Abstract
Purpose
Although sexual concerns have been examined in breast cancer (BC), these concerns remain understudied and undertreated for patients with gastrointestinal (GI) cancer. Objectives were to: (1) assess sexual concerns in GI cancer patients compared with breast cancer patients; (2) examine whether sexual concerns are stable over time in GI and breast cancer patients; and (3) evaluate whether sexual concerns in GI and breast cancer are significantly associated with quality of life, symptom severity, and disease interference, and whether these associations change over time.
Methods
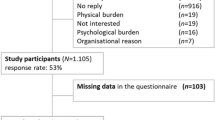
Data were collected from GI and breast cancer patients during four outpatient clinic visits over 6 months. Measures included sexual concerns (reduced sexual enjoyment, interest, or performance), quality of life (FACT-G), symptom severity, disease interference (MD Anderson Symptom Inventory), and disease-related distress (NCCN Distress Scale). Linear mixed model analyses were conducted.
Results
Sexual concerns were common in both samples, with 57% of GI cancer patients and 53% of breast cancer patients reporting at least mild sexual concerns. Sexual concerns were stable over time and were significantly associated with lower levels of functioning in multiple domains (e.g., quality of life, symptom severity, disease interference, and disease-related distress), irrespective of length of time since diagnosis. Cancer type (GI/breast cancer) was not a moderator of this relationship.
Conclusions
Self-reported sexual concerns were common, stable, and related significantly to quality of life, symptom severity, disease interference, and disease-related distress for both GI and breast cancer patients. Limitations and implications for future research are discussed.
Similar content being viewed by others
Notes
To examine the possibility that metastatic/recurrent disease state might be related to the reporting of sexual concerns, we conducted an LMM in which we estimated the effects of time, disease state (dummy coded as metastatic/recurrent disease vs. nonmetastatic/recurrent disease), and time X disease state effects in the combined GI and breast cancer dataset. Neither the effect of disease state (p = 0.68) nor the time X disease state effect was significant (p = 0.38).
In order to further examine the possible effect of gender on sexual concerns, we examined both the stability of sexual concerns over time and the relationships between sexual concerns and multiple domains of functioning in female patients only (i.e., female GI cancer patients and all breast cancer patients). We ran the identical two LMM analyses initially conducted in the mixed gender sample in which we: (1) estimated the effects of time, cancer type (GI vs. breast cancer), and the time X cancer-type interaction effect on sexual concerns and (2) estimated the effects of time, cancer type, sexual concerns, and all two- and three-way interaction terms on four domains of functioning (i.e., quality of life, symptom severity, disease-related interference, and disease-related distress). The results generally paralleled those obtained using both genders in the GI sample. For the first analysis on the outcome of sexual concerns, the time, cancer type, and time X cancer-type interaction effects were nonsignificant (all p values > 0.51). For the analyses examining the effects of time, cancer type, and sexual concerns on the domains of functioning, sexual concerns was the only significant predictor of quality of life, disease-related interference, and disease-related distress (all p values < 0.01) and these relationships did not vary over waves of assessment or by cancer type, as was found in the mixed gender sample. The effect of sexual concerns on symptom severity, however was not significant (p = 0.18).
References
Abernethy AP, Herndon JE 2nd, Wheeler JL, Patwardhan M, Shaw H, Lyerly HK, Weinfurt K (2008) Improving health care efficiency and quality using tablet personal computers to collect research-quality, patient-reported data. Health Serv Res 43:1975–1991
Alder J, Zanetti R, Wight E, Urech C, Fink N, Bitzer J (2008) Sexual dysfunction after premenopausal stage I and II breast cancer: do androgens play a role? J Sex Med 5:1898–1906
Andersen BL, Carpenter KM, Yang HC, Shapiro CL (2007) Sexual well-being among partnered women with breast cancer recurrence. J Clin Oncol 25:3151–3157
Brotto LA, Heiman JR, Goff B, Greer B, Lentz GM, Swisher E, Tamimi H, Van Blaricom A (2008) A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Arch Sex Behav 37:317–329
Burnett AL, Aus G, Canby-Hagino ED, Cookson MS, D'Amico AV, Dmochowski RR, Eton DT, Forman JD, Goldenberg SL, Hernandez J, Higano CS, Kraus S, Liebert M, Moul JW, Tangen C, Thrasher JB, Thompson I (2007) Erectile function outcome reporting after clinically localized prostate cancer treatment. J Urol 178:597–601
Canada AL, Neese LE, Sui D, Schover LR (2005) Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer 104:2689–2700
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579
Chambers SK, Schover L, Halford K, Clutton S, Ferguson M, Gordon L, Gardiner RA, Occhipinti S, Dunn J (2008) ProsCan for Couples: randomised controlled trial of a couples-based sexuality intervention for men with localised prostate cancer who receive radical prostatectomy. BMC Cancer 8:226
Chorost MI, Weber TK, Lee RJ, Rodriguez-Bigas MA, Petrelli NJ (2000) Sexual dysfunction, informed consent and multimodality therapy for rectal cancer. Am J Surg 179:271–274
Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, Engstrom MC (2000) Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 89:1634–1646
Fobair P, Stewart SL, Chang S, D'Onofrio C, Banks PJ, Bloom JR (2006) Body image and sexual problems in young women with breast cancer. Psycho-Oncology 15:579–594
Fortner B, Okon T, Schwartzberg L, Tauer K, Houts AC (2003) The cancer care monitor: psychometric content evaluation and pilot testing of a computer administered system for symptom screening and quality of life in adult cancer patients. J Pain Symptom Manage 26:1077–1092
Ganz PA, Coscarelli A, Fred C, Kahn B, Polinsky ML, Petersen L (1996) Breast cancer survivors: psychosocial concerns and quality of life. Breast Cancer Res Treat 38:183–199
Ganz PA, Kwan L, Stanton AL, Krupnick JL, Rowland JH, Meyerowitz BE, Bower JE, Belin TR (2004) Quality of life at the end of primary treatment of breast cancer: first results from the moving beyond cancer randomized trial. J Natl Cancer Inst 96:376–387
Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE (1998) Life after breast cancer: understanding women's health-related quality of life and sexual functioning. J Clin Oncol 16:501–514
Hendren SK, O'Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, Macrae HM, Gryfe R, McLeod RS (2005) Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg 242:212–223
Hoffman BM, Zevon MA, D'Arrigo MC, Cecchini TB (2004) Screening for distress in cancer patients: the NCCN rapid-screening measure. Psycho-Oncology 13:792–799
Holland J (1999) Update: NCCN practice guidelines for the management of psychosocial distress. Oncology (Williston Park) 13:459–507
Hordern AJ, Street AF (2007) Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust 186:224–227
Hordern AJ, Street AF (2007) Constructions of sexuality and intimacy after cancer: patient and health professional perspectives. Soc Sci Med 64:1704–1718
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007) Cancer statistics, 2007. CA Cancer J Clin 57:43–66
Laumann EO, Paik A, Rosen RC (1999) Sexual dysfunction in the United States: prevalence and predictors. JAMA 281:537–544
Manne S, Badr H (2008) Intimacy and relationship processes in couples' psychosocial adaptation to cancer. Cancer 112:2541–2555
Meyerowitz BE, Desmond KA, Rowland JH, Wyatt GE, Ganz PA (1999) Sexuality following breast cancer. J Sex Marital Ther 25:237–250
Raudenbush S, Bryk AS (2002) Hierarchical linear models: applications and data analysis methods. Sage, Thousand Oaks
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D'Agostino R Jr (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830
Rosenthal R (1994) Science and ethics in conducting, analyzing, and reporting psychological research. Psychol Sci 5:127–134
Schmidt CE, Bestmann B, Kuchler T, Longo WE, Kremer B (2005) Ten-year historic cohort of quality of life and sexuality in patients with rectal cancer. Dis Colon Rectum 48:483–492
Singer J, Willett JB (2003) Applied longitudinal data analysis: modeling change and event occurrence. Oxford University Press, New York
Speer JJ, Hillenberg B, Sugrue DP, Blacker C, Kresge CL, Decker VB, Zakalik D, Decker DA (2005) Study of sexual functioning determinants in breast cancer survivors. Breast J 11:440–447
Sprangers MA, te Velde A, Aaronson NK (1999) The construction and testing of the EORTC colorectal cancer-specific quality of life questionnaire module (QLQ-CR38). European Organization for Research and Treatment of Cancer Study Group on Quality of Life. Eur J Cancer 35:238–247
Acknowledgements
This study was a subanalysis of data collected through an outcomes research service agreement with Pfizer, Inc. focusing on the use of e/Tablets to collect patient-reported data in the clinic. Pfizer does not have access to individual data. SOS, Inc. served as vendor for the e/Tablets in this project; the vendor provided the hardware and programmed the software. Duke University Medical Center provided the wireless system and associated technical support. Dr. Abernethy had a nominal consulting arrangement with SOS, Inc., ending in April 2008. None of this funding or these relationships are specifically related to the topic of the manuscript, sexual concerns. This work was funded in part by the National Institutes of Health through the NIH Roadmap for Medical Research, Grant (U 5 U01 AR052186). This work was supported in part by the National Institute of Mental Health Clinical Research Training in Geriatric Mood Disorders, Grant (MH070448).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reese, J.B., Shelby, R.A., Keefe, F.J. et al. Sexual concerns in cancer patients: a comparison of GI and breast cancer patients. Support Care Cancer 18, 1179–1189 (2010). https://doi.org/10.1007/s00520-009-0738-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-009-0738-8