Abstract
Background
Although there are several studies on the association between use of proton pump inhibitors (PPIs) and increased Clostridium difficile infection (CDI) risk, detailed studies analyzing the effects of PPI use on CDI risk are lacking. The present study investigated the association of the dose, duration, and types of PPIs with CDI risk.
Methods
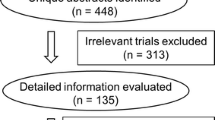
A single-center, cohort study was conducted on patients admitted to a hospital. The exposed cohort comprised patients who were prescribed PPIs at least once during the study period, and a control cohort was prepared by randomly assigning an index date to patients who did not use PPIs ensuring the same distribution of index dates as in the exposed cohort and matching sex, age, hospitalization period, and date of admission.
Results
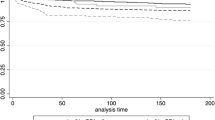
PPI use increased the risk of CDI by 1.8-fold [95% confidence interval (CI) 1.5–2.2]. CDI risk increased by 1.8-fold with esomeprazole (95% CI 1.4–2.2) and 2.0-fold with pantoprazole (95% CI 1.5–2.8). Patients who used a high dose had a higher risk than those who used a medium dose [adjusted hazard ratio (HR) 2.0 vs 1.3]. The risk of CDI increased 4.2-fold when the PPI exposure period was 6 days or shorter than 6 days.
Conclusions
Our study showed that PPI use was associated with an increased risk of developing CDI and the risk of CDI was dose dependent. Therefore, PPIs should only be used at proper doses and only for the necessary indications to avoid CDI risk.


Similar content being viewed by others
References
Lodato F, Poluzzi E, Raschi E, et al. Appropriateness of proton pump inhibitor (PPI) prescription in patients admitted to hospital: attitudes of general practitioners and hospital physicians in Italy. Eur J Intern Med. 2016;30:31–6.
Zink DA, Pohlman M, Barnes M, et al. Long-term use of acid suppression started inappropriately during hospitalization. Aliment Pharmacol Ther. 2005;21:1203–9.
Reid M, Keniston A, Heller JC, et al. Inappropriate prescribing of proton pump inhibitors in hospitalized patients. J Hosp Med. 2012;7:421–5.
Schoenfeld AJ, Grady D. Adverse effects associated with proton pump inhibitors. JAMA Intern Med. 2016;176:172–4.
Cheungpasitporn W, Thongprayoon C, Kittanamongkolchai W, et al. Proton pump inhibitors linked to hypomagnesemia: a systematic review and meta-analysis of observational studies. Ren Fail. 2015;37:1237–41.
Kwok CS, Arthur AK, Anibueze CI, et al. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. Am J Gastroenterol. 2012;107:1011–9.
Eom CS, Jeon CY, Lim JW, et al. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011;183:310–9.
Depestel DD, Aronoff DM. Epidemiology of Clostridium difficile infection. J Pharm Pract. 2013;26:464–75.
Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372:1539–48.
Nehra AK, Alexander JA, Loftus CG, et al. Proton pump inhibitors: review of emerging concerns. Mayo Clin Proc. 2018;93:240–6.
Dubberke ER, Olsen MA, Stwalley D, et al. Identification of medicare recipients at highest risk for Clostridium difficile infection in the US by population attributable risk analysis. PLoS ONE. 2016;11:e0146822.
Loo VG, Bourgault AM, Poirier L, et al. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med. 2011;365:1693–703.
Wei L, Ratnayake L, Phillips G, et al. Acid-suppression medications and bacterial gastroenteritis: a population-based cohort study. Br J Clin Pharmacol. 2017;83:1298–308.
Garcia Rodriguez LA, Ruigomez A, Panes J. Use of acid-suppressing drugs and the risk of bacterial gastroenteritis. Clin Gastroenterol Hepatol. 2007;5:1418–23.
Dial S, Alrasadi K, Manoukian C, et al. Risk of Clostridium difficile diarrhea among hospital inpatients prescribed proton pump inhibitors: cohort and case-control studies. CMAJ. 2004;171:33–8.
Trifan A, Stanciu C, Girleanu I, et al. Proton pump inhibitors therapy and risk of Clostridium difficile infection: systematic review and meta-analysis. World J Gastroenterol. 2017;23:6500–15.
Oshima T, Wu L, Li M, et al. Magnitude and direction of the association between Clostridium difficile infection and proton pump inhibitors in adults and pediatric patients: a systematic review and meta-analysis. J Gastroenterol. 2018;53:84–94.
Tariq R, Singh S, Gupta A, et al. Association of gastric acid suppression with recurrent Clostridium difficile infection: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:784–91.
FDA Drug Safety Communication. Clostridium difficile associated diarrhea can be associated with stomach acid drugs known as proton pump inhibitors (PPIs). https://www.fda.gov/Drugs/DrugSafety/ucm290510.htm. Accessed 30 Dec 2018.
Lisi D. Pharmacotherapy self-assessment program 2018 BOOK1 infectious diseases. Lenexa: American College of Clinical Pharmacy; 2018.
Pai VG, Pai NV, Thacker HP, et al. Comparative clinical trial of S-pantoprazole versus racemic pantoprazole in the treatment of gastro-esophageal reflux disease. World J Gastroenterol. 2006;12:6017–20.
Dexlansoprazole. https://www.pdr.net/drug-summary/Dexilant-dexlansoprazole-558.6197. Accessed 13 May 2019
Wang L, Zhou L, Lin S, et al. A new PPI, ilaprazole compared with omeprazole in the treatment of duodenal ulcer: a randomized double-blind multicenter trial. J Clin Gastroenterol. 2011;45:322–9.
Revaprazan hydrochloride. https://www.pharmacodia.com/yaodu/html/v1/chemicals/7ec2442aa04c157590b2fa1a7d093a33.html. Accessed 13 May 2019
Dalton BR, Lye-Maccannell T, Henderson EA, et al. Proton pump inhibitors increase significantly the risk of Clostridium difficile infection in a low-endemicity, non-outbreak hospital setting. Aliment Pharmacol Ther. 2009;29:626–34.
Seto CT, Jeraldo P, Orenstein R, et al. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42.
Mylotte JM. Laboratory surveillance method for nosocomial Clostridium difficile diarrhea. Am J Infect Control. 1998;26:16–23.
Hensgens MP, Goorhuis A, Dekkers OM, et al. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012;67:742–8.
Stevens V, Dumyati G, Fine LS, et al. Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis. 2011;53:42–8.
Hung YP, Lee JC, Lin HJ, et al. Clinical impact of Clostridium difficile colonization. J Microbiol Immunol Infect. 2015;48:241–8.
Dial S, Delaney JA, Barkun AN, et al. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989–95.
Lewis PO, Litchfield JM, Tharp JL, et al. Risk and severity of hospital-acquired Clostridium difficile infection in patients taking proton pump inhibitors. Pharmacotherapy. 2016;36:986–93.
Hamzat H, Sun H, Ford JC, et al. Inappropriate prescribing of proton pump inhibitors in older patients: effects of an educational strategy. Drugs Aging. 2012;29:681–90.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, Y.H., Seong, J.M., Cho, S. et al. Effects of proton pump inhibitor use on risk of Clostridium difficile infection: a hospital cohort study. J Gastroenterol 54, 1052–1060 (2019). https://doi.org/10.1007/s00535-019-01598-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-019-01598-2