Abstract
Purpose
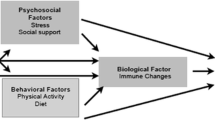
The aim of the present study was to explore clusters of psychoneurological symptoms and inflammation (levels of C-reactive protein) over time in a cohort of women with early-stage breast cancer. Specifically, we examined the relationships among affective symptoms (depression, anxiety, fatigue, sleep disturbances, pain, and perceived stress), domains of cognitive performance, and levels of peripheral C-reactive over a period of 2 years.
Methods
This was a prospective, longitudinal study of 77 women diagnosed with early-stage breast cancer. Data collection, including symptom questionnaires, performance-based cognitive testing, and blood draws, took place at 5 time points: prior to initiating adjuvant chemotherapy, prior to the fourth chemotherapy treatment, and at 6, 12, and 24 months after the initiation of chemotherapy.
Results
Exploratory factor analysis with varimax orthogonal rotation was used to examine the covariance among symptoms at each visit. Using the factor scores and weighted sums, three clusters were identified: global cognition, affective symptoms, and cognitive efficiency. Peripheral levels of C-reactive protein were inversely correlated with the cognitive efficiency factor across time.
Conclusions
The findings suggest that objectively measured domains of cognitive function occur independently of other affective symptoms that are commonly reported by women with breast cancer in long-term survivorship. The cognitive efficiency symptom cluster may be amenable to interventions targeted to biological influences that reduce levels of C-reactive protein.
Similar content being viewed by others
References
American Cancer Society (2015) Cancer facts and figures 2015. Washington, D.C.: American Cancer Society.
Jemal A, Ward E, Thun M (2010) Declining death rates reflect progress against cancer. PLoS One 5(3):e9584. doi:10.1371/journal.pone.0009584
Dodd M, Cho M, Cooper B, Miaskowski C (2010) The effect of symptom clusters on functional status and quality of life in women with breast cancer. Eur J Oncol Nurs 14(2):101–110. doi:10.1016/j.ejon.2009.09.005
Kim HJ, Barsevick AM, Fang CY, Miaskowski C (2012) Common biological pathways underlying the psychoneurological symptom cluster in cancer patients. Cancer Nurs 35(6):E1–E20. doi:10.1097/NCC.0b013e318233a811
Kim H, Barsevick AM, Tulman L, McDermott PA (2008) Treatment-related symptom clusters in breast cancer: a secondary analysis. J Pain Sympt Manag 36(5):468–479. doi:10.1016/j.jpainsymman.2007
Zhou Q, Jackson-Cook C, Lyon D, Perera R, Archer KJ (2015) Identifying molecular features associated with psychoneurological symptoms in women with breast cancer using multivariate mixed models. Cancer Inform 14(S2):139–145. doi:10.4137/CIN.S17276
Collado-Hidalgo A, Bower JE, Ganz PA, Cole SW, Irwin MR (2006) Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res 12(9):2759–2766. doi:10.1158/1078-0432.CCR-05-2398
Mehnert A, Scherwath A, Schirmer L, Schleimer B, Peterson C, Schulz-Kindermann F, Zander AR, Koch U (2007) The association between neuropsychological impairment, self-perceived cognitive deficits, fatigue and health-related quality of life in breast cancer survivors following standard adjuvant versus high-dose chemotherapy. Patient Educ Couns 66(1):108–118. doi:10.1016/j.pec.2006.11.005
Collins B, MacKenzie J, Tasca GA, Scherling C, Smith A (2014) Persistent cognitive changes in breast cancer patients 1 year following completion of chemotherapy. J Int Neuropsychol Soc 20:370–379. doi:10.1017/S1355617713001215
Myers JS (2012) Chemotherapy-related cognitive impairment: the breast cancer experience. Oncol Nurs Forum 39(1):E31–E40. doi:10.1188/12.ONF.E31-E40
Ahles TA, Root JC, Ryan EL (2012) Cancer and cancer-related treatment associated cognitive change: an update on the state of the science. J Clin Oncol 30(30):3675–3686. doi:10.1200/JCO.2012.43.0116
Wefel JS, Saleeba AK, Buzdar AU, Meyers CA (2010) Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer 116(14):3348–3356. doi:10.1002/cncr.25098
Ahles TA, Saykin AJ, McDonald B, Furstenberg CT, Cole BF, Hanscom BS, Mulrooney TJ, Schwartz GN, Kaufman PA (2008) Cognitive function in breast cancer patients prior to adjuvant treatment. Breast Cancer Res Treat 111(1):143–152
Goedendorp MM, Gielissen MF, Verhagen CA, Peters ME, Bleijenberg G (2008) Severe fatigue and related factors in cancer patients before the initiation of treatment. Br J Cancer 99(9):1408–1414. doi:10.1038/sj.bjc.6604739
Alfano CM, Imayama I, Neuhouser ML, Kiecolt-Glaser JK, Wilder Smith A, Meeske K, McTiernan A, Bernstein L, Baumgartner KB, Ulrich CM, Ballard-Barbash R (2012) Fatigue, inflammation and ω-3 and ω-6 fatty acid intake among breast cancer survivors. J Clin Oncol 30(12):1280–1287. doi:10.1200/JCO.2011.36.4109
Pomykala KL, Ganz PA, Bower JE, Kwan L, Castellon SA, Mallam S, Cheng I, Ahn R, Breen AC, Irwin MR, Silverman DHS (2013) The association between pro-inflammatory cytokines and region cerebral metabolism, and cognitive complaints following adjuvant chemotherapy for breast cancer. Brain Imaging and Behav 7:511–523. doi:10.1007/s11682-013-9243-2
Lyon DE, Cohen R, Chen H, Kelly DL, Starkweather AR, Ahn H, Jackson-Cook CK (2016) Relationship of cognitive performance to concurrent symptoms, cancer- and cancer-treatment-related variables in women with early-stage breast cancer: a 2-year longitudinal study. J Cancer Res Clin Oncol (epub ahead of print). doi:10.1007/s00432-016-2163-y
Scherling C, Collins B, Mackenzie J, Bielajew C, Smith A (2012) Prechemotherapy differences in response inhibition in breast cancer patients compared to controls: a functional magnetic resonance imaging study. J Clin Exp Neuropsychol 34(5):543–560
Noble JM, Manly JJ, Schupf N, Tang MX, Mayeux R, Luchsinger JA (2010) Association of C-reactive protein with cognitive impairment. Arch Neurol 67(1):87–92. doi:10.1001/archneurol.2009.308
Markus HS, Hunt B, Palmer K, Enzinger C, Schmidt H, Schmidt R (2005) Markers of endothelial and hemostatic activation and progression of cerebral white matter hyperintensities: longitudinal results of the Austrian Stroke Prevention Study. Stroke 36(7):1410–1414
Hoth KF, Tate DF, Poppas A, Forman DE, Gunstad J, Moser DJ, Paul RH, Jefferson AL, Haley AP, Cohen RA (2007) Endothelial function and white matter hyperintensities in older adults with cardiovascular disease. Stroke 38:308–312
Gualtieri C, Johnson L (2006) Reliability and validity of a computerized neurocognitive test battery, CNS Vital Signs. Arch Clinical Neuropsychol 21(7):623–643
Snaith RP (2003) The Hospital Anxiety and Depression Scale. Health Qual Life Outcomes 1:29
Singer S, Kuhnt S, Gotze H, Hauss J, Hinz A, Liebmann A, Kraub O, Lehmann A, Schwarz R (2009) Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. Br J Cancer 100(6):908–912. doi:10.1038/sj.bjc.6604952
Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, et al. (1999) The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer 85(5):1186–1196
Bower JE, Ganz PA, Aziz N, Fahey JL (2002) Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med 64(4):604–611
Lee KA, McEnany G, Weekes D (1999) Gender differences in sleep patterns for early adolescents. J Adolesc Health 24(1):16–20
Miaskowski C, Cooper BA, Paul SM, Dodd M, Lee K, Aouizerat BE, et al. (2006) Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Oncol Nurs Forum 33(5):E79–E89
Caraceni A (2001) Evaluation and assessment of cancer pain and cancer pain treatment. Acta Anaesthesiol Scand 45(9):1067–1075
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Social Behav 24(4):385–396
Cohen S, Williamson G (1988) Perceived stress in a probability sample of the United States. The Social Psychol Health 13:123–128
Yeh ET, Willerson JT (2003) Coming of age of C-reactive protein: using inflammation markers in cardiology. Circulation 107(3):370–371
Nudelman KN, Wang Y, McDonald BC, Conroy SK, Smith DJ, West JD, O’Neill DP, Schneider BP, Saykin AJ (2014) Altered cerebral blood flow one month after systemic chemotherapy for breast cancer: a prospective study using pulsed arterial spin labeling MRI perfusion. PLoS One 9(5):e96713. doi:10.1371/journal.pone.0096713
McDonald BC, Conroy SK, Smith DJ, West JD, Saykin AJ (2013) Frontal gray matter reduction after breast cancer chemotherapy and association with executive symptoms: a replication and extension study. Brain Behav Immun 30:S111–S125. doi:10.1016/j.bbi.2012.05.007
Jansen CE, Dodd MJ, Miaskowski CA, Dowling GA, Kramer J (2008) Preliminary results of a longitudinal study of changes in cognitive function in breast cancer patients undergoing chemotherapy with doxorubicin and cyclophosphamide. Psychooncol 17(12):1189–1195. doi:10.1002/pon.1342
Ono M, Ogilvie JM, Wilson JS, Green HJ, Chambers SK, Ownsworth T, Shum DHK (2015) A meta-analysis of cognitive impairment and decline associated with adjuvant chemotherapy in women with breast cancer. Front Oncol 5:59. doi:10.3389/fonc.2015.00059
Jansen CE, Cooper BA, Dodd MJ, Miaskowski CA (2011) A prospective longitudinal study of chemotherapy-induced cognitive changes in breast cancer patients. Support Care Cancer 19(10):1647–1656. doi:10.1007/s00520-010-0997-4
Biglia N, Bounous VE, Malabaila A, Palmisano D, Torta DM, D’Alonzo M, Sismondi P, Torta R (2012) Objective and self-reported cognitive dysfunction in breast cancer women treated with chemotherapy: a prospective study. Eur J Cancer Care 21(2):485–492. doi:10.1111/j.1365-2354.2011.01320.x
Reiner AP, Beleza S, Franceschini N, Auer PL, Robinson JG, Kooperberg C, Peters U, Tan H (2012) Genome-wide association and population genetic analysis of C-reactive protein in African American and Hispanic American women. Am J Hum Genet 91(3):502–512
Pertl MM, Hevey D, Boyle NT, Hughes MM, Collier S, O’Dwyer AM, Harkin A, Kennedy MJ, Conner TJ (2013) C-reactive protein predicts fatigue independently of depression in breast cancer patients prior to chemotherapy. Brain Behav Immun 34:108–119. doi:10.1016/j.bbi.2013.07.177
Ganz PA, Bower JE, Kwan L, Castellon SA, Silverman DH, Geist C, Breen EC, Irwin MR, Cole SW (2013) Does tumor necrosis factor-alpha (TNF-α) play a role in post-chemotherapy cerebral dysfunction? Brain Behav Immun 30:S99–108. doi:10.1016/j.bbi.2012.07.015
Yang J, Fan C, Pan L, Xie M, He Q, Li D, Wang S (2015) C-reactive protein plays a marginal role in cognitive decline: a systematic review and meta-analysis. Int J Geriatr Psychiatry 30(2):156–165. doi:10.1002/gps.4236
Marsland AL, Gianaros PJ, Kuan DC, Sheu LK, Krajina K, Manuck SB (2015) Brain morphology links systemic inflammation to cognitive function in midlife adults. Brain Behav Immun 48:195–204. doi:10.1016/j.bbi.2015.03.015
Acknowledgments
The authors would like to thank Jamie Sturgill, PhD, and Julie Stillman for their expertise in performing the assays reported in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest and source of funding
This research was supported by the National Institute of Nursing Research (Lyon/Jackson-Cook; MPI; R01 NR012667). Dr. Jackson-Cook (NIH/NIA R01AG037986) and Dr. A. Starkweather (R01 NR013932) are currently receiving grants. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research (NINR), the National Institute on Aging (NIA), or the National Institutes of Health (NIH). For the remaining authors, none were declared.
Electronic supplementary material
ESM 1
(DOCX 124 kb)
Rights and permissions
About this article
Cite this article
Starkweather, A., Kelly, D.L., Thacker, L. et al. Relationships among psychoneurological symptoms and levels of C-reactive protein over 2 years in women with early-stage breast cancer. Support Care Cancer 25, 167–176 (2017). https://doi.org/10.1007/s00520-016-3400-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3400-2