Abstract
Purpose
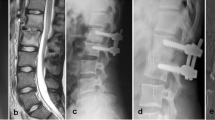
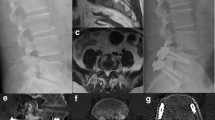
To determine the safety and efficacy of using a single posterior approach with transforaminal lumbar interbody debridement and fusion (TLIDF) plus pedicle screws fixation in treating infective spondylodiscitis in the lumbar spine.
Methods
Between January 2009 and June 2011, 28 patients with infective spondylodiscitis who underwent TLIDF, using autogenous graft and posterior pedicle screws instrumentation, met the indications for surgery, and completed more than 18 months of follow-up, were included. Clinical outcomes were assessed using a visual analog scale (VAS), the Oswestry Disability Index (ODI), and Kirkaldy-Willis functional outcome criteria. Infection status was evaluated using C-reactive protein levels, erythrocyte sedimentation rate, and clinical symptoms. The interbody fusion status and sagittal alignment of the infected segments were assessed using radiographic studies.
Results
Intra-operative culture rate was 82.1 %. The most common pathogen was methicillin-resistant Staphylococcus aureus. One post-operative deep wound infection with septic implant loosening and one instance of early aseptic implant loosening were noted. Implants in both patients were subsequently removed. Two infections recurred within 3 months post-operatively, with both subsiding within 3 months after extended antibiotic treatment. VAS and ODI values were significantly improved. The interbody fusion rate was 82.1 % and the lordotic angle of the infected segments and the lumbar spine were corrected by 9.7° and 14.3°, respectively at the last follow-up.
Conclusions
A single posterior approach with TLIDF and pedicle screws instrumentation for lumbar infective spondylodiscitis provided a satisfactory clinical outcome, adequate infection control and good fusion rate, and this strategy avoids the risks of anterior or staging surgeries.

Similar content being viewed by others
References
Wiley AM, Trueta J (1959) The vascular anatomy of the spine and its relationship to pyogenic vertebral osteomyelitis. J Bone Jt Surg Br 41:796–809
Batson OV (1967) The vertebral systemic of veins as a means for cancer dissemination. Prog Clin Cancer 3:1–18
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ (2000) Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976) 25:1668–1679
Sapico FL, Montgomerie JZ (1979) Pyogenic vertebral osteomyelitis: report of nine cases and review of the literature. Rev Infect Dis 1:754–776
Mehta JS, Bhojraj SY (2001) Tuberculosis of the thoracic spine. J Bone Jt Surg Br 83(6):859–863
Emery SE, Chan DP, Woodward HR (1989) Treatment of hematogenous pyogenic vertebral osteomyelitis with anterior debridement. Spine (Phila Pa 1976) 14:284–291
Hodgson AR, Stock FE, Fang HS, Ong GB (1960) Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg 48:172–178
Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL (2002) Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res 398:50–59
Sasso RC, Best NM, Mummaneni PV, Reilly TM, Hussain SM (2005) Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 30:670–674
Rath SA, Neff U, Schneider O, Richter HP (1996) Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurgery 38:926–933
Korovessis P, Petsinis G, Koureas G, Iliopoulos P, Zacharatos S (2006) Anterior surgery with insertion of titanium mesh cage and posterior instrumented fusion performed sequentially on the same day under one anesthesia for septic spondylitis of thoracolumbar spine: is the use of titanium mesh cages safe? Spine (Phila Pa 1976) 31:1014–1019
Ruf M, Stoltze D, Merk HR, Ames M, Harms J (2007) Treatment of vertebral osteomyelitis by radical debridement and stabilization using titanium mesh cages. Spine (Phila Pa 1976) 32:E275–E280
Pee YH, Park JD, Choi YG, Lee SH (2008) Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine 8:405–412
D’Aliberti G, Talamonti G, Villa F, Debernardi A (2012) The anterior stand-alone approach (ASAA) during the acute phase of spondylodiscitis: results in 40 consecutively treated patients. Eur Spine J 21(Suppl 1):S75–S82
Lee JS, Suh KT (2006) Posterior lumbar interbody fusion with an autogenous iliac crest bone graft in the treatment of pyogenic spondylodiscitis. J Bone Jt Surg Br 88:765–770
Fritzell P, Hagg O, Wessberg P, Nordwall A (2002) Chronic low back pain and fusion: a comparison of three surgical techniques: A prospective multicenter randomized study from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 27:1131–1141
Endres S, Wilke A (2012) Posterior interbody grafting and instrumentation for spondylodiscitis. J Orthop Surg (Hong Kong) 20:1–6
Yan DL, Pei FX, Li J, Soo CL (2008) Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J 17:1311–1316
Zaveri GR, Mehta SS (2009) Surgical treatment of lumbar tuberculous spondylodiscitis by transforaminal lumbar interbody fusion (TLIF) and posterior instrumentation. J Spinal Disord Tech 22(4):257–262
Rayes M, Colen CB, Bahqat DA et al (2010) Safety of instrumentation in patients with spinal infection. J Neurosurg Spine 12:647–659
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lu, ML., Niu, CC., Tsai, TT. et al. Transforaminal lumbar interbody debridement and fusion for the treatment of infective spondylodiscitis in the lumbar spine. Eur Spine J 24, 555–560 (2015). https://doi.org/10.1007/s00586-014-3585-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3585-3