Abstract
Purpose
We assessed the cerebrovascular CO2 reactivity (CO2R) in chronic renal failure (CRF) patients without diabetes mellitus (DM), uncontrolled hypertension, peripheral vascular disease, or neurological disease under isoflurane-nitrous oxide anesthesia.
Methods
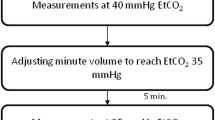
Forty-nine patients undergoing surgery, including 36 CRF patients (30 receiving dialysis and six pre-dialysis patients) and 13 patients without CRF (controls). Middle cerebral artery flow velocity (VMCA) was measured by transcranial Doppler ultrasonography at an end-tidal CO2 of 35 to 45 mmHg. CO2R was calculated as an absolute value (change in VMCA per mmHg PaCO2) and a relative value (absolute CO2R/baseline VMCA × 100). Factors associated with CO2R were evaluated simultaneously.
Results
Despite no significant differences in the absolute and relative values of CO2R between the CRF (mean 2.5 cm/s/mmHg; median 5.0%/mmHg) and control (2.4 cm/s/mmHg; 5.0%/mmHg) groups, blood urea nitrogen (BUN) concentrations in the CRF group correlated inversely with both absolute and relative CO2R. BUN concentration was higher (mean 72 versus 53 mg/dl, p = 0.006) and relative CO2R was lower (mean 2.6 versus 5.7%/mmHg, p = 0.011) in patients with pre-dialysis CRF (n = 6) versus CRF patients receiving dialysis (n = 30).
Conclusions
CO2R in CRF patients was not significantly different from that in controls. However, in CRF patients with high BUN concentrations, CO2R might be impaired, leading to reduced cerebrovascular reserve capacity. Because DM is a major cause of CRF and we excluded DM patients, our results might not be applicable to patients with DM-induced CRF.


Similar content being viewed by others
Change history
23 December 2017
In the original publication of the article, the first sentence was published incorrectly under the section “Patients and preoperative assessment”. The correct sentence should read as, “The Yamaguchi University Graduate School of Medicine Ethics Committee for Human Study approved the study protocol (18th August 2004: H16-71)”.
References
Koren-Morag N, Goldbourt U, Tanne D. Renal dysfunction and risk of ischemic stroke or TIA in patients with cardiovascular disease. Neurology. 2006;67:224–8.
Fazekas G, Fazekas F, Schmidt R, Kapeller P, Offenbacher H, Krejs GJ. Brain MRI findings and cognitive impairment in patients undergoing chronic hemodialysis treatment. J Neurol Sci. 1995;134:83–8.
Fazekas G, Fazekas F, Schmidt R, Flooh E, Valetitsch H, Kapeller P, Krejs GJ. Pattern of cerebral blood flow and cognition in patients undergoing chronic haemodialysis treatment. Nucl Med Commun. 1996;17:603–8.
Wolfgram DF, Sunio L, Vogt E, Smith HM, Visotcky A, Laud P, Whittle J. Haemodynamics during dialysis and cognitive performance. Nephrology (Carlton). 2014;19:771–6.
Plecha EJ, King TA, Pitluk HC, Rubin JR. Risk assessment in patients undergoing carotid endarterectomy. Cardiovasc Surg. 1993;1:30–2.
Rigdon EE, Monajjem N, Rhodes RS. Is carotid endarterectomy justified in patients with severe chronic renal insufficiency? Ann Vasc Surg. 1997;11:115–9.
Toh Y, Yano K, Takesue F, Korenaga D, Maekawa S, Muto Y, Ikeda T, Sugimachi K. Abdominal surgery for patients on maintenance hemodialysis. Surg Today. 1998;28:268–72.
Penta de Peppo A, Nardi P, De Paulis R, Pellegrino A, Forlani S, Scafuri A, Chiariello L. Cardiac surgery in moderate to end-stage renal failure: analysis of risk factors. Ann Thorac Surg. 2002;74:378–83.
Wang F, Dupuis JY, Nathan H, Williams K. An analysis of the association between preoperative renal dysfunction and outcome in cardiac surgery: estimated creatinine clearance or plasma creatinine level as measures of renal function. Chest. 2003;124:1852–62.
Ulrich PT, Becker T, Kempski OS. Correlation of cerebral blood flow and MCA flow velocity measured in healthy volunteers during acetazolamide and CO2 stimulation. J Neurol Sci. 1995;129:120–30.
Markus H, Cullinane M. Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain. 2001;124:457–67.
Kessler C, Junge HM, Walker ML, Busack R, Albrecht DM, von Ackeren K. Reduced cerebral vasomotor reactivity as an indicator of postoperative confusion. Anaesthesia. 1997;52:433–7.
Kadoi Y, Kawauchi C, Kuroda M, Takahashi K, Saito S, Fujita N, Mizutani A. Association between cerebrovascular carbon dioxide reactivity and postoperative short-term and long-term cognitive dysfunction in patients with diabetes mellitus. J Anesth. 2011;25:641–7.
Kuwabara Y, Sasaki M, Hirakata H, Koga H, Nakagawa M, Chen T, Kaneko K, Masuda K, Fujishima M. Cerebral blood flow and vasodilatory capacity in anemia secondary to chronic renal failure. Kidney Int. 2002;61:564–9.
Skinner H, Mackaness C, Bedforth N, Mahajan R. Cerebral haemodynamics in patients with chronic renal failure: effects of haemodialysis. Br J Anaesth. 2005;94:203–5.
Kawata R, Nakakimura K, Matsumoto M, Kawai K, Kunihiro M, Sakabe T. Cerebrovascular CO2 reactivity during anesthesia in patients with diabetes mellitus and peripheral vascular disease. Anesthesiology. 1998;89:887–93.
Kado Y, Hinohara H, Kunimoto F, Saito S, Ide M, Hiraoka H, Kawahara F, Goto F. Diabetic patients have an impaired cerebral vasodilatory response to hypercapnia under propofol anesthesia. Stroke. 2003;34:2399–403.
Lasek-Bal A, Kazibutowska Z, Golba A, Motta E. Cerebral vasoreactivity in hypocapnia and hypercapnia in patients with diabetes mellitus type 2 with or without arterial hypertension. Neurol Neurochir Pol. 2012;46:529–35.
Serrador JM, Sorond FA, Vyas M, Gagnon M, Iloputaife ID, Lipsitz LA. Cerebral pressure-flow relations in hypertensive elderly humans: transfer gain in different frequency domains. J Appl Physiol. 2005;98:151–9.
Wijnhoud AD, Koudstaal PJ, Dippel DW. Relationships of transcranial blood flow Doppler parameters with major vascular risk factors: TCD study in patients with a recent TIA or nondisabling ischemic stroke. J Clin Ultrasound. 2006;34:70–6.
Kanai H, Hirakata H, Nakane H, Fujii K, Hirakata E, Ibayashi S, Kuwabara Y. Depressed cerebral oxygen metabolism in patients with chronic renal failure: a positron emission tomography study. Am J Kidney Dis. 2001;38:S129–33.
Holzer H, Marguc K, Pogglitsch H, Ott E, Katschnig H. The effects of haemodialysis on cerebral blood flow. Proc Eur Dial Transpl Assoc. 1981;18:126–32.
Lipsitz LA, Mukai S, Hamner J, Gagnon M, Babikian V. Dynamic regulation of middle cerebral artery blood flow velocity in aging and hypertension. Stroke. 2000;31:1897–903.
Hata R, Matsumoto M, Handa N, Terakawa H, Sugitani Y, Kamada T. Effects of hemodialysis on cerebral circulation evaluated by transcranial Doppler ultrasonography. Stroke. 1994;25:408–12.
Hughes JR. Correlations between EEG and chemical changes in uremia. Electroencephalogr Clin Neurophysiol. 1980;48:583–94.
van de Ven M, Colier WN, Kersten BT, Oeseburg B, Folgering H. Cerebrovascular response to acute metabolic acidosis in humans. Adv Exp Med Biol. 2003;530:707–15.
Szprynger K, Kwiecinski J, Szczepanska M, Pierzchala K. Evaluation of cerebrovascular reactivity in children (corrected) with chronic renal failure. Pediatr Nephrol. 2000;14:993–6.
Kamano C, Komaba Y, Sakayori O, Iino Y, Katayama Y. Decreased cerebral blood flow in renal transplant recipients. Intern Med. 2002;41:677–83.
Evers S, Tepel M, Obladen M, Suhr B, Husstedt IW, Grotemeyer KH, Zidek W. Influence of end-stage renal failure and hemodialysis on event-related potentials. J Clin Neurophysiol. 1998;15:58–63.
Iseki K. Predictors of diabetic end-stage renal disease in Japan. Nephrology. 2005;10:S2–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This work was supported by a grant from the Ministry of Education, Science, Sports and Culture of Japan (no. 22591734 for Kazuyoshi Ishida).
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00540-017-2443-y.
About this article
Cite this article
Ishida, K., Uchida, M., Utada, K. et al. Cerebrovascular CO2 reactivity during isoflurane-nitrous oxide anesthesia in patients with chronic renal failure. J Anesth 32, 15–22 (2018). https://doi.org/10.1007/s00540-017-2422-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2422-3