Abstract
Purpose
The authors have developed a “para-midline” approach to the posterior lumbar spine using a virtually avascular surgical plane not previously described in the literature. It was their purpose to document consistent MRI presence of this plane and to prospectively evaluate its clinical use in terms of blood loss.
Methods
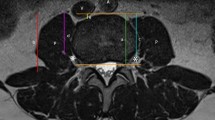
Fifty consecutive patients undergoing primary lumbar surgery on 1–3 levels were prospectively enrolled from September 2014 to May 2015. The para-midline approach was used in all cases. The deep lumbar fascia is longitudinally incised on either side of the spinous processes instead of directly in the midline, which reveals the para-midline fatty plane. Blood loss during the approach and overall blood loss were recorded for all patients. MRIs from each patient were reviewed by an experienced neuroradiologist to determine the presence of the para-midline fatty plane.
Results
There was no recorded blood loss during the approach for all procedures. The average overall blood loss was 60 cc (20–200 cc). No patient required a transfusion intraoperatively or postoperatively. The fatty para-midline plane was noted on preoperative MRI at all operated levels in all patients. The average width of this plane was 6.5 mm (2–17 mm).
Conclusions
The para-midline approach for lumbar surgery is associated with less blood loss than traditional, subperiosteal exposure techniques. The fatty interval through which this approach is made is universally present and identifiable on MRI. The authors offer this approach as a means of decreasing the risks associated with blood loss and transfusion with posterior lumbar surgery.





Similar content being viewed by others
References
Knoeller SM, Seifried C (2000) Historical perspective: history of spinal surgery. Spine 25(21):2838–2843
Weinstein SL (1994) The Pediatric spine: principles and practice. Raven Press, New York
Hoppenfeld S, DeBoer P, Buckley R (2009) Surgical exposures in orthopaedics: the anatomic approach, 4th edn. Wolters Kluwer/Lippincott Williams & Wilkins Health, Philadelphia
Herkowitz HN, Rothman RH (2011) Rothman-Simeone the spine, 6th edn. Saunders/Elsevier, Philadelphia
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. The Journal of bone and joint surgery American 50(5):919–926
Dazley JM, Deering RM, Bono CM (2013) Recurrent lumbar spinal stenosis: etiology and surgical management. Sem Spine Surg 25(4):283–294
Fritzell P, Hägg O, Wessberg P, Nordwall A (2002) Swedish Lumbar Spine Study Group: chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine 27(11):1131–1141
Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA (2001) Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine 26(5):567–571
Kakuchi M (1997) Reduction of blood loss during spinal surgery by epidural blockade under normotensive general anesthesia. Spine 22(8):889–894
Cha CW, Deible C, Muzzonigro T, Lopez-Plaza I, Vogt M, Kang JD (2002) Allogeneic transfusion requirements after autologous donations in posterior lumbar surgeries. Spine 27(1):99–104
Pradhan BB, Nassar JA, Delamarter RB, Wang JC (2002) Single-level lumbar spine fusion: a comparison of anterior and posterior approaches. J Spinal Disord Tech 15(5):355–361
Moller H, Hedlund R (2000) Instrumented and noninstrumented posterolateral fusion in adult spondylolisthesis–a prospective randomized study: part 2. Spine 25(13):1716–1721
Hostin R, McCarthy I, O’Brien M, Bess S, Line B, Boachie-Adjei O, Burton D, Gupta M, Ames C, Deviren V et al (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine 38(12):1008–1015
Ekman P, Moller H, Shalabi A, Yu YX, Hedlund R (2009) A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration. Eur Spine J 18(8):1175–1186
Buttermann GR, Mullin WJ (2013) Two-Level Circumferential Lumbar Fusion Comparing Midline and Paraspinal Posterior Approach: 5-Year Interim Outcomes of a Randomized, Blinded, Prospective Study. J Spinal Disorders Techn
Fraser RD, Hall DJ (1993) Laminectomy combined with posterolateral stabilisation: a muscle-sparing approach to the lumbosacral spine. Europ Spine J Off Publ Europ Spine Soc Europ Spinal Deform Soc Europ Sect Cervical Spine Res Soc 1(4):249–253
Mirza SK, Deyo RA, Heagerty PJ, Konodi MA, Lee LA, Turner JA, Goodkin R (2008) Development of an index to characterize the “invasiveness” of spine surgery. Spine 33(24):2651–2661
Zheng F, Cammisa FP Jr, Sandhu HS, Girardi FP, Khan SN (2002) Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine 27(8):818–824
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Charles H. Cho is on the Board of Directors for the North American Spine Society. Andrew J. Schoenfeld receives personal fees from Arbormetrix, royalties from Wolters Kluwer, and grant funding from the Robert Wood Johnson Foundation. Christopher M. Bono is the president of the North American Spine Society, consults for United Health Care, gives expert testimony for Crico, receives royalties from Wolters Kluwer, and recieves a stipend from JAAOS for being a deputy edictor. None of the above are relevant to the present article. None reported for all other authors.
Rights and permissions
About this article
Cite this article
Moghimi, M.H., Leonard, D.A., Cho, C.H. et al. Virtually bloodless posterior midline exposure of the lumbar spine using the “para-midline” fatty plane. Eur Spine J 25, 956–962 (2016). https://doi.org/10.1007/s00586-015-4319-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4319-x