Abstract
Background
Accelerated bone loss is a known complication after bariatric surgery. Bone mineral density has been shown to decrease significantly after Laparoscopic Roux-en-Y gastric bypass (RYGB). Laparoscopic sleeve gastrectomy (SG) effects on bone density are largely unknown. This should be considered for those with increased preoperative risk for bone loss, such as postmenopausal females.
Methods
This prospective clinical trial included postmenopausal patients, with BMI ≥ 35 k/m2, being evaluated for either RYGB or SG. Patients with history of osteoporosis, estrogen hormone replacement therapy, active smoking, glucocorticoid use, or weight > 295 lb were excluded. Patients underwent DEXA scans preoperatively and 1 year postoperatively with measurement of total body bone mineral density (BMD) and bone mineral content (BMC) as well as regional site-specific BMD and BMC.
Results
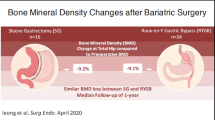
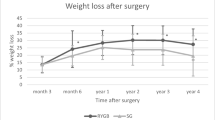
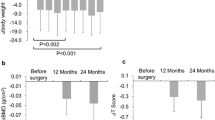
A total of 28 patients were enrolled. 16 (57.1%) patients underwent RYGB and 12 (42.9%) patients underwent SG. Median preoperative BMI was 44.2 k/m2 (IQR 39.9, 46.6). Median change in BMI at 12 months was − 11.3 k/m2 (IQR − 12.8, − 7.9). A significant reduction in total body BMC was seen when comparing preoperative measurements to postoperative measurements (2358.32 vs 2280.68 grams; p = 0.002). Regional site BMC and BMD significantly decreased in the ribs and spine postoperatively (p = < 0.02) representing the greatest loss in the axial skeleton. Comparing those who underwent RYGB to SG there was no significant difference between the two groups when evaluating changes in total or regional site BMD.
Conclusion
Postmenopausal women were found to have decreased BMD and BMC after RYGB and SG, suggesting that high-risk women may benefit from postoperative DEXA screening. Further study is needed to determine the clinical significance of these findings. It is unknown if these changes in BMD are due to modifiable factors (Vitamin D level, activity level, hormone status, etc.), and whether BMD and BMC is recovered beyond 1 year.
Similar content being viewed by others
References
Versteegden DPA, Van Himbeeck MJJ, Nienhuijs SW (2018) Improvement in quality of life after bariatric surgery: sleeve versus bypass. Surg Obes Relat Dis 14:170–174
Umeda LM, Silva EA, Carneiro G, Arasaki CH, Geloneze B, Zanella MT (2011) Early improvement in glycemic control after bariatric surgery and its relationships with insulin, GLP-1, and glucagon secretion in type 2 diabetic patients. Obes Surg 21:896–901
Gutierrez-Blanco D, Romero Funes D, Matute C, Ganga R, Lo Menzo E, Szomstein S, Rosenthal RJ (2018) A119—can surgical weight loss reduce the risk of developing coronary heart disease? Surg Obes Relat Dis 14:S13
Albala C, Yanez M, Devoto E, Sostin C, Zeballos L, Santos JL (1996) Obesity as a protective factor for postmenopausal osteoporosis. Int J Obes Relat Metab Disord 20:1027–1032
von Mach MA, Stoeckli R, Bilz S, Kraenzlin M, Langer I, Keller U (2004) Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism 53:918–921
Tsiftsis DD, Mylonas P, Mead N, Kalfarentzos F, Alexandrides TK (2009) Bone mass decreases in morbidly obese women after long limb-biliopancreatic diversion and marked weight loss without secondary hyperparathyroidism. A physiological adaptation to weight loss? Obes Surg 19:1497–1503
Vilarrasa N, Gomez JM, Elio I, Gomez-Vaquero C, Masdevall C, Pujol J, Virgili N, Burgos R, Sanchez-Santos R, de Gordejuela AG, Soler J (2009) Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg 19:860–866
Scibora LM, Ikramuddin S, Buchwald H, Petit MA (2012) Examining the link between bariatric surgery, bone loss, and osteoporosis: a review of bone density studies. Obes Surg 22:654–667
Compston JE, Horton LW, Laker MF, Ayers AB, Woodhead JS, Bull HJ, Gazet JC, Pilkington TR (1978) Bone disease after jejuno-ileal bypass for obesity. Lancet 2:1–4
Fleischer J, Stein EM, Bessler M, Della Badia M, Restuccia N, Olivero-Rivera L, McMahon DJ, Silverberg SJ (2008) The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab 93:3735–3740
ASMBS (2018) Estimate of Bariatric Surgery Numbers, 2011–2017. Available at: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed 18 Feb 2019
Nogues X, Goday A, Pena MJ, Benaiges D, de Ramon M, Crous X, Vial M, Pera M, Grande L, Diez-Perez A, Ramon JM (2010) Bone mass loss after sleeve gastrectomy: a prospective comparative study with gastric bypass. Cir Esp 88:103–109
Adamczyk P, Buzga M, Holeczy P, Svagera Z, Smajstrla V, Zonca P, Pluskiewicz W (2015) Bone mineral density and body composition after laparoscopic sleeve gastrectomy in men: a short-term longitudinal study. Int J Surg 23:101–107
Bredella MA, Greenblatt LB, Eajazi A, Torriani M, Yu EW (2017) Effects of Roux-en-Y gastric bypass and sleeve gastrectomy on bone mineral density and marrow adipose tissue. Bone 95:85–90
Pontiroli AE, Ceriani V, Sarro G, Micheletto G, Giovanelli A, Zakaria AS, Fanchini M, Osio C, Nosari I, Veronelli AM, Folli F (2018) Incidence of diabetes mellitus, cardiovascular diseases, and cancer in patients undergoing malabsorptive surgery (biliopancreatic diversion and biliointestinal bypass) vs medical treatment. Obes Surg 29:935–942
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Pontiroli AE, Zakaria AS, Fanchini M, Osio C, Tagliabue E, Micheletto G, Saibene A, Folli F (2018) A 23-year study of mortality and development of co-morbidities in patients with obesity undergoing bariatric surgery (laparoscopic gastric banding) in comparison with medical treatment of obesity. Cardiovasc Diabetol 17:161
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, Lamonte MJ, Stroup AM, Hunt SC (2007) Long-term mortality after gastric bypass surgery. N Engl J Med 357:753–761
Wucher H, Ciangura C, Poitou C, Czernichow S (2008) Effects of weight loss on bone status after bariatric surgery: association between adipokines and bone markers. Obes Surg 18:58–65
Schollenberger AE, Heinze JM, Meile T, Peter A, Konigsrainer A, Bischoff SC (2015) Markers of bone metabolism in obese individuals undergoing laparoscopic sleeve gastrectomy. Obes Surg 25:1439–1445
Wang X, Li L, Zhu C, Gao J, Qu S (2018) Alteration of bone mineral density differs between genders in obese subjects after laparoscopic sleeve gastrectomy: bone morphogenetic protein 4 may count. Obes Surg 28:3221–3226
Zalesin KC, Franklin BA, Lillystone MA, Shamoun T, Krause KR, Chengelis DL, Mucci SJ, Shaheen KW, McCullough PA (2010) Differential loss of fat and lean mass in the morbidly obese after bariatric surgery. Metab Syndr Relat Disord 8:15–20
Hsin MC, Huang CK, Tai CM, Yeh LR, Kuo HC, Garg A (2015) A case-matched study of the differences in bone mineral density 1 year after 3 different bariatric procedures. Surg Obes Relat Dis 11:181–185
Johnson JM, Maher JW, Samuel I, Heitshusen D, Doherty C, Downs RW (2005) Effects of gastric bypass procedures on bone mineral density, calcium, parathyroid hormone, and vitamin D. J Gastrointest Surg 9:1106–1110; (discussion 1110–1101)
Goode LR, Brolin RE, Chowdhury HA, Shapses SA (2004) Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res 12:40–47
Carrasco F, Ruz M, Rojas P, Csendes A, Rebolledo A, Codoceo J, Inostroza J, Basfi-Fer K, Papapietro K, Rojas J, Pizarro F, Olivares M (2009) Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg 19:41–46
Douchi T, Yamamoto S, Oki T, Maruta K, Kuwahata R, Yamasaki H, Nagata Y (2000) Difference in the effect of adiposity on bone density between pre- and postmenopausal women. Maturitas 34:261–266
Ricci TA, Heymsfield SB, Pierson RN Jr, Stahl T, Chowdhury HA, Shapses SA (2001) Moderate energy restriction increases bone resorption in obese postmenopausal women. Am J Clin Nutr 73:347–352
Knapp KM, Welsman JR, Hopkins SJ, Shallcross A, Fogelman I, Blake GM (2015) Obesity increases precision errors in total body dual-energy x-ray absorptiometry measurements. J Clin Densitom 18:209–216
Acknowledgements
This study was funded by a SAGES research grant awarded by the SAGES research and career development committee.
Funding
Research support through the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Foundation Award, granted in 2013. The Duke BERD Methods Core’s support of this project was made possible (in part) by Grant Number UL1TR002553 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCATS or NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Alfredo D. Guerron is an advisor for Levita and Phenomix, speaker for Gore and Medtronic, and proctor for Biom’up. Dr. Dana Portenier is and advisor for Medtronic, consultant for Medtronic and Intuitive, and speaker for Teleflex, Gore, Medtronic and Levita. Dr. Jin Yoo is a consultant for Gore, Medtronic and Novadaq, and a speaker for Teleflex, Stryker, Gore, Medtronic and Novadaq. Dr. Chan Park is a consultant for Gore and Teleflex. Dr. Andrew R Luhrs, Dr. Gerardo Davalos, Mr. Reginald Lerebours, Dr. Lawrence Tabone, Dr. Philip Omotosho, and Dr. Alfonso Torquati have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luhrs, A.R., Davalos, G., Lerebours, R. et al. Determining changes in bone metabolism after bariatric surgery in postmenopausal women. Surg Endosc 34, 1754–1760 (2020). https://doi.org/10.1007/s00464-019-06922-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06922-8