Abstract
Purpose
To quantify the relationship between diabetes and fatigue from pre-chemotherapy to 6 months post-chemotherapy for women with breast cancer compared to women without a history of cancer (controls).
Methods
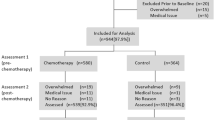
This was a secondary analysis from a nationwide prospective longitudinal study of female patients with breast cancer undergoing chemotherapy and controls. Diabetes diagnosis (yes/no) was obtained at baseline, and cancer-related fatigue was measured using the Multidimensional Fatigue Symptom Inventory (MFSI) pre-, post-, and 6 months post-chemotherapy in patients; controls were assessed at equivalent time points. Repeated measures mixed effects models estimated the association between fatigue and diabetes controlling for cancer (yes/no), body mass index, exercise and smoking habits, baseline anxiety and depressive symptoms, menopausal status, marital status, race, and education.
Results
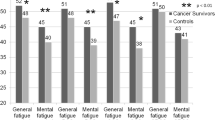
Among 439 patients and 235 controls (52.8 ± 10.5 years old), diabetes was twice as prevalent among patients as controls (11.6% vs. 6.8%). At baseline, diabetes was associated with worse fatigue (4.1 ± 1.7 points, p = 0.017). Also, diabetes was associated with clinically meaningful worse fatigue throughout the study period among all participants (5.2 ± 1.9 points, p = 0.008) and patients alone (4.5 ± 2.0, p = 0.023). For the MFSI subdomains among patients, diabetes was associated with worse general (p = 0.005) and mental fatigue (p = 0.026).
Conclusions
Diabetes was twice as prevalent in women with breast cancer compared to controls, and diabetes was associated with more severe cancer-related fatigue in patients before and after chemotherapy and at 6 months post-chemotherapy. Interventions that address diabetes management may also help address cancer-related fatigue during chemotherapy treatment.
Trial registration
ClinicalTrials.gov identifier: NCT01382082, first posted June 27, 2011.

Similar content being viewed by others
Data availability
The datasets and statistical code generated during and analyzed during the current study are available from the corresponding and last author on reasonable request.
References
Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, Cleeland C, Dotan E, Eisenberger MA, Escalante CP et al (2015) Cancer-related fatigue, version 2.2015, Clinical Practice Guidelines in Oncology. Nat Comp Cancer Netw 13(8):1012–1039
Servaes P, Verhagen C, Bleijenberg G (2002) Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer 38:27–43
Al Maqbali M, Al Sinani M, Al Naamani Z, Al Badi K, Tanash MI (2020) Prevalence of fatigue in patients with cancer: a systematic review and meta-analysis. J Pain Symptom Manage
Jones JM, Olson K, Catton P, Catton CN, Fleshner NE, Krzyzanowska MK, McCready DR, Wong RK, Jiang H, Howell D (2016) Cancer-related fatigue and associated disability in post-treatment cancer survivors. J Cancer Surviv 10(1):51–61
Bower JE, Wiley J, Petersen L, Irwin MR, Cole SW, Ganz PA (2018) Fatigue after breast cancer treatment: biobehavioral predictors of fatigue trajectories. Health Psychol 37(11):1025–1034
Bower JE (2014) Cancer-related fatigue—mechanisms risk factors and treatments. Nat Rev Clin Oncol 11(Oct):597–609
Horneber M, Fischer I, Dimeo F, Ruffer JU, Weis J (2012) Cancer-related fatigue: epidemiology, pathogenesis, diagnosis, and treatment. Dtsch Arztebl Int 109(9):161–171 (quiz 172)
Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR (2007) Cancer-related fatigue: the scale of the problem. Oncologist 12(Suppl 1):4–10
Saligan LN, Olson K, Filler K, Larkin D, Cramp F, Yennurajalingam S, Escalante CP, del Giglio A, Kober KM, Kamath J et al (2015) The biology of cancer-related fatigue: a review of the literature. Support Care Cancer 23(8):2461–2478
O’Higgins CM, Brady B, O’Connor B, Walsh D, Reilly RB (2018) The pathophysiology of cancer-related fatigue: current controversies. Support Care Cancer 26(10):3353–3364
Grossberg AJ, Vichaya EG, Gross PS, Ford BG, Scott KA, Estrada D, Vermeer DW, Vermeer P, Dantzer R (2020) Interleukin 6-independent metabolic reprogramming as a driver of cancer-related fatigue. Brain Behav Immun 88:230–241
Inglis JE, Janelsins MC, Culakova E, Mustian KM, Lin PJ, Kleckner IR, Peppone LJ 2020 Longitudinal assessment of the impact of higher body mass index on cancer-related fatigue in patients with breast cancer receiving chemotherapy. Support Care Cancer.
American Diabetes Association: CDC national diabetes statistics report, 2017. In. Arlington, VA; 2017.
Srokowski TP, Fang S, Hortobagyi GN, Giordano SH (2009) Impact of diabetes mellitus on complications and outcomes of adjuvant chemotherapy in older patients with breast cancer. J Clin Oncol 27(13):2170–2176
van Herpt TTW, van de Schans SAM, Haak HR, van Spronsen DJ, Dercksen MW, Janssen-Heijnen MLG (2011) Treatment and outcome in non-Hodgkin’s lymphoma patients with and without prevalent diabetes mellitus in a population-based cancer registry. Journal of Geriatric Oncology 2(4):239–245
Karlin NJ, Dueck AC, Nagl Reddy SK, Verona PM, Cook CB (2014) Implications of breast cancer with diabetes mellitus on patient outcomes and care. Diabetes Management 4(5):1–9
Lee SY, Kurita N, Yokoyama Y, Seki M, Hasegawa Y, Okoshi Y, Chiba S (2014) Glucocorticoid-induced diabetes mellitus in patients with lymphoma treated with CHOP chemotherapy. Support Care Cancer 22(5):1385–1390
Singh R, Teel C, Sabus C, McGinnis P, Kluding P (2016) Fatigue in type 2 diabetes: impact on quality of life and predictors. PLoS ONE 11(11):e0165652
Storey S, Cohee A, Gathirua-Mwangi WG, Vachon E, Monahan P, Otte J, Stump TE, Cella D, Champion V (2019) Impact of diabetes on the symptoms of breast cancer survivors. Oncol Nurs Forum 46(4):473–484
Janelsins MC, Heckler CE, Peppone LJ, Ahles TA, Mohile SG, Mustian KM, Palesh O, O’Mara AM, Minasian LM, Williams AM et al (2018) Longitudinal trajectory and characterization of cancer-related cognitive impairment in a nationwide cohort study. J Clin Oncol 32(36):3231–3239
Janelsins MC, Heckler CE, Peppone LJ, Kamen C, Mustian KM, Mohile SG, Magnuson A, Kleckner IR, Guido JJ, Young KL et al (2017) Cognitive complaints in survivors of breast cancer after chemotherapy compared with age-matched controls: an analysis from a nationwide, multicenter, prospective longitudinal study. J Clin Oncol 35(5):506–514
Stein KD, Jacobsen PB, Blanchard CM, Thors C (2004) Further validation of the multidimensional fatigue symptom inventory-short form. J Pain Symptom Manage 27(1):14–23
Spielberger CD, Sydeman SJ, Owen AE, et al. 1999 Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI). In: The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. edn. Edited by Maruish ME. Mahwah, NJ: Lawrence Erlbaum Associates. 993–1021
Chan A, Yo TE, Wang XJ, Ng T, Chae JW, Yeo HL, Shwe M, Gan YX (2018) Minimal clinically important difference of the Multidimensional Fatigue Symptom Inventory-Short Form (MFSI-SF) for fatigue worsening in Asian breast cancer patients. J Pain Symptom Manage 55(3):992-997 e992
Williams AM, Paterson C, Heckler CE, Barton DL, Ontko M, Geer J, Kleckner AS, Dakhil SR, Mitchell JM, Mustian KM et al: Cancer-related fatigue, anxiety, and quality of life in breast cancer patients compared to non-cancer controls: a nationwide longitudinal analysis. Breast Cancer Reserach and Treatment in press.
Ancoli-Israel S, Liu L, Marler MR, Parker BA, Jones V, Sadler GR, Dimsdale J, Cohen-Zion M, Fiorentino L (2006) Fatigue, sleep, and circadian rhythms prior to chemotherapy for breast cancer. Support Care Cancer 14(3):201–209
Hammer MJ, Aouizerat BE, Schmidt BL, Cartwright F, Wright F, Miaskowski C (2015) Glycosylated hemoglobin A1c and lack of association with symptom severity in patients undergoing chemotherapy for solid tumors. Oncol Nurs Forum 42(6):581–590
Oh HS, Seo WS (2011) Systematic review and meta-analysis of the correlates of cancer-related fatigue. Worldviews Evid Based Nurs 8(4):191–201
Hughes A, Suleman S, Rimes KA, Marsden J, Chalder T (2020) Cancer-related fatigue and functional impairment - towards an understanding of cognitive and behavioural factors. J Psychosom Res 134:110127
Tchen N, Juffs HG, Downie FP, Yi QL, Hu H, Chemerynsky I, Clemons M, Crump M, Goss PE, Warr D et al (2003) Cognitive function, fatigue, and menopausal symptoms in women receiving adjuvant chemotherapy for breast cancer. J Clin Oncol 21(22):4175–4183
Peppone LJ, Mustian KM, Morrow GR, Dozier AM, Ossip DJ, Janelsins MC, Sprod LK, McIntosh S (2011) The effect of cigarette smoking on cancer treatment-related side effects. Oncologist 16(12):1784–1792
Hershey DS (2017) Importance of glycemic control in cancer patients with diabetes: treatment through end of life. Asia Pac J Oncol Nurs 4(4):313–318
Hershey DS, Pierce SJ (2015) Examining patterns of multivariate, longitudinal symptom experiences among older adults with type 2 diabetes and cancer via cluster analysis. Eur J Oncol Nurs 19(6):716–723
Hammer MJ, Eckardt P, Cartwright F, Miaskowski C (2021) Prescribed walking for glycemic control and symptom management in patients without diabetes undergoing chemotherapy. Nurs Res 70(1):6–14
Yang S, Chu S, Gao Y, Ai Q, Liu Y, Li X, Chen N 2019 A narrative review of cancer-related fatigue (CRF) and its possible pathogenesis. Cells, 8(7).
Dieli-Conwright CM, Wong L, Waliany S, Bernstein L, Salehian B, Mortimer JE (2016) An observational study to examine changes in metabolic syndrome components in patients with breast cancer receiving neoadjuvant or adjuvant chemotherapy. Cancer 122(17):2646–2653
Calip GS, Hubbard RA, Stergachis A, Malone KE, Gralow JR, Boudreau DM (2015) Adherence to oral diabetes medications and glycemic control during and following breast cancer treatment. Pharmacoepidemiol Drug Saf 24(1):75–85
Tan X, Feng X, Chang J, Higa G, Wang L, Leslie D (2016) Oral antidiabetic drug use and associated health outcomes in cancer patients. J Clin Pharm Ther 41(5):524–531
Samuel SM, Varghese E, Varghese S, Busselberg D (2018) Challenges and perspectives in the treatment of diabetes associated breast cancer. Cancer Treat Rev 70:98–111
Evans JMM, Donnelly LA, Emslie-Smoth AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients. BMJ 330(7503):1304–1305
Sullivan PW, Morrato EH, Ghushcyan V, Wyatt HR, Hill JO (2005) Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S 2000–2002. Diabetes Care 28(7):1599–1603
Servaes P, Verhagen C, Bleijenberg G (2002) Fatigue in cancer patients during and after treatment:prevalence, correlates and interventions. Eur J Cancer 38:27–43
Prentice AM, Jebb SA (2001) Beyond body mass index. Obes Rev 2:141–147
Acknowledgements
We would like to thank the following National Cancer Institute (NCI) Community Oncology Research Program (NCORP) affiliate sites who participated in this study: Central Illinois, Columbus, Cancer Research Consortium of West Michigan, Dayton, Delaware, Grand Rapids, Greenville, Hematology-Oncology Associates of Central New York, Kalamazoo, Kansas City, Marshfield, Metro Minnesota, Nevada, North Shore, Pacific Cancer Research Consortium, Southeast Cancer Control Consortium, Southeast Clinical Oncology Research Consortium, Upstate Carolina, Virginia Mason, Wichita, Wisconsin NCORP, and Western Oncology Research Consortium.
Funding
This research was supported by the National Institutes of Health (NIH) NCI grants UG1CA189961 to KMM and Gary Morrow, T32CA102618 to MCJ and Gary Morrow, R01CA231014 to MCJ, and K07CA221931 to IRK. This publication was supported by funds through the Maryland Department of Health’s Cigarette Restitution Fund Program.
Author information
Authors and Affiliations
Contributions
MCJ led the parent study. KMM, LJP, AAO, JOH, and HG contributed to the design of the parent study. ASK conceived the idea for this analysis. ASK, IRK, EC, and MCJ designed and conducted the analysis. EC and ASK performed the statistical analysis. ASK wrote the initial draft of the manuscript. All authors edited the manuscript and read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Ethical approval was obtained from Institutional Review Boards at University of Rochester Cancer Center and each of the 22 recruitment sites prior to enrollment. This trial was performed in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
All individual participants included in the study provided informed consent.
Consent for publication
N/A
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The results of this study were presented as an oral presentation at the 2021 Multinational Association of Supportive Care in Cancer Annual meeting, with a Young Investigator Award to AK.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kleckner, A.S., Kleckner, I.R., Culakova, E. et al. The association between cancer-related fatigue and diabetes from pre-chemotherapy to 6 months post-chemotherapy. Support Care Cancer 30, 7655–7663 (2022). https://doi.org/10.1007/s00520-022-07189-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07189-x