Abstract
Background
Laparoscopic skill acquisition involves a steep learning curve and laparoscopic suturing is an exceptionally challenging task. By improving the way feedback is given, trainees can learn these skills more effectively. This study aims to establish the most effective form of structured feedback on laparoscopic suturing skill acquisition in novices, by comparing the effects of expert verbal feedback, video review with expert feedback (video feedback), and video review with self-assessment.
Methods
A prospective randomized blinded trial comparing verbal feedback, video feedback, and self-assessment. Novices in laparoscopic surgery were tasked with performing laparoscopic suturing with intracorporeal knot tying. Time was given for practice, and pre- and post-feedback assessments were undertaken. Suturing performance was measured using a task-specific checklist and global ratings. A post-study questionnaire was used to measure participant-perceived confidence, knowledge, and experience levels.
Results
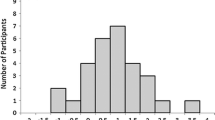
Fifty-one participants were randomized and allocated equally into the three groups. Performance in all three groups improved significantly from baseline. Video feedback had the largest improvement margin with checklist and global score improvements of 17.1% (± 9.9%) and 14.7% (± 9.3%), respectively. Performance improvements between groups were statistically significant in the global components (p = 0.004) but not the checklist components (p = 0.186). Global score improvement was significantly better in the video feedback group but was statistically insignificant between the self-assessment and verbal feedback groups. Questionnaire responses demonstrated positive results in confidence, knowledge, and experience levels, across all three study groups, with no differences between the groups (p > 0.05).
Conclusion
Structured video feedback facilitates reflection and self-directed learning, which improves the ability to develop proficiency in surgical skills. Combining both self-assessment and video feedback may be beneficial over verbal feedback alone due to the advantages of video review. These techniques should therefore be considered for implementation into surgical education curricula.



Similar content being viewed by others
References
Palter VN, Orzech N, Aggarwal R et al (2010) Resident perceptions of advanced laparoscopic skills training. Surg Endosc 24:2830–2834. https://doi.org/10.1007/s00464-010-1058-2
Mattar SG, Alseidi AA, Jones DB et al (2013) General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 258:440–447. https://doi.org/10.1097/SLA.0b013e3182a191ca
Enani G, Watanabe Y, McKendy KM et al (2017) What are the training gaps for acquiring laparoscopic suturing skills? J Surg Educ 74:656–662. https://doi.org/10.1016/j.jsurg.2016.12.004
Dowell D, Kunins HV, Farley TA (2013) Opioid analgesics—risky drugs, not risky patients. JAMA. https://doi.org/10.1001/jama.2013.5794
ACGME (2019) ACGME Program Requirements for Graduate Medical Education in General Surgery. In: ACGME Website. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/440_GeneralSurgery_2019.pdf?ver=2019–06–19–092818–273. Accessed 21 Mar 2020
Cope AC, Mavroveli S, Bezemer J et al (2015) Making meaning from sensory cues: a qualitative investigation of postgraduate learning in the operating room. Acad Med 90:1125–1131. https://doi.org/10.1097/ACM.0000000000000740
Aiken CA, Fairbrother JT, Post PG (2012) The effects of self-controlled video feedback on the learning of the basketball set shot. Front Psychol 3:338. https://doi.org/10.3389/fpsyg.2012.00338
Kelley H, Miltenberger RG (2016) Using video feedback to improve horseback-riding skills. J Appl Behav Anal 49:138–147. https://doi.org/10.1002/jaba.272
Boucher M, Creech A, Dubé F (2019) Video feedback and the self-evaluation of college-level guitarists during individual practice. Psychol Music. https://doi.org/10.1177/0305735619842374
Schmidt J, Fleming J, Ownsworth T, Lannin NA (2013) Video feedback on functional task performance improves self-awareness after traumatic brain injury: a randomized controlled trial. Neurorehabil Neural Repair 27:316–324. https://doi.org/10.1177/1545968312469838
James DM, Hall A, Lombardo C, Mcgovern W (2016) A video feedback intervention for workforce development: exploring staff perspective using longitudinal qualitative methodology. J Appl Res Intellect Disabil 29:111–123. https://doi.org/10.1111/jar.12161
Backstein D, Agnidis Z, Regehr G, Reznick R (2004) The effectiveness of video feedback in the acquisition of orthopedic technical skills. Am J Surg 187:427–432. https://doi.org/10.1016/j.amjsurg.2003.12.011
Backstein D, Agnidis Z, Sadhu R, MacRae H (2005) Effectiveness of repeated video feedback in the acquisition of a surgical technical skill. Can J Surg 48(3):195–200. https://canjsurg.ca/vol48-issue3/48-3-195/. Accessed 23 Mar 2020
Farquharson AL, Cresswell AC, Beard JD, Chan P (2013) Randomized trial of the effect of video feedback on the acquisition of surgical skills. Br J Surg 100:1448–1453. https://doi.org/10.1002/bjs.9237
Singh P, Aggarwal R, Tahir M et al (2015) A randomized controlled study to evaluate the role of video-based coaching in training laparoscopic skills. Ann Surg 261:862–869. https://doi.org/10.1097/SLA.0000000000000857
Rindos NB, Wroble-Biglan M, Ecker A et al (2017) Impact of video coaching on gynecologic resident laparoscopic suturing: a randomized controlled trial. J Minim Invasive Gynecol 24:426–431. https://doi.org/10.1016/j.jmig.2016.12.020
Jamshidi R, LaMasters T, Eisenberg D et al (2009) Video self-assessment augments development of videoscopic suturing skill. J Am Coll Surg 209:622–625. https://doi.org/10.1016/j.jamcollsurg.2009.07.024
Nesbitt CI, Phillips AW, Searle RF, Stansby G (2015) Randomized trial to assess the effect of supervised and unsupervised video feedback on teaching practical skills. J Surg Educ 72:697–703. https://doi.org/10.1016/j.jsurg.2014.12.013
Alameddine MB, Englesbe MJ, Waits SA (2018) A video-based coaching intervention to improve surgical skill in fourth-year medical students. J Surg Educ 75:1475–1479. https://doi.org/10.1016/j.jsurg.2018.04.003
Rizan C, Ansell J, Tilston TW et al (2015) Are general surgeons able to accurately self-assess their level of technical skills? Ann R Coll Surg Engl 97:549–555. https://doi.org/10.1308/rcsann.2015.0024
Bandura A (1982) Self-efficacy mechanism in human agency. Am Psychol 37:122–147. https://doi.org/10.1037/0003-066X.37.2.122
MacDonald J, Williams RG, Rogers DA (2003) Self-assessment in simulation-based surgical skills training. Am J Surg 185:319–322. https://doi.org/10.1016/S0002-9610(02)01420-4
Arora S, Miskovic D, Hull L et al (2011) Self vs expert assessment of technical and non-technical skills in high fidelity simulation. Am J Surg 202:500–506. https://doi.org/10.1016/j.amjsurg.2011.01.024
Ganni S, Chmarra MK, Goossens RHM, Jakimowicz JJ (2017) Self-assessment in laparoscopic surgical skills training: Is it reliable? Surg Endosc 31:2451–2456. https://doi.org/10.1007/s00464-016-5246-6
Farooq A, Reso A, Harvey A (2018) Instant replay: evaluation of instant video feedback in surgical novices for a laparoscopic gallbladder dissection. Am J Surg 215:943–947. https://doi.org/10.1016/j.amjsurg.2018.01.013
Ramani S, Könings KD, Ginsburg S, van der Vleuten CP (2019) Feedback redefined: principles and practice. J Gen Intern Med. https://doi.org/10.1007/s11606-019-04874-2
Chang OH, King LP, Modest AM, Hur HC (2016) Developing an objective structured assessment of technical skills for laparoscopic suturing and intracorporeal knot tying. J Surg Educ 73:258–263. https://doi.org/10.1016/j.jsurg.2015.10.006
Seymour NE, Gallagher AG, Roman SA et al (2002) Virtual reality training improves operating room performance. Ann Surg 236:458–464. https://doi.org/10.1097/00000658-200210000-00008
Ahmet A, Gamze K, Rustem M, Sezen KA (2018) Is video-based education an effective method in surgical education? a systematic review. J Surg Educ 75:1150–1158. https://doi.org/10.1016/j.jsurg.2018.01.014
Wanzel KR, Hamstra SJ, Caminiti MF et al (2003) Visual-spatial ability correlates with efficiency of hand motion and successful surgical performance. Surgery 134:750–757. https://doi.org/10.1016/S0039-6060(03)00248-4
Hedman L, Ström P, Andersson P et al (2006) High-level visual-spatial ability for novices correlates with performance in a visual-spatial complex surgical simulator task. Surg Endosc Other Interv Tech 20:1275–1280. https://doi.org/10.1007/s00464-005-0036-6
Quick JA, Kudav V, Doty J et al (2017) Surgical resident technical skill self-evaluation: increased precision with training progression. J Surg Res 218:144–149. https://doi.org/10.1016/j.jss.2017.05.070
Alaraimi B, El Bakbak W, Sarker S et al (2014) A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg 38:2746–2752. https://doi.org/10.1007/s00268-014-2674-0
Leijte E, de Blaauw I, Van Workum F et al (2019) Robot assisted versus laparoscopic suturing learning curve in a simulated setting. Surg Endosc. https://doi.org/10.1007/s00464-019-07263-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jonathan Halim, Joshua Jelley, Ningning Zhang, Marcus Ornstein, and Bijendra Patel have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Halim, J., Jelley, J., Zhang, N. et al. The effect of verbal feedback, video feedback, and self-assessment on laparoscopic intracorporeal suturing skills in novices: a randomized trial. Surg Endosc 35, 3787–3795 (2021). https://doi.org/10.1007/s00464-020-07871-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07871-3