Abstract
Purpose
To investigate the possible role of physical activity (PA) on sleep disturbance in breast cancer patients.
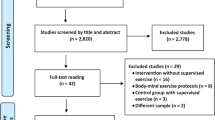
Methods
Literature in PubMed, Embase, and the Cochrane Library was systematically searched until January 30, 2020. Randomized controlled trials that focused on the role of PA interventions on sleep disturbance were selected. The main outcome measures included the global Pittsburgh Sleep Quality Index (PSQI) score and PSQI subscales. Subgroup analysis was performed based on the study area and intervention time. The stability and authenticity of the results were measured by sensitivity analysis and publication bias analysis, respectively.
Results
Six articles were included in this meta-analysis. There were no significant differences in global PSQI scores between the PA intervention group and the usual care group (P = 0.057). As for PSQI subscales, PA intervention could improve sleep quality (weighted mean difference = 0.22; 95% confidence interval 0.04–0.40; P = 0.018). There were no significant differences in sleep duration, sleep medication, sleep latency, habitual sleep efficiency, and daytime dysfunction between the two groups (all P > 0.05).
Conclusion
PA serves as an effective intervention to improve sleep quality.






Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
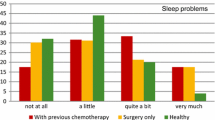
Voiss P, Höxtermann MD, Dobos G, Cramer H (2019) Cancer, sleep problems, and mind-body medicine use: results of the 2017 National Health Interview Survey. Cancer 125(24):4490–4497
Colagiuri B, Christensen S, Jensen AB, Price MA, Butow PN, Zachariae R (2011) Prevalence and predictors of sleep difficulty in a national cohort of women with primary breast cancer three to four months postsurgery. J Pain Symptom Manag 42(5):710–720
Lowery-Allison AE, Passik SD, Cribbet MR, Reinsel RA, O'Sullivan B, Norton L, Kirsh KL, Kavey NB (2018) Sleep problems in breast cancer survivors 1-10 years posttreatment. Palliat Support Care 16(3):325–334
Garland SN, Mahon K, Irwin MR (2019) Integrative approaches for sleep health in cancer survivors. Cancer J 25(5):337–342
Palesh O, Aldridge-Gerry A, Ulusakarya A, Ortiz-Tudela E, Capuron L, Innominato PF (2013) Sleep disruption in breast cancer patients and survivors. J Natl Compr Cancer Netw 11(12):1523–1530
Sternfeld B, Weltzien E, Quesenberry CP Jr, Castillo AL, Kwan M, Slattery ML, Caan BJ (2009) Physical activity and risk of recurrence and mortality in breast cancer survivors: findings from the LACE study. Cancer Epidemiol Biomark Prev 18(1):87–95
Palesh O, Kamen C, Sharp S, Golden A, Neri E, Spiegel D, Koopman C (2018) Physical activity and survival in women with advanced breast cancer. Cancer Nurs 41(4):E31–E38
Kampshoff CS, Chinapaw MJ, Brug J, Twisk JW, Schep G, Nijziel MR, van Mechelen W, Buffart LM (2015) Randomized controlled trial of the effects of high intensity and low-to-moderate intensity exercise on physical fitness and fatigue in cancer survivors: results of the Resistance and Endurance exercise After ChemoTherapy (REACT) study. BMC Med 13:275
Roveda E, Vitale JA, Bruno E, Montaruli A, Pasanisi P, Villarini A, Gargano G, Galasso L, Berrino F, Caumo A, Carandente F (2017) Protective effect of aerobic physical activity on sleep behavior in breast cancer survivors. Integr Cancer Ther 16(1):21–31
Bernard P, Ivers H, Savard MH, Savard J (2016) Temporal relationships between sleep and physical activity among breast cancer patients with insomnia. Health Psychol 35(12):1307–1315
Kreutz C, Schmidt ME, Steindorf K (2019) Effects of physical and mind-body exercise on sleep problems during and after breast cancer treatment: a systematic review and meta-analysis. Breast Cancer Res Treat 176(1):1–15
Mercier J, Savard J, Bernard P (2017) Exercise interventions to improve sleep in cancer patients: a systematic review and meta-analysis. Sleep Med Rev 36:43–56
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
de la Vega R, Tomé-Pires C, Solé E, Racine M, Castarlenas E, Jensen MP, Miró J (2015) The Pittsburgh Sleep Quality Index: validity and factor structure in young people. Psychol Assess 27(4):e22–e27
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Br Med J 339:b2535
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J (2019) Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 10:ED000142
Ghavami H, Akyolcu N (2017) The impact of lifestyle interventions in breast cancer women after completion of primary therapy: a randomized study. J Breast Health 13(2):94–99
Rogers LQ, Courneya KS, Oster RA, Anton PM, Robbs RS, Forero A, McAuley E (2017) Physical activity and sleep quality in breast cancer survivors: a randomized trial. Med Sci Sports Exerc 49(10):2009–2015
Rogers LQ, Fogleman A, Trammell R, Hopkins-Price P, Spenner A, Vicari S, Rao K, Courneya KS, Hoelzer K, Robbs R, Verhulst S (2015) Inflammation and psychosocial factors mediate exercise effects on sleep quality in breast cancer survivors: pilot randomized controlled trial. Psychooncology 24(3):302–310
Rogers LQ, Fogleman A, Trammell R, Hopkins-Price P, Vicari S, Rao K, Edson B, Verhulst S, Courneya KS, Hoelzer K (2013) Effects of a physical activity behavior change intervention on inflammation and related health outcomes in breast cancer survivors: pilot randomized trial. Integr Cancer Ther 12(4):323–335
Rogers LQ, Hopkins-Price P, Vicari S, Pamenter R, Courneya KS, Markwell S, Verhulst S, Hoelzer K, Naritoku C, Jones L, Dunnington G, Lanzotti V, Wynstra J, Shah L, Edson B, Graff A, Lowy M (2009) A randomized trial to increase physical activity in breast cancer survivors. Med Sci Sports Exerc 41(4):935–946
Wang YJ, Boehmke M, Wu YW, Dickerson SS, Fisher N (2011) Effects of a 6-week walking program on Taiwanese women newly diagnosed with early-stage breast cancer. Cancer Nurs 34(2):E1–E13
Vargas S, Wohlgemuth WK, Antoni MH, Lechner SC, Holley HA, Carver CS (2010) Sleep dysfunction and psychosocial adaptation among women undergoing treatment for non-metastatic breast cancer. Psychooncology 19(6):669–673
Reynolds GO, Otto MW, Ellis TD, Cronin-Golomb A (2016) The therapeutic potential of exercise to improve mood, cognition, and sleep in Parkinson’s disease. Mov Disord 31(1):23–38
Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A (2016) The Pittsburgh Sleep Quality Index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev 25:52–73
Grutsch JF, Wood PA, Du-Quiton J, Reynolds JL, Lis CG, Levin RD, Ann Daehler M, Gupta D, Quiton DF, Hrushesky WJ (2011) Validation of actigraphy to assess circadian organization and sleep quality in patients with advanced lung cancer. J Circadian Rhythms 9:4
Armbruster SD, Song J, Gatus L, Lu KH, Basen-Engquist KM (2018) Endometrial cancer survivors’ sleep patterns before and after a physical activity intervention: a retrospective cohort analysis. Gynecol Oncol 149(1):133–139
Henneghan AM, Carter P, Stuifbergan A, Parmelee B, Kesler S (2018) Relationships between self-reported sleep quality components and cognitive functioning in breast cancer survivors up to 10 years following chemotherapy. Psychooncology 27(8):1937–1943
Humpel N, Iverson DC (2010) Sleep quality, fatigue and physical activity following a cancer diagnosis. Eur J Cancer Care 19(6):761–768
Meneses-Echávez JF, Correa-Bautista JE, González-Jiménez E, Schmidt Río-Valle J, Elkins MR, Lobelo F, Ramírez-Vélez R (2016) The effect of exercise training on mediators of inflammation in breast cancer survivors: a systematic review with meta-analysis. Cancer Epidemiol Biomark Prev 25(7):1009–1017
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80(1):40–52
Aoyama S, Shibata S (2017) The role of circadian rhythms in muscular and osseous physiology and their regulation by nutrition and exercise. Front Neurosci 11:63
Yamanaka Y, Hashimoto S, Takasu NN, Tanahashi Y, Nishide SY, Honma S, Honma K (2015) Morning and evening physical exercise differentially regulate the autonomic nervous system during nocturnal sleep in humans. Am J Physiol Regul Integr Comp Physiol 309(9):R1112–R1121
Aritake-Okada S, Tanabe K, Mochizuki Y, Ochiai R, Hibi M, Kozuma K, Katsuragi Y, Ganeko M, Takeda N, Uchida S (2019) Diurnal repeated exercise promotes slow-wave activity and fast-sigma power during sleep with increase in body temperature: a human crossover trial. J Appl Physiol (1985) 127(1):168–177
Funding
This study was supported by the Fundamental Research Funds for the Central Universities (no. B210202175), the Hohai University Disciplinary Planning Program (no. 1013–418246) and Social Science Fund of Jiangsu Province (no. 19TYD001).
Author information
Authors and Affiliations
Contributions
Conception and design of the research: QZ and HY; acquisition of data: ZY and HP; analysis and interpretation of data: ZY and HP; statistical analysis: ZY and HP; obtained funding: QZ; drafting the manuscript: HY; and revision of the manuscript for important intellectual content: QZ. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Yang, H., Yang, Z., Pan, H. et al. Effects of physical activity on sleep problems in breast cancer survivors: a meta-analysis. Support Care Cancer 29, 4023–4032 (2021). https://doi.org/10.1007/s00520-020-05914-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05914-y