magnetic resonance imaging muscle fat content in the lumbar paraspinal muscles with patient-reported outcome measures in patients with lumbar degenerative disk disease and focal disk prolapse. Global Spine J. 6:401–410
Knutsson B, Michaëlsson K, Sanden B (2013) Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish Spine register. Spine J. 38(5):435–441
Sigmundsson FG, Jönsson B, Strömqvist B (2013) Impact of pain on function and health related quality of life in lumbar spinal stenosis: a register study of 14,821 Patients. Spine J 38(15):937–945
Lozano-Alvarez C, Valencia MR, Adrover AM et al (2012) Can epidemiological factors predict the outcome of degenerative lumbar surgery? Bone Joint J 94:399
Weiner B, Fraser RD, Peterson M (1999) Spinous process osteotomies to facilitate lumbar decompressive surgery. Spine 24(1):62–66
Pressler JF, Heiss DG, Buford Jam et al (2006) Between-day repeatability and symmetry of multifidus cross-sectional area measured using ultrasound imaging. J Orthop Sport Phys Therapy 36(1):10–18
Hu ZJ, He J, Zhao FD et al (2011) An assessment of the intra- and inter-reliability of the lumbar paraspinal muscle parameters using CT scan and magnetic resonance imaging. Spine. 36(11):e868–e874
Modic MT, Steinberg PM, Ross JS et al (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166(1):193–199
Kang CH, Shin MJ, Kim SM et al (2007) MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol 62(5):479–486
Schizas C, Theumann N, Burn A et al (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine. 35(21):1919–1924
Haley SM, Osberg JS (1989) Kappa coefficient calculation using multiple ratings per subject: a special communication. J Am Phys Ther Assoc 69(11):970–974
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 327(8476):307–310
McDonald JH (2014). Handbook of Biological Statistics (3rd edn.) Sparky House Publishing, Baltimore, Maryland, pp 209–212
Lauridsen HH, Hartvigsen J, Manniche C et al (2006) Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord 7(82):2474–2482
Kääriäinen T, Taimela S, Aalto T et al (2016) The effect of decompressive surgery on lumbar paraspinal and biceps brachii muscle function and movement perception in lumbar spinal stenosis: a 2-year follow-up. Eur Spine J 25(3):789–794
Fan S, Hu Z, Zhao F et al (2010) Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J 19(2):316–324
Xia Y, Ishii K, Matsumoto M, Nakamura M et al (2008) Radiographic predictors of residual low back pain after laminectomy for lumbar spinal canal stenosis: minimum 5-year follow-up. J Spinal Disord Tech 21(3):153–158
Tabaraee E, Ahn J, Bohl DD et al (2015) Quantification of multifidus atrophy and fatty infiltration following a minimally invasive microdiscectomy. Int J Spine Surg 26(9):25
Mellado JM, Calmet J, Olona M et al (2005) Surgically repaired massive rotator cuff tears: mRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intra-operative and clinical findings. AJR Am J Roentgenol 184(5):1456–1463
Shen PH, Lien SB, Shen HC et al (2008) Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg 17(1 Suppl):1S–7S
Acknowledgements
Bernadette Mitchell, Spine Tango Database Coordinator, Royal Adelaide Hospital, Adelaide, South Australia is acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Zotti, M.G.T., Boas, F.V., Clifton, T. et al. Does pre-operative magnetic resonance imaging of the lumbar multifidus muscle predict clinical outcomes following lumbar spinal decompression for symptomatic spinal stenosis?. Eur Spine J 26, 2589–2597 (2017). https://doi.org/10.1007/s00586-017-4986-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-4986-x