Abstract
Introduction
Standard of care for locally advanced esophageal carcinoma is neoadjuvant chemoradiation (nCRT) and surgical resection 4–8 weeks after completion of nCRT. It is recommended that the CRT to surgery interval not exceed 90 days. Many patients do not undergo surgery within this timeframe due to patient/physician preference, complete clinical response, or poor performance status. Select patients are offered salvage esophagectomy (SE), defined in two ways: resection for recurrent/persistent disease after complete response to definitive CRT (dCRT) or esophagectomy performed > 90 days after completion of nCRT. Salvage esophagectomy reportedly has higher postoperative morbidity and poor survival outcomes. In this study, we assessed outcomes, overall, and disease-free survival of patients undergoing salvage esophagectomy by both definitions (recurrent/persistent disease after dCRT and/or > 90 days), compared to planned (resection after nCRT/within 90 days) esophagectomy (PE).
Materials and methods
Retrospective review of a prospectively maintained database identified patients who underwent minimally invasive esophagectomy at a single institution from 2009 to 2019. Esophagectomy for benign disease and patients who did not receive nCRT were excluded. Outcomes included postoperative complications, length of stay (LOS), disease-free survival, and overall survival.
Results
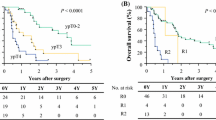
97 patients underwent minimally invasive esophageal resection for esophageal carcinoma. 89.7% of patients were male. Mean age was 64.9 years (range 36–85 years). 94.8% of patients had adenocarcinoma, with 16 transthoracic and 81 transhiatal approaches. On comparing planned esophagectomy (n = 87) to esophagectomy after dCRT failure (n = 10), no significant differences were identified in overall survival (p = 0.73), disease-free survival (p = 0.32), 30-day or major complication rate, anastomotic leak, or LOS. Similarly, when comparing esophagectomy < 90 days after CRT (n = 62) to > 90 days after CRT completion (n = 35), no significant differences were identified in overall survival (p = 0.39), disease-free survival (p = 0.71), 30-day or major complication rate, LOS, or anastomotic leak rate between groups. In this comparison, local recurrence was noted to be elevated with SE as compared to PE (64.3% vs. 25.0%, p = 0.04).
Conclusion
Overall survival and disease-free survival were equivalent between SE and PE. Local recurrence was noted to be increased with SE, though this did not appear to affect survival. Although planned esophagectomy remains the standard of care, salvage esophagectomy has comparable outcomes and is appropriate for selected patients.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2019) Cancer Statistics, 2019. CA Cancer J Clin. https://doi.org/10.3322/caac.21551
Gatta G, Mallone S, van der Zwan JM et al (2014) Cancer survival in Europe 1999–2007 by country and age: results of EUROCARE-5—a population-based study. Lancet Oncol. https://doi.org/10.1016/S1470-2045(13)70546-1
Van Hagen P, Hulshof MCCM, Van Lanschot JJB et al (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. https://doi.org/10.1056/NEJMoa1112088
Shapiro J, van Lanschot JJB, Hulshof MCCM et al (2015) Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. https://doi.org/10.1016/S1470-2045(15)00040-6
Hofstetter WL (2014) Salvage esophagectomy. J Thorac Dis. https://doi.org/10.3978/j.issn.2072-1439.2014.03.29
Sjoquist KM, Burmeister BH, Smithers BM et al (2011) Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. https://doi.org/10.1016/S1470-2045(11)70142-5
Swisher SG, Wynn P, Putnam JB et al (2002) Salvage esophagectomy for recurrent tumors after definitive chemotherapy and radiotherapy. J Thorac Cardiovasc Surg. https://doi.org/10.1067/mtc.2002.119070
Borggreve AS, van Rossum PSN, Mook S, Haj Mohammad N, van Hillegersberg R, Ruurda JP (2019) Frequency of surgical resection after starting neoadjuvant chemoradiotherapy in patients with esophageal cancer: a population-based cohort study. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2019.03.031
Bedenne L, Michel P, Bouché O et al (2007) Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol. https://doi.org/10.1200/JCO.2005.04.7118
Ma MW, Gao XS, Bin GX et al (2018) The role of definitive chemoradiotherapy versus surgery as initial treatments for potentially resectable esophageal carcinoma. World J Surg Oncol. https://doi.org/10.1186/s12957-018-1470-y
Ajani JA, Correa AM, Hofstetter WL et al (2012) Clinical parameters model for predicting pathologic complete response following preoperative chemoradiation in patients with esophageal cancer. Ann Oncol. https://doi.org/10.1093/annonc/mds210
Hodari A, Hammoud ZT, Borgi JF, Tsiouris A, Rubinfeld IS (2013) Assessment of morbidity and mortality after esophagectomy using a modified frailty index. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2013.05.051
Raymond D (2012) Complications of esophagectomy. Surg Clin North Am. https://doi.org/10.1016/j.suc.2012.07.007
Takeuchi H, Saikawa Y, Oyama T et al (2010) Factors influencing the long-term survival in patients with esophageal cancer who underwent esophagectomy after chemoradiotherapy. World J Surg. https://doi.org/10.1007/s00268-009-0331-9
Bollschweiler E, Plum P, Mönig SP, Hölscher AH (2017) Current and future treatment options for esophageal cancer in the elderly. Expert Opin Pharmacother. https://doi.org/10.1080/14656566.2017.1334764
Wakui R, Yamashita H, Okuma K et al (2010) Esophageal cancer: definitive chemoradiotherapy for elderly patients. Dis Esophagus. https://doi.org/10.1111/j.1442-2050.2010.01062.x
Cooper JS, Guo MD, Herskovic A et al (1999) Chemoradiotherapy of locally advanced. J Am Med Assoc 281(17):1623–16276
Minsky D, Pajak T, Ginsberg R et al (2014) III Trial of combined-modality therapy for esophageal therapy. J Clin Oncol
Abate E, DeMeester SR, Zehetner J et al (2010) Recurrence after esophagectomy for adenocarcinoma: defining optimal follow-up intervals and testing. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2010.01.006
Marks JL, Hofstetter W, Correa AM et al (2012) Salvage esophagectomy after failed definitive chemoradiation for esophageal adenocarcinoma. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2012.05.106
Alosi JA, Wilson JP, Yendamuri S, Dexter E (2013) Planned esophagectomy after neoadjuvant treatment versus salvage/delayed esophagectomy. Ann Surg Oncol 159(6):2555–2566
Levinsky NC, Wima K, Morris MC et al (2019) Outcome of delayed versus timely esophagectomy after chemoradiation for esophageal adenocarcinoma. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2019.09.169
Benveniste MF, Gomez D, Carter BW et al (2019) Recognizing radiation therapy– related complications in the chest. Radiographics. https://doi.org/10.1148/rg.2019180061
Nishimura M, Daiko H, Yoshida J, Nagai K (2007) Salvage esophagectomy following definitive chemoradiotherapy. Gen Thorac Cardiovasc Surg. https://doi.org/10.1007/s11748-007-0157-z
Morita M, Kumashiro R, Hisamatsu Y et al (2011) Clinical significance of salvage esophagectomy for remnant or recurrent cancer following definitive chemoradiotherapy. J Gastroenterol. https://doi.org/10.1007/s00535-011-0448-0
Takeuchi S, Ohtsu A, Doi T et al (2007) A retrospective study of definitive chemoradiotherapy for elderly patients with esophageal cancer. Am J Clin Oncol Cancer Clin Trials. https://doi.org/10.1097/COC.0b013e3180ca7c84
Gardner-Thorpe J, Hardwick RH, Dwenyhouse SJ (2007) Salvage oesophagectomy after local failure of definitive chemoradiotherapy. Br J Surg. https://doi.org/10.1002/bjs.5865
Markar SR, Karthikesalingam A, Penna M, Low DE (2014) Assessment of short-term clinical outcomes following salvage esophagectomy for the treatment of esophageal malignancy: systematic review and pooled analysis. Ann Surg Oncol. https://doi.org/10.1245/s10434-013-3364-0
Rice TW, Patil DT, Blackstone EH (2017) 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: application to clinical practice. Ann Cardiothorac Surg. https://doi.org/10.21037/acs.2017.03.14
Barreto JC, Posner MC (2010) Transhiatal versus transthoracic esophagectomy for esophageal cancer. World J Gastroenterol. https://doi.org/10.3748/wjg.v16.i30.3804
Broderick RC, Horgan S, Fuchs HF (2020) Robotic transhiatal esophagectomy. Dis Esophagus. https://doi.org/10.1093/dote/doaa037
Wei MT, Zhang YC, Deng XB, Yang TH, He YZ, Wang ZQ (2014) Transthoracic vs transhiatal surgery for cancer of the esophagogastric junction: a meta-analysis. World J Gastroenterol. https://doi.org/10.3748/wjg.v20.i29.10183
Boshier PR, Anderson O, Hanna GB (2011) Transthoracic versus transhiatal esophagectomy for the treatment of esophagogastric cancer: a meta-analysis. Ann Surg. https://doi.org/10.1097/SLA.0b013e3182263781
Vincent J, Mariette C, Pezet D et al (2015) Early surgery for failure after chemoradiation in operable thoracic oesophageal cancer. Analysis of the non-randomised patients in FFCD 9102 phase III trial: chemoradiation followed by surgery versus chemoradiation alone. Eur J Cancer. https://doi.org/10.1016/j.ejca.2015.05.027
Nakamura T, Hayashi K, Ota M et al (2004) Salvage esophagectomy after definitive chemotherapy and radiotherapy for advanced esophageal cancer. Am J Surg. https://doi.org/10.1016/j.amjsurg.2004.06.003
Delanian S, Lefaix JL (2007) Current management for late normal tissue injury: radiation-induced fibrosis and necrosis. Semin Radiat Oncol. https://doi.org/10.1016/j.semradonc.2006.11.006
Smithers BM, Cullian M, Thomas JM et al (2007) Outcomes from salvage esophagectomy post definitive chemoradiotherapy compared with resection following preoperative neoadjuvant chemoradiotherapy. Dis Esophagus. https://doi.org/10.1111/j.1442-2050.2007.00701.x
Qin Q, Xu H, Liu J et al (2018) Does timing of esophagectomy following neoadjuvant chemoradiation affect outcomes? A meta-analysis. Int J Surg. https://doi.org/10.1016/j.ijsu.2018.09.013
Juloori A, Tucker SL, Komaki R et al (2014) Influence of preoperative radiation field on postoperative leak rates in esophageal cancer patients after trimodality therapy. J Thorac Oncol. https://doi.org/10.1097/JTO.0000000000000100
Markar S, Gronnier C, Duhamel A et al (2015) The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg. https://doi.org/10.1097/SLA.0000000000001011
Andreou A, Biebl M, Dadras M et al (2016) Anastomotic leak predicts diminished long-term survival after resection for gastric and esophageal cancer. Surgery (United States). https://doi.org/10.1016/j.surg.2016.02.020
Lou F, Sima CS, Adusumilli PS et al (2013) Esophageal cancer recurrence patterns and implications for surveillance. J Thorac Oncol. https://doi.org/10.1097/01.JTO.0000437420.38972.fb
Sudarshan M (2019) Locoregional and oligometastatic recurrence of esophageal cancer-what are the management strategies? J Thorac Dis. https://doi.org/10.21037/jtd.2019.06.76
Katayama A, Mafune K, Tanaka Y, Takubo K, Makuuchi M, Kaminishi M (2003) Autopsy findings in patients after curative esophagectomy for esophageal carcinoma. J Am Coll Surg. https://doi.org/10.1016/S1072-7515(03)00116-9
Kang CH, Hwang Y, Lee HJ, Park IK, Kim YT (2016) Risk factors for local recurrence and optimal length of esophagectomy in esophageal squamous cell carcinoma. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2016.03.117
Lagarde SM, De Boer JD, Ten Kate FJW, Busch ORC, Obertop H, Van Lanschot JJB (2008) Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death due to recurrence. Ann Surg. https://doi.org/10.1097/SLA.0b013e31815b695e
Vellayappan BA, Soon YY, Ku GY, Leong CN, Lu JJ, Tey JC (2017) Chemoradiotherapy versus chemoradiotherapy plus surgery for esophageal cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010511.pub2
Markar SR, Johar A, Maisey N, Lagergren P, Lagergren J (2018) Complications during neoadjuvant therapy and prognosis following surgery for esophageal cancer. Dis Esophagus. https://doi.org/10.1093/dote/dox151
Piessen G, Messager M, Mirabel X et al (2013) Is there a role for surgery for patients with a complete clinical response after chemoradiation for esophageal cancer? An intention-to-treat case-control study. Ann Surg. https://doi.org/10.1097/SLA.0000000000000228
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Santiago Horgan is a consultant for Stryker Corporation, Intuitive Surgical, Fortimedix Surgical, and Medtronic. Dr. Jacobsen receives a teaching honorarium from Gore Medical. Dr. Sandler is a consultant for Intuitive Surgical and Boston Scientific. Dr. Onaitis is a consultant for Intuitive Surgical. Dr. Bouvet is a consultant for Stryker Corporation. Drs. Broderick, Lee, Zhao, Blitzer, Lam, Cheverie, and Kelly have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Broderick, R.C., Lee, A.M., Blitzer, R.R. et al. It’s not always too late: a case for minimally invasive salvage esophagectomy. Surg Endosc 35, 4700–4711 (2021). https://doi.org/10.1007/s00464-020-07937-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07937-2