Summary
Background
Lymphocyte and plateletcrit (PCT) as proportions of routine complete blood count tests, have been studied as simple biomarkers for inflammatory diseases. The aim of our study was to investigate whether blood routine parameters, especially platelet parameters could be a useful tool to distinguish Adult onset Still’s disease (AOSD) from sepsis.
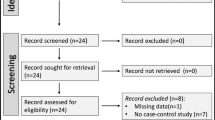
Methods
We retrospectively reviewed 58 patients with AOSD and 55 sepsis patients diagnosed at the First Affiliated Hospital of Nanjing Medical University between January, 2015 to December 2018. Laboratory data including ferritin, blood routine parameters and C‑reactive protein (CRP) level were collected, and the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte (PLR) were calculated.
Results
The results showed that AOSD patients showed higher ferritin, lymphocyte and PCT (all P < 0.01) and these factors are independent risk factors for predicting AOSD. In receiver operating characteristic (ROC) curve analysis of LY, PCT and ferritin for distinguish of AOSD, the area under the curve (AUC) was 0.676 (0.576–0.777); 0.706 (95% CI = 0.596–0.816); 0.715 (0.617–0.814). Meanwhile, the AUC of the combination of lymphocyte, PCT and ferritin was 0.836 (0.737–0.909) with sensitivity 67.3, specificity 92.3, and the difference was significant.
Conclusions
Thus we suggest that lymphocyte, PCT may be a useful tool to make a distinction between AOSD and sepsis, as supplementary biomarkers to ferritin.
Similar content being viewed by others
References
Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992;19:424–30.
Fautrel B, Zing E, Golmard JL, et al. Proposal for a new set of classification criteria for adult-onset still disease. Medicine (Baltimore). 2002;81:194–200.
Cush JJ. Adult-onset Still’s disease. Bull Rheum Dis. 2000;49:1–4.
Mitrovic S, Fautrel B. New markers for adult-onset Still’s disease. Joint Bone Spine. 2018;85:285–93.
Gerfaud-Valentin M, Maucort-Boulch D, Hot A, et al. Adult-onset still disease: manifestations, treatment, outcome, and prognostic factors in 57 patients. Medicine (Baltimore). 2014;93:91–9.
Priori R, Colafrancesco S, Alessandri C, et al. Interleukin 18: a biomarker for differential diagnosis between adult-onset Still’s disease and sepsis. J Rheumatol. 2014;41:1118–23.
Klein Klouwenberg PM, Ong DS, Bonten MJ, Cremer OL. Classification of sepsis, severe sepsis and septic shock: the impact of minor variations in data capture and definition of SIRS criteria. Intensive Care Med. 2012;38:811–9.
Lee SW, Park YB, Song JS, Lee SK. The mid-range of the adjusted level of ferritin can predict the chronic course in patients with adult onset Still’s disease. J Rheumatol. 2009;36:156–62.
Hanaganahalli SB, Sreeram S, Bompada M, Kuppannagari SK, Suresh PK, Philipose CS. Is MPV a predictive marker for neonatal sepsis? A pilot study. J Pediatr Hematol Oncol. 2018;40:548–52.
Dursun A, Ozsoylu S, Akyildiz BN. Neutrophil-to-lymphocyte ratio and mean platelet volume can be useful markers to predict sepsis in children. Pak J Med Sci. 2018;34:918–22.
Shaaban HA, Safwat N. Mean platelet volume in preterm: a predictor of early onset neonatal sepsis. J Matern Fetal Neonatal Med. 2020;33(2):206–11.
ACCP/SCCM. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Kim HA, Sung JM, Suh CH. Therapeutic responses and prognosis in adult-onset Still’s disease. Rheumatol Int. 2012;32:1291–8.
Ohta A, Yamaguchi M, Tsunematsu T, et al. Adult Still’s disease: a multicenter survey of Japanese patients. J Rheumatol. 1990;17:1058–63.
Zeng T, Zou YQ, Wu MF, Yang CD. Clinical features and prognosis of adult-onset still’s disease: 61 cases from China. J Rheumatol. 2009;36:1026–31.
Priori R, Colafrancesco S, Gattamelata A, Di Franco M, Di Tondo U, Valesini G. Adult-onset Still disease: a rare disorder with a potentially fatal outcome. Auto Immun Highlights. 2010;1:53–9.
Zhao D, Qiu G, Luo Z, Zhang Y. Platelet parameters and (1, 3)-beta-D-glucan as a diagnostic and prognostic marker of invasive fungal disease in preterm infants. PLoS One. 2015;10:e123907.
Bilgin E, Hayran M, Erden A, et al. Proposal for a simple algorithm to differentiate adult-onset Still’s disease with other fever of unknown origin causes: a longitudinal prospective study. Clin Rheumatol. 2019;38(6):1699–706.
Seo JY, Suh CH, Jung JY, Kim AR, Yang JW, Kim HA. The neutrophil-to-lymphocyte ratio could be a good diagnostic marker and predictor of relapse in patients with adult-onset Still’s disease: a STROBE-compliant retrospective observational analysis. Medicine (Baltimore). 2017;96:e7546.
Lee YH, Song GG. Neutrophil-to-lymphocyte ratio, mean platelet volume and platelet-to-lymphocyte ratio in Behcet’s disease and their correlation with disease activity: a meta-analysis. Int J Rheum Dis. 2018;21:2180–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Zhang, M. Xie, Y. Wang, J. Li, and J. Zhou declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
M. Zhang and M. Xie contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, M., Xie, M., Wang, Y. et al. Combination value of biomarkers in discriminating adult onset Still’s disease and sepsis. Wien Klin Wochenschr 133, 118–122 (2021). https://doi.org/10.1007/s00508-020-01668-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01668-z