Abstract
Background
We hypothesized that the percent change in resistance (%RΔ) from bioimpedance analysis (BIA) measurements during hemodialysis (HD) can provide information on pediatric HD patients’ hydration status.
Methods
Whole-body single-frequency BIA measurements were obtained before HD, each hour on HD, and after HD during two HD sessions. Pre-and post-HD weights, blood pressures, Crit-Line® measurements, and intradialytic symptoms were collected on the day of the BIA measurements.
Results
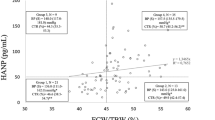
One hundred and thirty BIA measurements were obtained from 14 HD patients. The group was 43 % girls, and the mean age was 13.2 ± 4.4 years. Percent change in resistance was 13.5 ± 10.8 % at the end of HD; %RΔ correlated with percent body weight change (%BWΔ) following HD (r = −0.83, P < 0.01), as well as with percent blood volume change (%BVΔ) (r = −0.79, P < 0.01). The %RΔ was similar between patients with and without hypertension immediately before HD and was greater in those with intradialytic symptoms (19.1 ± 7.7 %) than in those without (9.9 ± 11.2 %) (P = 0.02). Patients with left ventricular hypertrophy (LVH) had lower %RΔ (7.2 ± 9.7 %) than those without (19.5 ± 7.7 %) (P = 0.03). Left ventricular mass index (LVMI) also correlated strongly with %RΔ (r = −0.79, P = 0.004) and %BWΔ (r = 0.82, P = 0.002).
Conclusions
Our study showed that %RΔ strongly correlates with %BWΔ and %BVΔ and that %RΔ also correlated with intradialytic symptoms and LVMI.




Similar content being viewed by others
References
Mitsnefes MM (2012) Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol 23:578–585
Holtta T, Happonen JM, Ronnholm K, Fyhrquist F, Holmberg C (2001) Hypertension, cardiac state, and the role of volume overload during peritoneal dialysis. Pediatr Nephrol 16:324–331
Agarwal R (2010) Hypervolemia is associated with increased mortality among hemodialysis patients. Hypertension 56:512–517
Piccoli A, Rossi B, Pillon L, Bucciante G (1994) A new method for monitoring body fluid variation by bioimpedance analysis: the RXc graph. Kidney Int 46:534–539
Kuhlmann MK, Zhu F, Seibert E, Levin NW (2005) Bioimpedance, dry weight and blood pressure control: new methods and consequences. Curr Opin Nephrol Hypertens 14:543–549
Tattersall J (2009) Bioimpedance analysis in dialysis: state of the art and what we can expect. Blood Purif 27:70–74
Piccoli A (1998) Identification of operational clues to dry weight prescription in hemodialysis using bioimpedance vector analysis. The Italian Hemodialysis-Bioelectrical Impedance Analysis (HD-BIA) Study Group. Kidney Int 53:1036–1043
Paglialonga F, Ardissino G, Galli MA, Scarfia RV, Testa S, Edefonti A (2012) Bioimpedance analysis and cardiovascular status in pediatric patients on chronic hemodialysis. Hemodial Int Suppl 1:S20–S25
Brooks ER, Fatallah-Shaykh SA, Langman CB, Wolf KM, Price HE (2008) Bioelectric impedance predicts total body water, blood pressure, and heart rate during hemodialysis in children and adolescents. J Ren Nutr 18:304–311
Di Iorio BR, Scalfi L, Terracciano V, Bellizzi V (2004) A systematic evaluation of bioelectrical impedance measurement after hemodialysis session. Kidney Int 65:2435–2440
(2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555-576
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR (2009) Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr 22:709–714
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL (2010) Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis 55:316–325
Martin LC, Franco RJ, Gavras I, Matsubara BB, Garcia S, Caramori JT, Barretti BB, Balbi AL, Barsanti R, Padovani C, Gavras H (2004) Association between hypervolemia and ventricular hypertrophy in hemodialysis patients. Am J Hypertens 17:1163–1169
Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C, Malecka-Masalska T, Marcelli D (2009) The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant 24:1574–1579
Odudu A, McIntyre C (2012) Volume is not the only key to hypertension control in dialysis patients. Nephron Clin Pract 120:c173–c177
Basile C, Vernaglione L, Di Iorio B, Bellizzi V, Chimienti D, Lomonte C, Rubino A, D’Ambrosio N (2007) Development and validation of bioimpedance analysis prediction equations for dry weight in hemodialysis patients. Clin J Am Soc Nephrol 2:675–680
Zaloszyc A, Schaefer B, Schaefer F, Krid S, Salomon R, Niaudet P, Schmitt CP, Fischbach M (2013) Hydration measurement by bioimpedance spectroscopy and blood pressure management in children on hemodialysis. Pediatr Nephrol 28:2169–2177
Matthie J, Zarowitz B, De Lorenzo A, Andreoli A, Katzarski K, Pan G, Withers P (1998) Analytic assessment of the various bioimpedance methods used to estimate body water. J Appl Physiol 84:1801–1816
Matthie JR, Withers PO (1998) Bioimpedance: 50 kHz parallel reactance and the prediction of body cell mass. Am J Clin Nutr 68:403–404
Reddan DN, Szczech LA, Hasselblad V, Lowrie EG, Lindsay RM, Himmelfarb J, Toto RD, Stivelman J, Winchester JF, Zillman LA, Califf RM, Owen WF Jr (2005) Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol 16:2162–2169
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oh, G., Wong, C., Begin, B. et al. Whole-body single-frequency bioimpedance analysis in pediatric hemodialysis patients. Pediatr Nephrol 29, 1417–1423 (2014). https://doi.org/10.1007/s00467-014-2778-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-014-2778-7