Abstract
Purpose
Sequelae of and therapies for head and neck cancers (HNC) are associated with physical and functional impairment as well as increased levels of psychological distress post treatment. Given the impact of HNC and treatment on functioning (i.e., eating and talking), health-related quality of life (HRQOL) is a significant area of survivorship concern within this population. Although prior research indicates that the incidence of anxiety and depression ranges from 15 to 50%, to date, there is a paucity of research on specific psychosocial interventions related to HNC treatment and completed studies have been limited by infrequent use of a randomized design and provision of non-standardized psychosocial interventions. This study aimed to address these gaps and utilize a brief cognitive behavioral intervention (CBI) to improve (1) self-efficacy for coping with cancer, (2) depressive symptoms, (3) other psychological symptoms, and (4) HRQOL among patients with HNC.
Methods
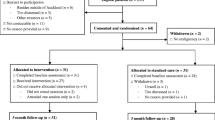
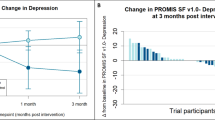
In an effort to conduct a randomized clinical trial of those undergoing treatment for HNC, eighty-eight patients were assigned to receive either a standardized CBI or usual psychological care (N = 47 and 41, respectively) with a 1-year follow-up. The means of all variables for both groups, adjusted for baseline, were visually compared at 3, 6, and 12 months post treatment.
Results
As has been a challenge in other longitudinal HNC studies, a high degree of attrition occurred, with a loss of 35 patients from the CBI group and 29 from the usual care group. Despite the high attrition, analysis of existing data indicated that the effect of CBI was discernable among the patients who completed the course of the study. Of the 38 comparisons, 34 showed that the CBI group had the favorable outcome. Important considerations for implementation of a structured psychotherapy intervention during active cancer treatment with multiple barriers including communication challenges and practical limitations were realized.
Conclusions
The impact of HNC treatment can be particularly distressing as it often results in functional impairment and markedly changed activities of daily living among survivors. However, engaging in therapeutic methods to cope and manage distress during treatment can influence QOL and mood into the survivorship phase.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33. https://doi.org/10.3322/caac.21708
Senchak JJ, Fang CY, Bauman JR (2019) Interventions to improve quality of life (QOL) and/or mood in patients with head and neck cancer (HNC): a review of the evidence. Cancers Head Neck 4(1):1–11. https://doi.org/10.1186/s41199-019-0041-4
Hammerlid E, Ahlner-Elmqvist M, Bjordal K et al (1999) A prospective multicentre study in Sweden and Norway of mental distress and psychiatric morbidity in head and neck cancer patients. Br J Cancer 80(5-6):766–774. https://doi.org/10.1038/sj.bjc.6690420
Kugaya A, Akechi T, Okuyama T et al (2000) Prevalence, predictive factors, and screening for psychologic distress in patients with newly diagnosed head and neck cancer. Cancer 88(12):2817–2823. https://doi.org/10.1002/1097-0142(20000615)88:12<2817::aid-cncr22>3.0.co;2-n
Lydiatt W, Moran J, Burke W (2009) A review of depression in the head and neck cancer patient. Clin Adv Hematol Oncol 7(6):397–403
Sehlen S, Lenk M, Herschbach P et al (2003) Depressive symptoms during and after radiotherapy for head and neck cancer. Head Neck 25(12):1004–1018. https://doi.org/10.1002/hed.10336
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S (2001) The prevalence of psychological distress by cancer site. Psycho-Oncology 10(1):19–28. https://doi.org/10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6
Pandey M, Devi N, Thomas BC, Vinod Kumar S, Krishnan R, Ramdas K (2007) Distress overlaps with anxiety and depression in patients with head and neck cancer. Psycho-Oncology 16(6):582–586. https://doi.org/10.1002/pon.1123
Mehnert A, Brähler E, Faller H et al (2014) Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol 32(31):3540–3546. https://doi.org/10.1200/jco.2014.56.0086
Kam D, Salib A, Gorgy G et al (2015) Incidence of suicide in patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg 141(12):1075. https://doi.org/10.1001/jamaoto.2015.2480
List M, Mumby P, Haraf D et al (1997) Performance and quality of life outcome in patients completing concomitant chemoradiotherapy protocols for head and neck cancer. Qual Life Res 6(3):274–284. https://doi.org/10.1023/A:1026419023481
Tschiesner UM, Rogers SN, Harreus U, Berghaus A, Cieza A (2009) Comparison of outcome measures in head and neck cancer-literature review 2000-2006. Head Neck 31(2):251–259. https://doi.org/10.1002/hed.20960
DeBoer M, Van Den Borne B, Pruyn J et al (1998) Psychosocial and physical correlates of survival and recurrence in patients with head and neck carcinoma: results of a 6-year longitudinal study. Cancer 83(12):2567–2579
Fang F-M, Liu Y-T, Tang Y, Wang C-J, Ko S-F (2004) Quality of life as a survival predictor for patients with advanced head and neck carcinoma treated with radiotherapy. Cancer 100(2):425–432. https://doi.org/10.1002/cncr.20010
Allison PJ, Guichard C, Fung K, Gilain L (2003) Dispositional optimism predicts survival status 1 year after diagnosis in head and neck cancer patients. J Clin Oncol 21(3):543–548. https://doi.org/10.1200/jco.2003.10.092
Coyne JC, Pajak TF, Harris J et al (2007) Emotional well-being does not predict survival in head and neck cancer patients. Cancer 110(11):2568–2575. https://doi.org/10.1002/cncr.23080
Grignon LM (2007) General health measures and long-term survival in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 133(5):471–476. https://doi.org/10.1001/archotol.133.5.471
Siddiqui F, Pajak TF, Watkins-Bruner D et al (2008) Pretreatment quality of life predicts for locoregional control in head and neck cancer patients: a radiation therapy oncology group analysis. Int J Radiat Oncol Biol Phys 70(2):353–360. https://doi.org/10.1016/j.ijrobp.2007.06.024
Mehanna HM, De Boer MF, Morton RP (2008) The association of psycho-social factors and survival in head and neck cancer. Clin Otolaryngol 33(2):83–89. https://doi.org/10.1111/j.1749-4486.2008.01666.x
Meyer F, Fortin A, Gélinas M et al (2009) Health-related quality of life as a survival predictor for patients with localized head and neck cancer treated with radiation therapy. J Clin Oncol 27(18):2970–2976. https://doi.org/10.1200/jco.2008.20.0295
Merluzzi TV, Martinez Sanchez MA (1997) Assessment of self-efficacy and coping with cancer: development and validation of the cancer behavior inventory. Health Psychol 16(2):163–170. https://doi.org/10.1037/0278-6133.16.2.163
Bandura A (1991) Self-efficacy mechanism in physiological activation and health-promoting behavior. In: Madden J (ed) Neurobiology of learning, emotion and affect. Raven, New York, NY, pp 229–270
Luszczynska A, Mohamed NE, Schwarzer R (2005) Self-efficacy and social support predict benefit finding 12 months after cancer surgery: the mediating role of coping strategies. Psychol Health Med 10(4):365–375. https://doi.org/10.1080/13548500500093738
Fiegenbaum W (1981) A social training program for clients with facial disfigurations. Int J Rehabil Res 4(4):501–510. https://doi.org/10.1097/00004356-198112000-00003
Myers EN, Hammerlid E, Persson L-O, Sullivan M, Westin T (1999) Quality-of-life effects of psychosocial intervention in patients with head and neck cancer. Otolaryngol Head Neck Surg 120(4):507–516. https://doi.org/10.1053/hn.1999.v120.a90352
Katz MR, Irish JC, Devins GM (2004) Development and pilot testing of a psychoeducational intervention for oral cancer patients. Psycho-Oncology 13(9):642–653. https://doi.org/10.1002/pon.767
Vilela LD, Nicolau B, Mahmud S et al (2006) Comparison of psychosocial outcomes in head and neck cancer patients receiving a coping strategies intervention and control subjects receiving no intervention. J Otolaryngol 35(2):88–96. https://doi.org/10.2310/7070.2005.5002
Allison PJ, Edgar L, Nicolau B, Archer J, Black M, Hier M (2004) Results of a feasibility study for a psycho-educational intervention in head and neck cancer. Psycho-Oncology 13(7):482–485. https://doi.org/10.1002/pon.816
Semple CJ, Dunwoody L, Kernohan WG, McCaughan E (2008) Development and evaluation of a problem-focused psychosocial intervention for patients with head and neck cancer. Support Care Cancer 17(4):379–388. https://doi.org/10.1007/s00520-008-0480-7
Kangas M, Milross C, Taylor A, Bryant RA (2012) A pilot randomized controlled trial of a brief early intervention for reducing posttraumatic stress disorder, anxiety and depressive symptoms in newly diagnosed head and neck cancer patients. Psycho-Oncology 22(7):1665–1673. https://doi.org/10.1002/pon.3208
Cohen A, Ianovski LE, Frenkiel S et al (2018) Barriers to psychosocial oncology service utilization in patients newly diagnosed with head and neck cancer. Psycho-Oncology 27(12):2786–2793. https://doi.org/10.1002/pon.4889
Bachmann A-S, Wiltfang J, Hertrampf K (2021) Development of the German speech intelligibility index for the treatment of oral cancer patients. J Cranio-Maxillofac Surg 49(1):52–58. https://doi.org/10.1016/j.jcms.2020.11.009
Beck AT, Steer RA, Brown G (1996) Beck Depression Inventory–II. PsycTESTS Dataset 10(3). https://doi.org/10.1037/t00742-000
Derogatis LR (2000) BSI 18, Brief Symptom Inventory 18: administration, scoring and procedures manual. PsycTESTS Dataset. https://doi.org/10.1037/t07502-000
Zabora J, Brintzenhofeszoc K, Jacobsen P et al (2001) A new psychosocial screening instrument for use with cancer patients. Psychosomatics 42(3):241–246. https://doi.org/10.1176/appi.psy.42.3.241
List MA, D'Antonio LL, Cella DF et al (1996) The performance status scale for head and neck cancer patients and the functional assessment of cancer therapy-head and neck scale: a study of utility and validity. Cancer 77(11):2294–2301. https://doi.org/10.1002/(sici)1097-0142(19960601)77:11<2294::aid-cncr17>3.0.co;2-s
Cella D (1997) F.A.C.I.T. Manual: Manual of the functional assessment of chronic illness therapy (FACIT) scales (version 4). Center on Outcomes Research and Education (CORE), Evanston Northwestern Healthcare and Northwestern University
Heitzmann CA, Merluzzi TV, Jean-Pierre P, Roscoe JA, Kirsh KL, Passik SD (2011) Assessing self-efficacy for coping with cancer: development and psychometric analysis of the brief version of the cancer behavior inventory (CBI-B). Psycho-Oncology 20(3):302–312. https://doi.org/10.1002/pon.1735
Posavac EJ, Carey RG (1989) Program evaluation : methods and cases studies (3rd edition). Prentice Hall, Hoboken, NJ
Josselin JM, Le Maux B (2017) Statistical tools for program evaluation: methods and applications to economic policy, public health, and education. Springer, New York
de Graeff A, de Leeuw JR, Ros WJG, Hordijk G-J, Blijham GH, Winnubst JAM (2000) Long-term quality of life of patients with head and neck cancer. Laryngoscope 110(1):98–106. https://doi.org/10.1097/00005537-200001000-00018
Nelke K, Pawlak W, Gerber H, Leszczyszyn J (2014) Head and neck cancer patients’ quality of life. Adv Clin Exp Med 23(6):1019–1027. https://doi.org/10.17219/acem/37361
Patsopoulos NA (2011) A pragmatic view on pragmatic trials. Dialogues Clin Neurosci 13(2):217–224. https://doi.org/10.31887/DCNS.2011.13.2/npatsopoulos
Cella D, Hahn EA, Dineen K (2002) Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res 11(3):207–221. https://doi.org/10.1023/a:1015276414526
Carmack CL, Basen-Engquist K, Yuan Y, Greisinger A, Rodriguez-Bigas M, Wolff RA et al (2011) Feasibility of an expressive-disclosure group intervention for post-treatment colorectal cancer patients: results of the Healthy Expressions study. Cancer 117(21):4993–5002
Serfaty M, King M, Nazareth I, Moorey S, Aspden T, Mannix K et al (2020) Effectiveness of cognitive–behavioural therapy for depression in advanced cancer: CanTalk randomised controlled trial. Br J Psychiatry 216(4):213–221
Russell L, Gough K, Drosdowsky A, Schofield P, Aranda S, Butow PN et al (2015) Psychological distress, quality of life, symptoms and unmet needs of colorectal cancer survivors near the end of treatment. J Cancer Surviv 9:462–470
Jones JM, Ferguson S, Edwards E, Walton T, McCurdy N, Howell D (2012) Experiences of care delivery: endometrial cancer survivors at end of treatment. Gynecol Oncol 124(3):458–464
Parry C, Morningstar E, Kendall J, Coleman EA (2011) Working without a net: leukemia and lymphoma survivors’ perspectives on care delivery at end-of-treatment and beyond. J Psychosoc Oncol 29(2):175–198
Braz DSA, Ribas MM, Dedivitis RA, Nishimoto IN, Barros APB (2005) Quality of life and depression in patients undergoing total and partial laryngectomy. Clinics 60:135–142
Eadie T, Faust L, Bolt S, Kapsner-Smith M, Pompon RH, Baylor C et al (2018) Role of psychosocial factors on communicative participation among survivors of head and neck cancer. Otolaryngol Head Neck Surg 159(2):266–273
Betiar A, Khorrami NS, Makvandi B (2022) Effectiveness of cognitive-behavioral therapy and mental imagery on hope and self-efficacy of patients with leukemia and lymphoma. Int J Health Studies 9(1):7–11
Fang CY, Galloway TJ, Egleston BL, Bauman JR, Ebersole B, Chwistek M et al (2020) Development of a web-based supportive care program for patients with head and neck cancer. Front Oncol 10:602202
LeFort SM (1993) The statistical versus clinical significance debate. Image J Nurs Sch 25(1):57–62
Acknowledgements
We would like to express appreciation for the collaborating medical providers who assisted with this study and the care of patients. Finally, thank you to the patients who gave their time during a period of great hardship.
Funding
This study was funded by a New Investigator internal grant from the Research Funding Committee of Loyola University Medical Center.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Drs. Thilges, Mumby, Clark, and Czerlanis and analysis was performed by Dr. James Sinacore. The first draft of the manuscript was written by Dr. Sarah Thilges and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of Loyola University Medical Center on 3/16/2011.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thilges, S., Mumby, P., Sinacore, J. et al. Implementing a cognitive behavioral intervention for patients with head and neck cancer. Support Care Cancer 31, 476 (2023). https://doi.org/10.1007/s00520-023-07948-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07948-4