Abstract
Purpose
The present study aimed to investigate the status and significantly influencing factors of treatment and prognosis perceptions among advanced cancer patients based on patient-reported outcome.
Methods
A cross-sectional study was conducted at two tertiary A general hospitals. From June to September 2019, 300 patients were invited and 292 of them participated in this study. Except for 9 invalid questionnaires, 283 pen-paper questionnaires including sociodemographic and clinical characteristics, Chinese Version of Prognosis and Treatment Perception Questionnaire, Herth Hope Index, and Hospital Anxiety and Depression Scale were well completed. Descriptive analysis, Pearson’s correlation test, logistic regression analysis, and multiple linear regression analysis were applied for analysis.
Results
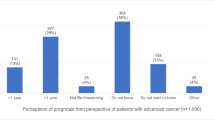
One hundred seventy-five (61.8%) advanced cancer patients reported inaccurate treatment perception. Prognosis perception scored 87.9 ± 13.72 indicating a middle level of prognosis perception. Fourteen (4.9%), 138 (48.8%), and 131 (46.3%) patients presented low, middle, and high prognosis perception levels, respectively. In patients, without spouse and religion beliefs, received chemoradiotherapy, diagnosed as cancer equal to or less than 1 year, and higher hope level were inaccurate treatment perception’s risk factors. Younger age, longer diagnosis time, higher educational level, less support for medical expenses payment, receiving chemoradiotherapy, and lower hope level but more anxiety and depression symptoms were positive predictors of prognosis perception.
Conclusions
A majority of advanced cancer patients in this study reported inaccurate treatment and middle level of prognosis perception influencing by objective and subjective factors. Clinical interventions could be developed referring these impacting factors originating from patient-reported outcome.

Similar content being viewed by others
Data and materials availability
All authors declared that all data and materials as well as software application or custom code support their published claims and comply with field standards.
Code availability
Not applicable.
References
Diamond EL, Prigerson HG, Correa DC, Reiner A, Panageas K, Kryza-Lacombe M, Buthorn J, Neil EC, Miller AM, DeAngelis LM, Applebaum AJ (2017) Prognostic awareness, prognostic communication, and cognitive function in patients with malignant glioma. Neuro Oncol 19(11):1532–1541. https://doi.org/10.1093/neuonc/nox117
Applebaum AJ, Kolva EA, Kulikowski JR, Jacobs JD, DeRosa A, Lichtenthal WG, Olden ME, Rosenfeld B, Breitbart W (2014) Conceptualizing prognostic awareness in advanced cancer: a systematic review. J Health Psychol 19(9):1103–1119. https://doi.org/10.1177/1359105313484782
Nipp RD, Greer JA, El-Jawahri A, Moran SM, Traeger L, Jacobs JM, Jacobsen JC, Gallagher ER, Park ER, Ryan DP, Jackson VA, Pirl WF, Temel JS (2017) Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol 35(22):2551–2557. https://doi.org/10.1200/JCO.2016.71.3404
Yennurajalingam S, Rodrigues LF, Shamieh O, Tricou C, Filbet M, Naing K, Ramaswamy A, Perez-Cruz PE, Bautista MJS, Bunge S, Muckaden MA, Sewram V, Fakrooden S, Noguera-Tejedor A, Rao SS, Liu D, Park M, Williams JL, Lu Z, Cantu H, Hui D, Reddy SK, Bruera E (2018) Perception of curability among advanced cancer patients: an international collaborative study. Oncologist 23(4):501–506. https://doi.org/10.1634/theoncologist.2017-0264
Fischer IC, Cripe LD, Rand KL (2018) Predicting symptoms of anxiety and depression in patients living with advanced cancer: the differential roles of hope and optimism. Support Care Cancer 26(10):3471–3477. https://doi.org/10.1007/s00520-018-4215-0
Enzinger AC, Zhang B, Schrag D, Prigerson HG (2015) Outcomes of prognostic disclosure: associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol 33(32):3809–3816. https://doi.org/10.1200/jco.2015.61.9239
Zafar W, Hafeez H, Jamshed A, Shah MA, Quader A, Yusuf MA (2016) Preferences regarding disclosure of prognosis and end-of-life care: a survey of cancer patients with advanced disease in a lower-middle-income country. Palliat Med 30(7):661–673. https://doi.org/10.1177/0269216315625810
Jeevanandan N, Nøhr C (2020) Patient-generated health data in the clinic. Stud Health Technol Inform 270:766–770. https://doi.org/10.3233/SHTI200264
Mierzynska J, Piccinin C, Pe M, Martinelli F, Gotay C, Coens C, Mauer M, Eggermont A, Groenvold M, Bjordal K, Reijneveld J, Velikova G, Bottomley A (2019) Prognostic value of patient-reported outcomes from international randomised clinical trials on cancer: a systematic review. Lancet Oncol 20(12):e685–e698. https://doi.org/10.1016/s1470-2045(19)30656-4
LeBlanc TW, Abernethy AP (2017) Patient-reported outcomes in cancer care - hearing the patient voice at greater volume. Nat Rev Clin Oncol 14(12):763–772. https://doi.org/10.1038/nrclinonc.2017.153
Yang LY, Manhas DS, Howard AF, Olson RA (2018) Patient-reported outcome use in oncology: a systematic review of the impact on patient-clinician communication. Support Care Cancer 26(1):41–60. https://doi.org/10.1007/s00520-017-3865-7
Kotronoulas G, Kearney N, Maguire R, Harrow A, Di Domenico D, Croy S, MacGillivray S (2014) What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol 32(14):1480–1501. https://doi.org/10.1200/JCO.2013.53.5948
Huang X, Zhang TZ, Li GH, Liu L, Xu GQ (2020) Prevalence and correlation of anxiety and depression on the prognosis of postoperative non-small-cell lung cancer patients in North China. Medicine 99(11):e19087. https://doi.org/10.1097/md.0000000000019087
Stark DPH, House A (2000) Anxiety in cancer patients. Br J Cancer 83(10):1261–1267. https://doi.org/10.1054/bjoc.2000.1405
Ghoneim MM, O’Hara MW (2016) Depression and postoperative complications: an overview. BMC Surg 16:5. https://doi.org/10.1186/s12893-016-0120-y
Pitman A, Suleman S, Hyde N, Hodgkiss A (2018) Depression and anxiety in patients with cancer. BMJ (Clin Res Ed) 361:k1415. https://doi.org/10.1136/bmj.k1415
Grossoehme DH, Friebert S, Baker JN, Tweddle M, Needle J, Chrastek J, Thompkins J, Wang J, Cheng YI, Lyon ME (2020) Association of religious and spiritual factors with patient-reported outcomes of anxiety, depressive symptoms, fatigue, and pain interference among adolescents and young adults with cancer. JAMA Netw Open 3(6):e206696. https://doi.org/10.1001/jamanetworkopen.2020.6696
Baczewska B, Block B, Kropornicka B, Niedzielski A, Malm M, Zwolak A, Makara-Studzińska M (2019) Hope in hospitalized patients with terminal cancer. Int J Environ Res Public Health 16(20):3867. https://doi.org/10.3390/ijerph16203867
Herth K (1991) Development and refinement of an instrument to measure hope. Sch Inq Nurs Pract 5(1):39–56. https://doi.org/10.1056/NEJM200012143432405
Costa DT, Silva DMRD, Cavalcanti IDL, Gomes ET, Vasconcelos JLA, Carvalho MVG (2019) Religious/spiritual coping and level of hope in patients with cancer in chemotherapy. Rev Bras Enferm 72(3):640–645. https://doi.org/10.1590/0034-7167-2018-0358
Amati M, Grignoli N, Rubinelli S, Amann J, Zanini C (2019) The role of hope for health professionals in rehabilitation: a qualitative study on unfavorable prognosis communication. PLoS ONE 14(10):e0224394. https://doi.org/10.1371/journal.pone.0224394
Tu PC, Yeh DC, Hsieh HC (2020) Positive psychological changes after breast cancer diagnosis and treatment: the role of trait resilience and coping styles. J Psychosoc Oncol 38(2):156–170. https://doi.org/10.1080/07347332.2019.1649337
Chow SC, Shao J, Wang H, Lokhnygina Y (2017) Sample size calculations in clinical research. CRC Press, New York
Yin XM, Jiang YY, Tang YY, Zhang YL, Zhao YL, Liu QW, Zhu XL (2020) Reliability and validity of the Chinese version of the Prognosis and Treatment Perception Questionnaire (In Chinese). Chin Nurs Manag 20(1):38–43. https://doi.org/10.3969/j.issn.1672-1756.2020.01.009
El-Jawahri A, Traeger L, Park ER, Greer JA, Pirl WF, Lennes IT, Jackson VA, Gallagher ER, Temel JS (2014) Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer 120(2):278–285. https://doi.org/10.1002/cncr.28369
Nipp RD, El-Jawahri A, Fishbein JN, Gallagher ER, Stagl JM, Park ER, Jackson VA, Pirl WF, Greer JA, Temel JS (2016) Factors associated with depression and anxiety symptoms in family caregivers of patients with incurable cancer. Ann Oncol 27(8):1607–1612. https://doi.org/10.1093/annonc/mdw205
Tang ST, Chen CH, Wen FH, Chen JS, Chang WC, Hsieh CH, Chou WC, Hou MM (2018) Accurate prognostic awareness facilitates, whereas better quality of life and more anxiety symptoms hinder end-of-life care discussions: a longitudinal survey study in terminally ill cancer patients’ last six months of life. J Pain Symptom Manage 55(4):1068–1076. https://doi.org/10.1016/j.jpainsymman.2017.12.485
Herth K (1992) Abbreviated instrument to measure hope: development and psychometric evaluation. J Adv Nurs 17(10):1251–1259. https://doi.org/10.1111/j.1365-2648.1992.tb01843.x
Zhao HP, Wang J (2000) Social support and hope of hemodialysis patients (In Chinese). Chin J Nurs 35(5):306–308. http://d.wanfangdata.com.cn/periodical/zhhlzz200005024. Accessed 20 Aug 2007
An N, Ye JJ, Huang QY (2016) Correlation between levels of hope and coping styles of oral cancer patients after surgery (In Chinese). Family Nursing 14(4):331–334. https://doi.org/10.3969/j.issn.1674-4748.2016.04.003
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Sun ZX, Liu HX LY, Zhou JT, Yang LN, Fan JY (2017) Reliability and validity of hospital anxiety and depression scale (In Chinese). Chin J Clin (Electron Ed) 11(2):198-201.https://doi.org/10.3877/cma.j.issn.1674-0785.2017.02.005
Kim JH (2019) Multicollinearity and misleading statistical results. Korean J Anesthesiol 72(6):558–569. https://doi.org/10.4097/kja.19087
Traa MJ, De Vries J, Bodenmann G, Den Oudsten BL (2015) Dyadic coping and relationship functioning in couples coping with cancer: a systematic review. Br J Health Psychol 20(1):85–114. https://doi.org/10.1111/bjhp.12094
Bowie JV, Bell CN, Ewing A, Kinlock B, Ezema A, Thorpe RJ, LaVeist TA (2017) Religious coping and types and sources of information used in making prostate cancer treatment decisions. Am J Men’s Health 11(4):1237–1246. https://doi.org/10.1177/1557988317690977
Palmer Kelly E, Meara A, Hyer M, Payne N, Pawlik TM (2019) Understanding the type of support offered within the caregiver, family, and spiritual/religious contexts of cancer patients. J Pain Symptom Manage 58(1):56–64. https://doi.org/10.1016/j.jpainsymman.2019.03.003
Kim JW, Choi JY, Jang WJ, Choi YJ, Choi YS, Shin SW, Kim YH, Park KH (2019) Completion rate of physician orders for life-sustaining treatment for patients with metastatic or recurrent cancer: a preliminary, cross-sectional study. BMC Palliat Care 18(1):84. https://doi.org/10.1186/s12904-019-0475-9
Sisk BA, Fasciano K, Block SD, Mack JW (2020) Longitudinal prognostic communication needs of adolescents and young adults with cancer. Cancer 126(2):400–407. https://doi.org/10.1002/cncr.32533
Loh KP, Mohile SG, Lund JL, Epstein R, Lei L, Culakova E, McHugh C, Wells M, Gilmore N, Mohamed MR, Kamen C, Aarne V, Conlin A, Bearden J, Onitilo A, Wittink M, Dale W, Hurria A, Duberstein P (2019) Beliefs about advanced cancer curability in older patients, their caregivers, and oncologists. Oncologist 24(6):e292–e302. https://doi.org/10.1634/theoncologist.2018-0890
Smith GL, Lopez-Olivo MA, Advani PG, Ning MS, Geng Y, Giordano SH, Volk RJ (2019) Financial burdens of cancer treatment: a systematic review of risk factors and outcomes. J Natl Compr Cancer Network: JNCCN 17(10):1184–1192. https://doi.org/10.6004/jnccn.2019.7305
Young AL, Lee E, Absolom K, Baxter H, Christophi C, Lodge JPA, Glaser AG, Toogood GJ (2018) Expectations of outcomes in patients with colorectal cancer. BJS Open 2(5):285–292. https://doi.org/10.1002/bjs5.73
Valikodath NG, Newman-Casey PA, Lee PP, Musch DC, Niziol LM, Woodward MA (2017) Agreement of ocular symptom reporting between patient-reported outcomes and medical records. JAMA Ophthalmol 135(3):225–231. https://doi.org/10.1001/jamaophthalmol.2016.5551
Soylu C, Babacan T, Sever AR, Altundag K (2016) Patients’ understanding of treatment goals and disease course and their relationship with optimism, hope, and quality of life: a preliminary study among advanced breast cancer outpatients before receiving palliative treatment. Support Care Cancer 24(8):3481–3488. https://doi.org/10.1007/s00520-016-3182-6
Wu X, Xu H, Zhang X, Han S, Ge L, Li X, Zhang X (2021) Self-efficacy, hope as mediators between positive coping and resilience among patients with gastric cancer before the first chemotherapy. Cancer Nurs 44(1):79–85. https://doi.org/10.1097/ncc.0000000000000753
Ellis EM, Varner A (2018) Unpacking cancer patients’ preferences for information about their care. J Psychosoc Oncol 36(1):1–18. https://doi.org/10.1080/07347332.2017.1357666
Kendig S, Keats JP, Hoffman MC, Kay LB, Miller ES, Moore Simas TA, Frieder A, Hackley B, Indman P, Raines C, Semenuk K, Wisner KL, Lemieux LA (2017) Consensus bundle on maternal mental health: perinatal depression and anxiety. Obstet Gynecol 129(3):422–430. https://doi.org/10.1097/aog.0000000000001902
Funding
The study was funded by the Project of Research Planning Foundation on Humanities and Social Sciences of the Ministry of Education (no. 20YJAZH144).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Study design and material preparation were performed by Bo Hu, Xiaomeng Yin, and Jizhe Wang. Data collection and analysis were performed by Bo Hu, Xiaomeng Yin, Nuan Wang, Hui Zhu, Zhanjun Gao, Xiuli Zhu, and Jizhe Wang. The first draft of the manuscript was written by Bo Hu, Xiaomeng Yin, and Jizhe Wang and all authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted according to the Declaration of Helsinki and was supported by the ethical committee of the university which the researchers affiliated.
Consent to participate
Before distributing the questionnaires, all the patients signed the informed consents. And they indicated that they understood the nature and purpose of the study and they knew that their personal information would not be divulged.
Consent for publication
Not applicable. Because this is not a case study, but cross-sectional study. We collect data anonymously. We present the results by analyzing a large number of quantitative data and there will be no information leakage of any participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hu, B., Yin, X., Du, C. et al. Influencing factors of treatment and prognosis perceptions among advanced cancer patients: a cross-sectional study. Support Care Cancer 30, 1209–1220 (2022). https://doi.org/10.1007/s00520-021-06516-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06516-y