Abstract
Background
Aim of the present systematic review is to compare the postoperative outcomes after minimally invasive anterior and posterior component separation technique (CST), in terms of postoperative morbidity and recurrence rates.
Methods
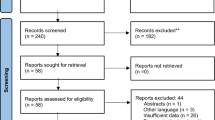
Nine-hundred and fifty-nine articles were identified through Pubmed database. Of these, 444 were eliminated because were duplicates between the searches. Of the remaining 515 articles, 414 were excluded after screening title and abstract. One hundred and one articles were fully analysed, and 73 articles were further excluded, finally including 28 articles. Based on the surgical technique, three groups were created: Group A, endoscopic anterior CST and closure of the abdominal midline by laparotomy; Group B, endoscopic anterior CST and closure of the abdominal midline laparoscopically or robotically; Group C, laparoscopic or robotic posterior CST with transversus abdominal muscle release (TAR).
Results
In group A, B and C, 196, 120 and 236 patients were included, respectively. Surgical and medical complication rates for the three groups were 31.2% and 13.7% in group A, 15.8% and 4.1% in group B, and 17.8% and 25.4% in group C, while recurrence rate was 10.7%, 6.6% and 0.4%, respectively. Statistically significant differences were observed in terms of surgical postoperative complication rate between group A versus B (p = 0.0022) and between group A versus C (p = 0.0015) and of recurrence rate between group A versus C (p = < 0.0001) and B versus C (p = 0.0009).
Conclusions
Anterior CST with midline closure by laparotomy showed the worst results in terms of postoperative surgical complications and recurrence in comparison to the pure minimally anterior and posterior CST. Posterior CST-TAR showed lowest hospital stay and recurrence rate, although the follow-up is short. However, due to the poor quality of most of the studies, further prospective studies and randomized control trials, with wider sample size and longer follow-up are required to demonstrate which is the best surgical option.

Similar content being viewed by others
References
Switzer NJ, Dykstra MA, Gill RS, Lim S, Lester E, de Gara C, Shi X, Birch DW, Karmali S (2015) Endoscopic versus open component separation: systematic review and meta-analysis. Surg Endosc 29(4):787–795. https://doi.org/10.1007/s00464-014-3741-1
Hodgkinson JD, Leo CA, Maeda Y, Bassett P, Oke SM, Vaizey CJ, Warusavitarne J (2018) A meta-analysis comparing open anterior component separation with posterior component separation and transversus abdominis release in the repair of midline ventral hernias. Hernia 22(4):617–626. https://doi.org/10.1007/s10029-018-1757-5
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86(3):519–526
Feretis M, Orchard P (2015) Minimally invasive component separation techniques in complex ventral abdominal hernia repair: a systematic review of the literature. Surg Laparosc Endosc Percutan Tech 25(2):100–105. https://doi.org/10.1097/sle.0000000000000114
Tong WM, Hope W, Overby DW, Hultman CS (2011) Comparison of outcome after mesh-only repair, laparoscopic component separation, and open component separation. Ann Plast Surg 66(5):551–556. https://doi.org/10.1097/sap.0b013e31820b3c91
Joels CS, Vanderveer AS, Newcomb WL, Lincourt AE, Polhill JL, Jacobs DG, Sing RF, Heniford BT (2006) Abdominal wall reconstruction after temporary abdominal closure: a ten-year review. Surg Innov 13(4):223–230
Lowe JB, Garza JR, Bowman JL, Rohrich RJ, Strodel WE (2000) Endoscopically assisted “components separation” for closure of abdominal wall defects. Plast Reconstr Surg 105(2):720–729 quiz 730
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ (2012) Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204(5):709–716. https://doi.org/10.1016/j.amjsurg.2012.02.008
Winder JS, Lyn-Sue J, Kunselman AR, Pauli EM (2017) Differences in midline fascial forces exist following laparoscopic and open transversus abdominis release in a porcine model. Surg Endosc 31(2):829–836. https://doi.org/10.1007/s00464-016-5040-5
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Lo CK, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45. https://doi.org/10.1186/1471-2288-14-45
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Rosen MJ, Jin J, McGee MF, Williams C, Marks J, Ponsky JL (2007) Laparoscopic component separation in the single-stage treatment of infected abdominal wall prosthetic removal. Hernia 11(5):435–440
Bachman SL, Ramaswamy A, Ramshaw BJ (2009) Early results of midline hernia repair using a minimally invasive component separation technique. Am Surg 75(7):572–577 (discussion 577–578)
Cox TC, Pearl JP, Ritter EM (2010) Rives-Stoppa incisional hernia repair combined with laparoscopic separation of abdominal wall components: a novel approach to complex abdominal wall closure. Hernia 14(6):561–567. https://doi.org/10.1007/s10029-010-0704-x
Albright E, Diaz D, Davenport D, Roth JS (2011) The component separation technique for hernia repair: a comparison of open and endoscopic techniques. Am Surg 77(7):839–843
Azoury SC, Dhanasopon AP, Hui X, Tuffaha SH, De La Cruz C, Liao C, Lovins M, Nguyen HT (2014) Endoscopic component separation for laparoscopic and open ventral hernia repair: a single institutional comparison of outcomes and review of the technique. Hernia 18(5):637–645. https://doi.org/10.1007/s10029-014-1274-0
Ng N, Wampler M, Palladino H, Agullo F, Davis BR (2015) Outcomes of laparoscopic versus open fascial component separation for complex ventral hernia repair. Am Surg 81(7):714–719
Mommers EH, Wegdam JA, Nienhuijs SW, de Vries Reilingh TS (2016) How to perform the endoscopically assisted components separation technique (ECST) for large ventral hernia repair. Hernia 20(3):441–447. https://doi.org/10.1007/s10029-016-1485-7
Thomsen CØ, Brøndum TL, Jørgensen LN (2016) Quality of life after ventral hernia repair with endoscopic component separation technique. Scand J Surg 105(1):11–16. https://doi.org/10.1177/1457496915571402
Dauser B, Ghaffari S, Ng C, Schmid T, Köhler G, Herbst F (2017) Endoscopic anterior component separation: a novel technical approach. Hernia 21(6):951–955. https://doi.org/10.1007/s10029-017-1671-2
Muse TO, Zwischenberger BA, Miller MT, Borman DA, Davenport DL, Roth JS (2018) Outcomes after ventral hernia repair using the rives-stoppa, endoscopic, and open component separation techniques. Am Surg 84(3):433–437
Köhler G, Fischer I, Kaltenböck R, Lechner M, Dauser B, Jorgensen LN (2018) Evolution of endoscopic anterior component separation to a precostal access with a new cylindrical balloon trocar. J Laparoendosc Adv Surg Tech A 28(6):730–735. https://doi.org/10.1089/lap.2017.0480
Malik K, Bowers SP, Smith CD, Asbun H, Preissler S (2009) A case series of laparoscopic components separation and rectus medialization with laparoscopic ventral hernia repair. J Laparoendosc Adv Surg Tech A 19(5):607–610. https://doi.org/10.1089/lap.2009.0155
Giurgius M, Bendure L, Davenport DL, Roth JS (2012) The endoscopic component separation technique for hernia repair results in reduced morbidity compared to the open component separation technique. Hernia 16(1):47–51. https://doi.org/10.1007/s10029-011-0866-1
Moazzez A, Mason RJ, Darehzereshki A, Katkhouda N (2013) Totally laparoscopic abdominal wall reconstruction: lessons learned and results of a short-term follow-up. Hernia 17(5):633–638. https://doi.org/10.1007/s10029-013-1145-0
Fox M, Cannon RM, Egger M, Spate K, Kehdy FJ (2013) Laparoscopic component separation reduces postoperative wound complications but does not alter recurrence rates in complex hernia repairs. Am J Surg 206(6):869–874 (discussion 874–875). https://doi.org/10.1016/j.amjsurg.2013.08.005
Oviedo RJ, Robertson JC, Desai AS (2017) Robotic ventral hernia repair and endoscopic component separation: outcomes. JSLS. https://doi.org/10.4293/jsls.2017.00055
Wiessner R, Vorwerk T, Tolla-Jensen C, Gehring A (2017) Continuous laparoscopic closure of the linea alba with barbed sutures combined with laparoscopic mesh implantation (IPOM plus repair) as a new technique for treatment of abdominal hernias. Front Surg 4:62. https://doi.org/10.3389/fsurg.2017.00062
Elstner KE, Read JW, Jacombs ASW, Martins RT, Arduini F, Cosman PH, Rodriguez-Acevedo O, Dardano AN, Karatassas A, Ibrahim N (2018) Single port component separation: endoscopic external oblique release for complex ventral hernia repair. Surg Endosc 32(5):2474–2479. https://doi.org/10.1007/s00464-017-5949-3
Belyansky I, Zahiri HR, Park A (2016) Laparoscopic transversus abdominis release, a Novel minimally invasive approach to complex abdominal wall reconstruction. Surg Innov 23(2):134–141. https://doi.org/10.1177/1553350615618290
Moore AM, Anderson LN, Chen DC (2016) Laparoscopic stapled sublay repair with self-gripping mesh: a simplified technique for minimally invasive extraperitoneal ventral hernia repair. Surg Technol Int 29:131–139
Amaral MVFD, Guimarães JR, Volpe P, Oliveira FMM, Domene CE, Roll S, Cavazzola LT (2017) Robotic transversus abdominis release (TAR): is it possible to offer minimally invasive surgery for abdominal wall complex defects? Rev Col Bras Circ 44(2):216–219. https://doi.org/10.1590/0100-69912017002009
Bittner JG 4th, Alrefai S, Vy M, Mabe M, Del Prado PAR, Clingempeel NL (2018) Comparative analysis of open and robotic transversus abdominis release for ventral hernia repair. Surg Endosc 32(2):727–734. https://doi.org/10.1007/s00464-017-5729-0
Martin-Del-Campo LA, Weltz AS, Belyansky I, Novitsky YW (2018) Comparative analysis of perioperative outcomes of robotic versus open transversus abdominis release. Surg Endosc 32(2):840–845. https://doi.org/10.1007/s00464-017-5752-1
Halka JT, Vasyluk A, DeMare AM, Janczyk RJ, Iacco AA (2018) Robotic and hybrid robotic transversus abdominis release may be performed with low length of stay and wound morbidity. Am J Surg 215(3):462–465. https://doi.org/10.1016/j.amjsurg.2017.10.053
Belyansky I, Reza Zahiri H, Sanford Z, Weltz AS, Park A (2018) Early operative outcomes of endoscopic (eTEP access) robotic-assisted retromuscular abdominal wall hernia repair. Hernia 22(5):837–847. https://doi.org/10.1007/s10029-018-1795-z
Halpern DK, Howell RS, Boinpally H, Magadan-Alvarez C, Petrone P, Brathwaite CEM (2019) Ascending the learning curve of robotic abdominal wall reconstruction. JSLS. https://doi.org/10.4293/jsls.2018.00084
Gokcal F, Morrison S, Kudsi OY (2019) Robotic retromuscular ventral hernia repair and transversus abdominis release: short-term outcomes and risk factors associated with perioperative complications. Hernia. https://doi.org/10.1007/s10029-019-01911-1
Onyekwelu I, Yakkanti R, Protzer L, Pinkston CM, Tucker C, Seligson D (2017) Surgical wound classification and surgical site infections in the orthopaedic patient. J Am Acad Orthop Surg Glob Res Rev 1(3):e022. https://doi.org/10.5435/jaaosglobal-d-17-00022
Harth KC, Rosen MJ (2010) Endoscopic versus open component separation in complex abdominal wall reconstruction. Am J Surg 199(3):342–346 (discussion 346–347). https://doi.org/10.1016/j.amjsurg.2009.09.015
Kurmann A, Visth E, Candinas D, Beldi G (2011) Long-term follow-up of open and laparoscopic repair of large incisional hernias. World J Surg 35(2):297–301. https://doi.org/10.1007/s00268-010-0874-9
Denney B, de la Torre JI (2017) Multipoint suture fixation technique for abdominal wall reconstruction with component separation and onlay biological mesh placement. Am Surg 83(5):515–521
Razavi SA, Desai KA, Hart AM, Thompson PW, Losken A (2018) The impact of mesh reinforcement with components separation for abdominal wall reconstruction. Am Surg 84(6):959–962
Cornette B, De Bacquer D, Berrevoet F (2018) Component separation technique for giant incisional hernia: a systematic review. Am J Surg 215(4):719–726. https://doi.org/10.1016/j.amjsurg.2017.07.032
Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ (2012) Posterior and open anterior components separations: a comparative analysis. Am J Surg 203(3):318–322 (discussion 322). https://doi.org/10.1016/j.amjsurg.2011.10.009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Andrea Balla, Dr. Isaias Alarcón and Prof. Salvador Morales-Conde declare that they have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balla, A., Alarcón, I. & Morales-Conde, S. Minimally invasive component separation technique for large ventral hernia: which is the best choice? A systematic literature review. Surg Endosc 34, 14–30 (2020). https://doi.org/10.1007/s00464-019-07156-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07156-4