Abstract
Purpose
Oesophageal squamous cell carcinoma (ESCC) patients have severe symptom burden after oesophagectomy; however, longitudinal studies of symptom recovery after surgery are scarce. This study used longitudinal patient-reported outcome (PRO)-based symptoms to identify severe symptoms and profile symptom recovery from surgery in patients undergoing oesophagectomy.
Methods
Oesophageal cancer patients (N = 327) underwent oesophagectomy were consecutively included between April 2019 and March 2020. Data were extracted from the Sichuan Cancer Hospital’s Esophageal Cancer Case Management Registration Database. Symptom assessment time points were pre-surgery and 1, 3, 5, 7, 14, 21, 30, and 90 days post-surgery using the Chinese version of the MD Anderson Symptom Inventory. And each symptom was rated on an 11-point scale, with 0 being ‘not present’ and 10 being ‘as bad as you can imagine’. The symptom recovery trajectories were profiled using mixed effect models and Kaplan–Meier analysis.
Results
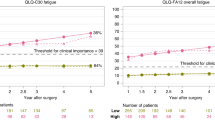
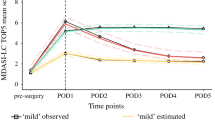
The most-severe symptoms on day 1 after oesophagectomy were pain, fatigue, dry mouth, disturbed sleep, and distress. The severity of symptoms peaked on day 1 after surgery. The top two symptoms were fatigue (mean: 5.44 [SD 1.88]) and pain (mean: 5.23 [SD 1.29]). Fatigue was more severe 90 days after surgery than at baseline (mean: 1.77 [SD 1.47] vs 0.65 [SD 1.05]; P < .0001). Disturbed sleep and distress persisted from pre-surgery to 90 days post-surgery; average sleep recovery time was up to 20 days, and 50.58% of patients had sleep disturbances 90 days post-surgery.
Conclusions
Early post-operative pain management after oesophagectomy should be considered. Characteristics and intervention strategies of post-operative fatigue, distress, and disturbed sleep in oesophageal cancer patients warrant further studies.




Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code availability
Data were analysed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. C.A. Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Chen W, Zheng R, Baade PD et al (2016) Cancer statistics in China, 2015. C.A. Cancer J Clin 66:115–132. https://doi.org/10.3322/caac.21338
Zeng HM, Chen WQ, Zheng RS et al (2018) Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 6:e555–e567. https://doi.org/10.1016/S2214-109X(18)30127-X
Viklund P, Lindblad M, Lu M, Ye W, Johansson J, Lagergren J (2006) Risk factors for complications after esophageal cancer resection: a prospective population-based study in Sweden. Ann Surg 243(2):204–211. https://doi.org/10.1097/01.sla.0000197698.17794.eb
Kauppila JH, Johar A, Lagergren P (2020) Medical and surgical complications and health-related quality of life after esophageal cancer surgery. Ann Surg 271:502–508. https://doi.org/10.1097/SLA.0000000000003097
Kauppila JH, Johar A, Lagergren P (2020) Postoperative complications and health-related quality of life 10 years after esophageal cancer surgery. Ann Surg 271:311–316. https://doi.org/10.1097/SLA.0000000000002972
Schandl A, Lagergren J, Johar A, Lagergren P (2016) Health-related quality of life 10 years after esophageal cancer surgery. Eur J Cancer 69:43–50. https://doi.org/10.1016/j.ejca.2016.09.032
Guo M, Wang C, Yin X, Nie L, Wang G (2019) Symptom clusters and related factors in oesophageal cancer patients 3 months after surgery. J Clin Nurs 28:3441–3450. https://doi.org/10.1111/jocn.14935
Quinten C, Martinelli F, Coens C et al (2014) A global analysis of multitrial data investigating quality of life and symptoms as prognostic factors for survival in different tumor sites. Cancer 120(2):302–311. https://doi.org/10.1002/cncr.28382
Derogar M, Orsini N, Sadr-Azodi O, Lagergren P (2012) Influence of major postoperative complications on health-related quality of life among long-term survivors of esophageal cancer surgery. J Clin Oncol 30(14):1615–1619. https://doi.org/10.1200/JCO.2011.40.3568
Ha S, Kim K, Kim J (2016) The influence of symptoms on quality of life among patients who have undergone oesophageal cancer surgery. Eur J Oncol Nurs 24:13–19. https://doi.org/10.1016/j.ejon.2016.08.002
Wikman A, Johar A, Lagergren P (2014) Presence of symptom clusters in surgically treated patients with esophageal cancer: implications for survival. Cancer 120:286–293. https://doi.org/10.1002/cncr.28308
Phillips JD (2020) SL Wong, Patient-reported outcomes in surgical oncology: an overview of instruments and scores. Ann Surg Oncol 27(1):45–53. https://doi.org/10.1245/s10434-019-07752-7
Basch E (2018) Patient-reported outcomes: an essential component of oncology drug development and regulatory review. Lancet Oncol 19:595–597. https://doi.org/10.1016/S1470-2045(18)30141-4
Aahlin EK, von Meyenfeldt M, Dejong CH et al (2014) Functional recovery is considered the most important target: a survey of dedicated professionals. Perioper Med (Lond) 3:5. https://doi.org/10.1186/2047-0525-3-5
Avery K, Chalmers K, Brookes S et al (2018) Development of a core outcome set for clinical effectiveness trials in esophageal cancer resection surgery. Ann Surg 267(4):700–710. https://doi.org/10.1097/SLA.0000000000002204
Maas K, Cuesta M, Van Berge HM et al (2015) Quality of life and late complications after minimally invasive compared to open esophagectomy: results of a randomized trial. World J Surg 39(8):1986–1993. https://doi.org/10.1007/s00268-015-3100-y
van der Schaaf M (2013) M Rutegård, and P Lagergren, The influence of surgical factors on persisting symptoms 3 years after esophageal cancer surgery: a population-based study in Sweden. Ann Surg Oncol 20(5):1639–1645. https://doi.org/10.1245/s10434-012-2690-y
Derogar M, Lagergren P (2012) Health-related quality of life among 5-year survivors of esophageal cancer surgery: a prospective population-based study. J Clin Oncol 30(4):413–418. https://doi.org/10.1200/JCO.2011.38.9791
Viklund P, Wengström Y, Rouvelas I, Lindblad M, Lagergren J (2006) Quality of life and persisting symptoms after oesophageal cancer surgery. Eur J Cancer 42(10):1407–1414. https://doi.org/10.1016/j.ejca.2006.02.005
Qiuling S, Shelley WX, Mendoza Tito R, Pandya Kishan J, Cleeland Charles S (2009) Assessing persistent cancer pain: a comparison of current pain ratings and pain recalled from the past week. J Pain Symptom Manage 37(2):168–174. https://doi.org/10.1016/j.jpainsymman.2008.02.009
Shi Q, Trask PC, Wang XS et al (2010) Does recall period have an effect on cancer patients’ ratings of the severity of multiple symptoms? J Pain Symptom Manag 40(2):191–199. https://doi.org/10.1016/j.jpainsymman.2009.12.010
Chang VT, Hwang SS, Feuerman M (2000) Validation of the Edmonton Symptom Assessment Scale. Cancer 88(9):2164–2171. https://doi.org/10.1002/(SICI)1097-0142(20000501)88:9<2164::AID-CNCR24>3.0.CO2-5
Fagundes CP, Shi Q, Vaporciyan AA et al (2015) Symptom recovery after thoracic surgery: measuring patient-reported outcomes with the MD Anderson Symptom Inventory. J Thorac Cardiovasc Surg 150:613–619. https://doi.org/10.1016/j.jtcvs.2015.05.057
Cleeland CS, Mendoza TR, Wang XS et al (2000) Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 89:1634–1646. https://doi.org/10.1002/1097-0142(20001001)89:7<1634::aid-cncr29>3.0.co;2-v
Hao Xi-Shan, Wang Ying, Kuo Hong, Cleeland Charles S, Wang Xin Shelly, Mendoza Tito R (2004) Chinese version of the M.D. Anderson Symptom Inventory. Validation and application of symptom measurement in cancer patients. Cancer 101(8):1890. https://doi.org/10.1002/cncr.20448
Gjeilo KH, Oksholm T, Follestad T et al (2020) Trajectories of pain in patients undergoing lung cancer surgery: a longitudinal prospective study. J Pain Symptom Manag 59(4):818-828.e1. https://doi.org/10.1016/j.jpainsymman.2019.11.004+
Visser E, Marsman M, van Rossum PSN et al (2017) Postoperative pain management after esophagectomy: a systematic review and meta-analysis. Dis Esophagus 30:1–11. https://doi.org/10.1093/dote/dox052
Bayman EO, Parekh KR, Keech J, Selte A, Brennan TJ (2017) A prospective study of chronic pain after thoracic surgery. Anesthesiology 126:938–951. https://doi.org/10.1097/ALN.0000000000001576
Sarkaria IS, Rizk NP, Goldman DA et al (2019) Early quality of life outcomes after robotic-assisted minimally invasive and open esophagectomy. Ann Thorac Surg 108:920–928. https://doi.org/10.1016/j.athoracsur.2018.11.075
Caumo W, Levandovsk R, Hidalgo M (2009) Preoperative anxiolytic effect of melatonin and clonidine on postoperative pain and morphine consumption in patients undergoing abdominal hysterectomy: a double-blind, randomized, placebo-controlled study. J Pain 10(1):100–108. https://doi.org/10.1016/j.jpain.2008.08.007
Parameswaran R, Titcomb DR, Blencowe NS et al (2013) Assessment and comparison of recovery after open and minimally invasive esophagectomy for cancer: an exploratory study in two centers. Ann Surg Oncol 20(6):1970–1977. https://doi.org/10.1245/s10434-012-2848-7
Pritlove C, Capone G, Kita H, Gladman S, Maganti M, Jones JM (2020) Cooking for vitality: pilot study of an innovative culinary nutrition intervention for cancer-related fatigue in cancer survivors. Nutrients 12.https://doi.org/10.3390/nu12092760
Baguley BJ, Bolam KA, Wright ORL, Skinner TL (2017) The effect of nutrition therapy and exercise on cancer-related fatigue and quality of life in men with prostate cancer: asystematic review. Nutrients 9.https://doi.org/10.3390/nu9091003
Inglis JE, Lin PJ, Kerns SL et al (2019) Nutritional interventions for treating cancer-related fatigue: a qualitative review. Nutr Cancer 71:21–40. https://doi.org/10.1080/01635581.2018.1513046
Bower JE (2014) Cancer-related fatigue–mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 11:597–609. https://doi.org/10.1038/nrclinonc.2014.127
Kauppila JH, Xie S, Johar A, Markar SR, Lagergren P (2017) Meta-analysis of health-related quality of life after minimally invasive versus open esophagectomy for esophageal cancer. Br J Surg 104:1131–1140. https://doi.org/10.1002/bjs.10577
Pearson EJM, Morris ME, di Stefano M, McKinstry CE (2018) Interventions for cancer-related fatigue: a scoping review. Eur J Cancer Care (Engl) 27.https://doi.org/10.1111/ecc.12516
Hilfiker R, Meichtry A, Eicher M et al (2018) Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br J Sports Med 52:651–658. https://doi.org/10.1136/bjsports-2016-096422
Mustian KM, Alfano CM, Heckler C et al (2017) Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. JAMA Oncol 3:961–968. https://doi.org/10.1001/jamaoncol.2016.6914
Gonzalez BD, Eisel SL, Qin B et al (2020) Prevalence, risk factors, and trajectories of sleep disturbance in a cohort of African-American breast cancer survivors. Support Care Cancer 29(5):2761–2770. https://doi.org/10.1007/s00520-020-05786-2
Pinto E, Cavallin F, Scarpa M (2019) Psychological support of esophageal cancer patient? J Thorac Dis 11:S654–S662. https://doi.org/10.21037/jtd.2019.02.34
Papadopoulos D, Kiagia M, Charpidou A, Gkiozos I, Syrigos K (2019) Psychological correlates of sleep quality in lung cancer patients under chemotherapy: a single-center cross-sectional study. Psychooncology 28:1879–1886. https://doi.org/10.1002/pon.5167
Graef DM, Crabtree VM, Srivastava DK et al (2018) Sleep and mood during hospitalization for high-dose chemotherapy and hematopoietic rescue in pediatric medulloblastoma. Psychooncology 27:1847–1853. https://doi.org/10.1002/pon.4737
Kukreja JB, Shi Q, Chang CM et al (2018) Patient-reported outcomes are associated with enhanced recovery status in patients with bladder cancer undergoing radical cystectomy[J]. Surg Innov 25(3):242–250. https://doi.org/10.1177/1553350618764218
Acknowledgements
The authors wish to thank all the participating patients and Wei Xu for her efforts in the statistical graph edit.
Funding
This work was supported by the Sichuan Science and Technology Program (grant numbers 2020YFH0169) and Nursing Research Project of Sichuan Province (grant numbers H20007).
Author information
Authors and Affiliations
Contributions
Conceptualisation: Qiuling Shi; formal analysis and investigation: Xi Luo, Qin Xie, Yan Miao, Hong Yin, Qingsong Yu, Hongfan Yu; writing — original draft preparation: Xi Luo; writing — review and editing: Qiuling Shi, Xi Luo; funding acquisition: Xuefeng Leng, Hong Zhou; resources: Yongtao Han, Hong Zhou; supervision: Hong Zhou.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Medical Ethics Committee and Clinical Trial Review Committee of the Sichuan Cancer Hospital (SCCHEC-02–2020-036).
Consent to participate
As this was a retrospective review of de-identified data, the requirement for informed consent was waived.
Consent for publication
Not applicable.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The Chinese version of the MD Anderson Symptom Inventory is copyrighted and licensed by the University of Texas MD Anderson Cancer Center. The authors report no other conflicts of interest in this work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was registered on ChiCTR.org.cn Web site (ChiCTR2000040780 Date 12/10/2020).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Luo, X., Xie, Q., Shi, Q. et al. Profiling patient-reported symptom recovery from oesophagectomy for patients with oesophageal squamous cell carcinoma: a real-world longitudinal study. Support Care Cancer 30, 2661–2670 (2022). https://doi.org/10.1007/s00520-021-06711-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06711-x